Abstract
Purpose
To evaluate the effect of female reproductive age on oocyte cryo-survival, fertilization and the subsequent embryonic development following vitrification using the mouse model in order to address the question of how maternal reproductive age is related to fertility preservation.
Methods
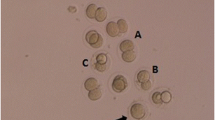
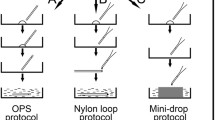
Oocytes were collected from mice of different reproductive age: (1) 8–10 weeks, (2) 16–20 weeks, (3) 32–36 weeks, and (4) 44–48 weeks. Following vitrification and warming, the oocytes in each group were assessed for cryo-survival, fertilization and embryonic development as well as for the quality of blastocysts. Fresh oocytes without undergoing vitrification were used in each age group as controls.
Results
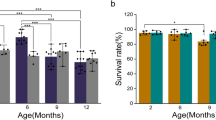
The mean number of oocytes retrieved following superovulation was found to reduce significantly (P < 0.05) in mice from 32–36 weeks of age (18.1 ± 8.5) compared with 8–10 weeks of age (26.8 ± 9.8) and 16–20 weeks of age (23.9 ± 4.2) respectively. The cryo-survival rate of oocytes was reduced significantly (P < 0.05) in mice of 44–48 weeks of age (90.4% ± 7.9) compared with the other 3 groups (98.8% ± 2.1, 98.0% ± 3.3 and 98.5% ± 2.2, respectively). The cleavage rate of vitrified oocytes declined significantly following the increase in maternal age in mice of 32–36 weeks of age (69.7% ± 20.8) forward (63.6% ± 9.2). However, no significant difference in the cleavage rate was found among the control groups of different maternal ages. The rate of embryo development to the blastocyst stage in the vitrified oocytes also significantly declined following the increase in maternal age (71.8% ± 8.8, 66.4% ± 10.7, 64.2% ± 17.4 and 4.1% ± 8.3 respectively). There were no such differences in the rates of embryo development to the blastocyst stage among the control groups following the increase in maternal age (75.9% ± 12.2, 79.5% ± 28.9, 70.2% ± 17.4 and 69.3% ± 19.0 respectively). However, the quality of blastocysts produced from 32–36 weeks and 44–48 weeks of ages was significantly poor in term of total cell numbers and the ratio of inner cell mass(ICM) / trophectoderm (TE) compared to younger age in both vitrified and control groups
Conclusions
Cryo-survival of oocytes following vitrification and warming procedures is associated with female reproductive age. There is a more negative impact on the oocytes following vitrification and warming with the increase of maternal age.
Similar content being viewed by others
References
van Noord-Zaadstra BM, Looman CW, Alsbach H, Habbema JD, te Velde ER, Karbaat J. Delaying childbearing: effect of age on fecundity and outcome of pregnancy. BMJ. 1991;302:1361–5.
Ottolenghi C, Uda M, Hamatani T, Crisponi L, Garcia JE, Ko M, et al. Aging of oocyte, ovary, and human reproduction. Ann NY Acad Sci. 2004;1034:117–31.
Armstrong DT. Effects of maternal age on oocyte developmental competence. Theriogenology. 2001;55:1303–22.
Klein J, Sauer MV. Assessing fertility in women of advanced reproductive age. Am J Obstet Gynecol. 2001;185:758–70.
Schwartz D, Mayaux MJ. Female fecundity as a function of age: results of artificial insemination in 2193 nulliparous women with azoospermic husbands. Federation CECOS. N Engl J Med. 1982;306:404–6.
van Kooij RJ, Looman CW, Habbema JD, Dorland M, te Velde ER. Age-dependent decrease in embryo implantation rate after in vitro fertilization. Fertil Steril. 1996;66:769–75.
te Velde ER, Pearson PL. The variability of female reproductive ageing. Hum Reprod Update. 2002;8:141–54.
Navot D, Drews MR, Bergh PA, Guzman I, Karstaedt A, Scott Jr RT, et al. Age-related decline in female fertility is not due to diminished capacity of the uterus to sustain embryo implantation. Fertil Steril. 1994;61:97–101.
