Abstract
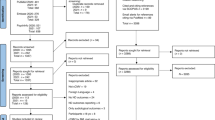
Association of congenital cytomegalovirus (CMV) infection with autism spectral disorder (ASD) has been suggested since 1980s. Despite the observed association, its role as a risk factor for ASD remains to be defined. In the present review, we systematically evaluated the available evidence associating congenital CMV infection with ASD using PubMed, Web of Science, Cochrane Library, and Embase databases. Any studies on children with CMV infection and ASD were evaluated for eligibility and three observational studies were included in meta-analysis. Although a high prevalence of congenital CMV infection in ASD cases (OR 11.31, 95% CI 3.07–41.66) was indicated, too few events (0–2 events) in all included studies imposed serious limitations. There is urgent need for further studies to clarify this issue.


Similar content being viewed by others
References
Abdallah, M. W., et al. (2012). Amniotic fluid chemokines and autism spectrum disorders: An exploratory study utilizing a Danish historic birth cohort. Brain Behavior and Immunity, 26(1), 170–176. https://doi.org/10.1016/j.bbi.2011.09.003.
Alford, C. A., Stagno, S., Pass, R. F., & Britt, W. J. (1990). Congenital and perinatal cytomegalovirus infections. Reviews of Infectious Diseases, 12(Suppl 7), S745–S753.
Aronsson, F., Lannebo, C., Paucar, M., Brask, J., Kristensson, K., & Karlsson, H. (2002). Persistence of viral RNA in the brain of offspring to mice infected with influenza A/WSN/33 virus during pregnancy. Journal of NeuroVirology, 8(4), 353–357. https://doi.org/10.1080/13550280290100480.
Baio, J. (2014). Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report, 63(2), 1–21.
Barbi, M., BINDA, S., Primache, V., Luraschi, C., & Corbetta, C. (1996). Diagnosis of congenital cytomegalovirus infection by detection of viral DNA in dried blood spots. Clinical and Diagnostic Virology, 6(1), 27–32.
Bilbo, S. D., & Schwarz, J. M. (2012). The immune system and developmental programming of brain and behavior. Frontiers in Neuroendocrinology, 33(3), 267–286. https://doi.org/10.1016/j.yfrne.2012.08.006.
Bilder, D., Pinborough-Zimmerman, J., Miller, J., & McMahon., W. (2009). Prenatal, perinatal, and neonatal factors associated with autism spectrum disorders. Pediatrics, 123(5), 1293–1300. https://doi.org/10.1542/peds.2008-0927.
Boppana, S. B. (2010). Dried blood spot real-time polymerase chain reaction assays to screen newborns for congenital cytomegalovirus infection. JAMA, 303(14), 1375–1382. https://doi.org/10.1001/jama.2010.423.
Corriveau, R. A., Huh, G. S., & Shatz, C. J. (1998). Regulation of class I MHC gene expression in the developing and mature CNS by neural activity. Neuron, 21(3), 505–520. https://doi.org/10.1016/S0896-6273(00)80562-0.
de la Torre-Ubieta, L. H., Won, J. L., Stein, D. H., & Geschwind (2016). Advancing the understanding of autism disease mechanisms through genetics. Nature Medicine, 22(4), 345–361. https://doi.org/10.1038/nm.4071.
Deverman, B. E., & Patterson, P. H. (2009). Cytokines and CNS development. Neuron, 64(1), 61–78. https://doi.org/10.1016/j.neuron.2009.09.002.
Dollard, S. C., Grosse, S. D., & Ross, D. S. (2007). New estimates of the prevalence of neurological and sensory sequelae and mortality associated with congenital cytomegalovirus infection. Reviews in Medical Virology, 17(5), 355–363. https://doi.org/10.1002/rmv.544.
Elsabbagh, M., et al. (2012). Global prevalence of autism and other pervasive developmental disorders. Autism Research, 5(3), 160–179. https://doi.org/10.1002/aur.239.
Engman, M. L., et al. (2015). Prenatal acquired cytomegalovirus infection should be considered in children with autism. Acta Paediatrica, 104(8), 792–795. https://doi.org/10.1111/apa.13032.
Engman, M.-L., et al. (2008). Congenital CMV infection: prevalence in newborns and the impact on hearing deficit. Scandinavian Journal of Infectious Disease, 40(11–12), 935–942. https://doi.org/10.1080/00365540802308431.
