Abstract
Purpose: DNA-damaging factors have been reported in patients that failed to achieve pregnancy after assisted reproductive technologies (ART). The hypothesis was that increased circulating cell-free DNA released by damaged cells could predict unfavorable conditions leading to failed ART treatment. The objective was to compare the relative concentrations of cell-free DNA in the luteal phase sera of nonpregnant versus pregnant patients.
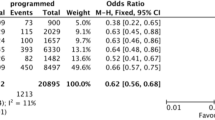
Methods: Frozen-thawed sera (30 IVF cases) were obtained 1 week after embryo transfer. There were 16 pregnant and 14 nonpregnant cases and controls consisting of male sera (n = 8 cases). Modified isocratic capillary electrophoresis was performed and the images analyzed for cell-free DNA.
Results: Circulating cell-free DNA were identified in the sera of all patients. The serum concentrations of high (12 kb) and low (1 kb) molecular weight cell-free DNA were similar for both nonpregnant and pregnant patients. Male control sera had higher cell-free DNA concentrations compared with females. Evaluation of sera from a control case showed no fluctuations in cell-free DNA concentrations throughout specific days of the menstrual cycle.
Conclusions: The results do not support the use of the luteal phase cell-free DNA concentration as a marker for failed pregnancies. The equal concentrations of high and low molecular weight cell-free DNA and ladder band-like gel patterns suggested cell apoptosis as the source of DNA.
Similar content being viewed by others
References
Chavez DJ, McIntyre JA: Sera from women with histories of repeated pregnancy losses cause abnormalities in peri-implantation blastocysts. J Reprod Immunol 1984;6:273–281
Oksenberg JR, Brautbar C: In vitro suppression of murine blastocysts growth by sera from women with reproductive disorders. Am J Reprod Immunol Microbiol 1986;11:118–124
Porter AJ, Singh SM, Jung JH: Evaluation of serum-associated embryotoxicity/mutagenicity in females with reproductive dysfunction using preimplantation mouse embryos in vitro. Mutagenesis 1988;3:403–408
Abir R, Zisman I, Ben Hur H, Yaffe P, Ornoy A: The effects of serum from women with miscarriages on the in vitro development of mouse preimplantation embryos. Acta Obstet Gynecol Scand 1990;69:27–33
Hill JA, Polgar K, Harlow BL, Anderson DJ: Evidence of embryo- and trophoblast-toxic cellular immune response(s) in women with recurrent spontaneous abortion. Am J Obstet Gynecol 1992;166:1044–1052
Dokras A, Sargent IL, Redman CWG, Barlow DH: Sera from women with unexplained infertility inhibit both mouse and human embryo growth in vitro. Fertil Steril 1993;60:285–292
Simon C, Frances A, Piquette GN, el Danasouri I, Zurawski G, Dang W, Polan ML: Embryonic implantation in mice is blocked by interleukin-1 receptor antagonist (IL-1ra). Endocrinology 1994;134:521–528
Thomason EJ, Roussev RG, Stern JJ, Coulam CB: Prevalence of embryotoxic factor in sera from women with unexplained recurrent abortion. Am J Reprod Immunol 1995;34:338–341
Fein A, Yacobovich R, Torchinsky A, Ben-Rafael Z, Carp H, Toder V: Evaluation of serum-associated embryotoxicity in women with reproductive disorders. J Assist Reprod Genetics 1995:12;305–311
Cameo M, Fontana V, Cameo P, Vauthay LG, Kaplan J, Tesone M: Similar embryotoxic effects of sera from infertile patients and exogenous interferon-γ on long-term in-vitro development of mouse embryos. Hum Reprod 1999;14:959–963