Navot D, Bergh PA, Williams MA, Garrisi GJ, Guzman I, Sandler B, et al. Poor oocyte quality rather than implantation failure as a cause of age-related decline in female fertility. Lancet. 1991;337:1375–7.
Volarcik K, Sheean L, Goldfarb J, Woods L, Abdul-Karim FW, Hunt P. The meiotic competence of in-vitro matured human oocytes is influenced by donor age: evidence that folliculogenesis is compromised in the reproductively aged ovary. Hum Reprod. 1998;13:154–60.
Krisher RL. The effect of oocyte quality on development. J Anim Sci. 2004;82(E-Suppl):E14–23.
Huang JY, Tulandi T, Holzer H, Tan SL, Chian RC. Combining ovarian tissue cryobanking with retrieval of immature oocytes followed by in vitro maturation and vitrification: an additional strategy of fertility preservation. Fertil Steril. 2008;89:567–72.
Oktay K, Cil AP, Bang H. Efficiency of oocyte cryopreservation: a meta-analysis. Fertil Steril. 2006;86:70–80.
Cobo A, Kuwayama M, Perez S, Ruiz A, Pellicer A, Remohi J. Comparison of concomitant outcome achieved with fresh and cryopreserved donor oocytes vitrified by the Cryotop method. Fertil Steril. 2008;89:1657–64.
Wei YH, Wu SB, Ma YS, Lee HC. Respiratory function decline and DNA mutation in mitochondria, oxidative stress and altered gene expression during aging. Chang Gung Med J. 2009;32:113–32.
Practice Committee of American Society for Reproductive Medicine, Practice Committee of Society for Assisted Reproductive Technology. Ovarian tissue and oocyte cryopreservation. Fertil Steril. 2008;90:S241–6.
Maher B. Little consensus on egg freezing. Nature. 2007;449:958.
Broekmans FJ, Knauff EA, te Velde ER, Macklon NS, Fauser BC. Female reproductive ageing: current knowledge and future trends. Trends Endocrinol Metab. 2007;18:58–65.
Mosher WD, Pratt WF. Fecundity and infertility in the United States: incidence and trends. Fertil Steril. 1991;56:192–3.
Huang JY, Chen HY, Park JY, Tan SL, Chian RC. Comparison of spindle and chromosome configuration in in vitro- and in vivo-matured mouse oocytes after vitrification. Fertil Steril. 2008;90:1424–32.
Kimura Y, Yanagimachi R. Intracytoplasmic sperm injection in the mouse. Biol Reprod. 1995;52:709–20.
Handyside AH, Hunter S. A rapid procedure for visualising the inner cell mass and trophectoderm nuclei of mouse blastocysts in situ using polynucleotide-specific fluorochromes. J Exp Zool. 1984;231:429–34.
Rugh R. The mouse. Its reproduction and development. Oxford University Press; 1990, P5.
Tarin JJ, Perez-Albala S, Cano A. Cellular and morphological traits of oocytes retrieved from aging mice after exogenous ovarian stimulation. Biol Reprod. 2001;65:141–50.
Lass A, Silye R, Abrams DC, Krausz T, Hovatta O, Margara R, et al. Follicular density in ovarian biopsy of infertile women: a novel method to assess ovarian reserve. Hum Reprod. 1997;12:1028–31.
Gosden RG, Laing SC, Felicio LS, Nelson JF, Finch CE. Imminent oocyte exhaustion and reduced follicular recruitment mark the transition to acyclicity in aging C57BL/6J mice. Biol Reprod. 1983;28:255–60.
Faddy MJ, Gosden RG. A mathematical model of follicle dynamics in the human ovary. Hum Reprod. 1995;10:770–5.
Levran D, Ben-Shlomo I, Dor J, Ben-Rafael Z, Nebel L, Mashiach S. Aging of endometrium and oocytes: observations on conception and abortion rates in an egg donation model. Fertil Steril. 1991;56:1091–4.
Balmaceda JP, Bernardini L, Ciuffardi I, Felix C, Ord T, Sueldo CE, et al. Oocyte donation in humans: a model to study the effect of age on embryo implantation rate. Hum Reprod. 1994;9:2160–3.
Faddy MJ, Gosden RG. A model conforming the decline in follicle numbers to the age of menopause in women. Hum Reprod. 1996;11:1484–6.