Jebelli B, Chan PJ, Corselli J, Patton WC, King A: Oocyte comet assay of luteal phase sera from non-pregnant patients after assisted reproductive procedures. J. Assist. Reprod. Genetics 2001;18:421–425
Dokras A, Sargent IL, Redman CWG, Barlow DH: Sera from women with unexplained infertility inhibit both mouse and human embryo growth in vitro. Fertil Steril 1993;60:285–292
Mandel P, Métais P: Les acides nucléiques du plasma sanguin chez l’homme. C.R. Acad Sci Paris 1948;142:241–243
Tan EM, Schur PH, Carr RI, Kunkel HG: Deoxyribonucleic acid (DNA) and antibodies to DNA in the serum of patients with systemic lupus erythematosus. J Clin Invest 1966;45:1732–1740
Leon SA, Shapiro B, Sklaroff DM, Yaros MJ: Free DNA in the serum of cancer patients and the effect of therapy. Cancer Res 1977;37:646–650
Fournie GJ, Courtin JP, Laval F, Chale JJ, Pourrat JP, Pujazon MC, Lauque D, Carles P: Plasma DNA as a marker of cancerous cell death. Investigations in patients suffering from lung cancer and in nude mice bearing human tumours. Cancer Lett. 1995;91:221–227
Rogers JC, Boldt D, Kornfeld S, Skinner A, Valeri CR: Excretion of deoxyribonucleic acid by lymphocytes stimulated with phytohemagglutinin or antigen. Proc Natl Acad Sci USA. 1972;69:1685–1689
Lo YM, Corbetta N, Chamberlain PF, Rai V, Sargent IL, Redman CW, Wainscoat JS: Presence of fetal DNA in maternal plasma and serum. Lancet. 1997;16:485–487
Lo YM, Tein MS, Lau TK, Haines CJ, Leung TN, Poon PM, Wainscoat JS, Johnson PJ, Chang AM, Hjelm NM: Quantitative analysis of fetal DNA in maternal plasma and serum: implications for noninvasive prenatal diagnosis. Am J Hum Genet 1998;62:768–775
Tsuda T, Nakagawa G, Sato M, Yagi K: Separation of nucleotides by high-voltage capillary electrophoresis. J Appl Biochem. 1983 AugOct;5(45):330–336
Kasper TJ, Melera M, Gozel P, Brownlee RG: Separation and detection of DNA by capillary electrophoresis. J Chromatogr. 1988 Dec 23;458:303–312
Cohen AS, Najarian DR, Paulus A, Guttman A, Smith JA, Karger BL: Rapid separation and purification of oligonucleotides by high-performance capillary gel electrophoresis. Proc Natl Acad Sci USA. 1988 Dec;85(24):9660–9663
Purdy JM: Methods for fertilization and embryo culture in vitro, in: Human Conception In Vitro (eds. RG Edwards and JM Purdy), Academic Press, London, 1982, pp 135–148
Wu TL, Zhang D, Chia JH, Tsao KH, Sun CF, Wu JT: Cell-free DNA: measurement in various carcinomas and establishment of normal reference range. Clin Chim Acta 2002;321:77–87
Kopreski MS, Benko FA, Kwee C, Leitzel KE, Eskander E, Lipton A, Gocke CD: Detection of mutant K-ras DNA in plasma or serum of patients with colorectal cancer. Br J Cancer 1997;76:1293–1299
Anker P, Lefort F, Vasioukhin V, Lyautey J, Lederrey C, Chen XQ, Stroun M, Mulcahy HE, Farthing MJ: K-ras mutations are found in DNA extracted from the plasma of patients with colorectal cancer. Gastroenterology 1997;112:1114–1120
Lee TH, Montalvo L, Chrebtow V, Busch MP: Quantitation of genomic DNA in plasma and serum samples: higher concentrations of genomic DNA found in serum than in plasma. Transfusion 2001;41:276–282
Holmgren L, Szeles A, Rajnavolgyi E, Folkman J, Klein G, Ernberg I, Falk KI: Horizontal transfer of DNA by the uptake of apoptotic bodies. Blood 1999;93:3956–3963
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hart, E.A., Patton, W.C., Jacobson, J.D. et al. Luteal phase serum cell-free DNA as a marker of failed pregnancy after assisted reproductive technology. J Assist Reprod Genet 22, 213–217 (2005). https://doi.org/10.1007/s10815-005-4924-4
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10815-005-4924-4