Munne S, Alikani M, Tomkin G, Grifo J, Cohen J. Embryo morphology, developmental rates, and maternal age are correlated with chromosome abnormalities. Fertil Steril. 1995;64:382–91.
Battaglia DE, Goodwin P, Klein NA, Soules MR. Influence of maternal age on meiotic spindle assembly in oocytes from naturally cycling women. Hum Reprod. 1996;11:2217–22.
Lopes FL, Fortier AL, Darricarrere N, Chan D, Arnold DR, Trasler JM. Reproductive and epigenetic outcomes associated with aging mouse oocytes. In: Hum Mol Genet, vol. 18; 2009: 2032–2044.
Wang Y, Ock SA, Chian RC. Effect of gonadotrophin stimulation on mouse oocyte quality and subsequent embryonic development in vitro. Reprod Biomed Online. 2006;12:304–14.
Fujino Y, Ozaki K, Yamamasu S, Ito F, Matsuoka I, Hayashi E, et al. DNA fragmentation of oocytes in aged mice. Hum Reprod. 1996;11:1480–3.
Bouquet M, Selva J, Auroux M. Cryopreservation of mouse oocytes: mutagenic effects in the embryo? Biol Reprod. 1993;49:764–9.
Men H, Monson RL, Parrish JJ, Rutledge JJ. Detection of DNA damage in bovine metaphase II oocytes resulting from cryopreservation. Mol Reprod Dev. 2003;64:245–50.
Stachowiak EM, Papis K, Kruszewski M, Iwanenko T, Bartlomiejczyk T, Modlinski JA. Comparison of the level(s) of DNA damage using Comet assay in bovine oocytes subjected to selected vitrification methods. Reprod Domest Anim. 2009;44:653–8.
Fuku E, Xia L, Downey BR. Ultrastructural changes in bovine oocytes cryopreserved by vitrification. Cryobiology. 1995;32:139–56.
Boonkusol D, Faisaikarm T, Dinnyes A, Kitiyanant Y. Effects of vitrification procedures on subsequent development and ultrastructure of in vitro-matured swamp buffalo (Bubalus bubalis) oocytes. Reprod Fertil Dev. 2007;19:383–91.
Gualtieri R, Iaccarino M, Mollo V, Prisco M, Iaccarino S, Talevi R. Slow cooling of human oocytes: ultrastructural injuries and apoptotic status. Fertil Steril. 2009;91:1023–34.
Rho GJ, Kim S, Yoo JG, Balasubramanian S, Lee HJ, Choe SY. Microtubulin configuration and mitochondrial distribution after ultra-rapid cooling of bovine oocytes. Mol Reprod Dev. 2002;63:464–70.
Valojerdi MR, Salehnia M. Developmental potential and ultrastructural injuries of metaphase II (MII) mouse oocytes after slow freezing or vitrification. J Assist Reprod Genet. 2005;22:119–27.
de Bruin JP, Dorland M, Spek ER, Posthuma G, van Haaften M, Looman CW, et al. Age-related changes in the ultrastructure of the resting follicle pool in human ovaries. Biol Reprod. 2004;70:419–24.
Parmegiani L, Cognigni GE, Bernardi S, Ciampaglia W, Pocognoli P, Filicori M. Birth of a baby conceived from frozen oocytes of a 40-year-old woman. Reprod Biomed Online. 2009;18:795–8.
Acknowledgments
Dr. J. Yan was supported by the China Scholarship Council (file No. 2008601206) with the State Scholarship Fund to pursue her studies in Canada. This research project was funded by the McGill Reproductive Center, McGill University Health Center (MUHC), Montreal, Canada
Author information
Authors and Affiliations
Corresponding authors
Additional information
Capsule
Reduction in fertilization rate and poor embryonic development following vitrification procedure has been found to be associated with increased reproductive age.
Rights and permissions
About this article
Cite this article
Yan, J., Suzuki, J., Yu, X. et al. Cryo-survival, fertilization and early embryonic development of vitrified oocytes derived from mice of different reproductive age. J Assist Reprod Genet 27, 605–611 (2010). https://doi.org/10.1007/s10815-010-9450-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-010-9450-3