First, M. B., & Pincus, H. A. (2000). Diagnostic and statistical manual of mental disorders, fourth edition, text revision (DSM-IV-TR). Arlington, VA: American Psychiatric Association.
Garofoli, F., et al. (2017). An Italian prospective experience on the association between congenital cytomegalovirus infection and autistic spectrum disorder. Journal of Autism and Developmental Disorders, 47(5), 1490–1495. https://doi.org/10.1007/s10803-017-3050-3.
Gentile, I., et al. (2014). Prevalence and titre of antibodies to cytomegalovirus and epstein-barr virus in patients with autism spectrum disorder. In Vivo, 28(4), 621–626.
Gentile, I., et al. (2017). Prevalence of congenital cytomegalovirus infection assessed through viral genome detection in dried blood spots in children with autism spectrum disorders. In Vivo, 31(3), 467–473. https://doi.org/10.21873/invivo.11085.
Glazier, A., Kerver, J., Talge, N., Paneth, N., & Racicot, K. (2017). Cytomegalovirus IgG in maternal serum during pregnancy is associated with increased risk for behaviors associated with autism spectrum disorder in children. American Journal of Reproductive Immunology, 78(S1), 43. https://doi.org/10.1111/aji.12736.
Goines, P. E., et al. (2011). Increased midgestational IFN-γ, IL-4 and IL-5 in women bearing a child with autism: A case-control study. Molecular Autism, 2(1), 13. https://doi.org/10.1186/2040-2392-2-13.
Higgins, J., & Green, S. (2017). Cochrane handbook for systematic reviews of interventions version 5.2 [Updated June 2017]. Cochrane Collaboration.
Hsiao, E. Y., & Patterson, P. H. (2012). Placental regulation of maternal-fetal interactions and brain development. Developmental Neurobiology, 72(10), 1317–1326. https://doi.org/10.1002/dneu.22045.
Idring, S., et al. (2015). Changes in prevalence of autism spectrum disorders in 2001–2011: findings from the Stockholm youth cohort. Journal of Autism and Developmental Disorders, 45(6), 1766–1773. https://doi.org/10.1007/s10803-014-2336-y.
Inaba, Y., et al. (2016). Correlation between white matter lesions and intelligence quotient in patients with congenital cytomegalovirus infection. Pediatric Neurology, 55, 52–57. https://doi.org/10.1016/j.pediatrneurol.2015.11.014.
Kanda, Y. (2013). Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplantation, 48(3), 452–458. https://doi.org/10.1038/bmt.2012.244.
Kenneson, A., & Cannon, M. J. (2007). Review and meta-analysis of the epidemiology of congenital cytomegalovirus (CMV) infection. Reviews in Medical Virology, 17(4), 253–276. https://doi.org/10.1002/rmv.535.
Koyano, S., et al. (2011). Screening for congenital cytomegalovirus infection using newborn urine samples collected on filter paper: feasibility and outcomes from a multicentre study. British Medical Journal Open, 1(1), e000118. https://doi.org/10.1136/bmjopen-2011-000118.
Kupper, D. J., & Regier, D. A. (2013). Diagnostic and statistical manual of mental disorders, fifth edition (DSM-V). Arlington, VA: American Psychiatric Association.
Lai, M.-C., Lombardo, M. V., & Baron-Cohen, S. (2014). Autism. Lancet, 383(9920), 896–910. https://doi.org/10.1016/S0140-6736(13)61539-1.
Leruez-Ville, M., et al. (2011). Prospective identification of congenital cytomegalovirus infection in newborns using real-time polymerase chain reaction assays in dried blood spots. Clinical Infectious Diseases, 52(5), 575–581. https://doi.org/10.1093/cid/ciq241.
Lo, C. K.-L., Mertz, D., & Loeb, M. (2014). Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Medical Research Methodology, 14(1), 45. https://doi.org/10.1186/1471-2288-14-45.
Lotter, V. (1966). Epidemiology of autistic conditions in young children. Social Psychiatry, 1(3), 124–135. https://doi.org/10.1007/BF00584048.
Mahic, M., et al. (2017). Maternal immunoreactivity to herpes simplex virus 2 and risk of autism spectrum disorder in male offspring. mSphere, 2(1), e00016–00017. https://doi.org/10.1128/mSphere.00016-17.
Malkova, N. V., Yu, C. Z., Hsiao, E. Y., Moore, M. J., & Patterson, P. H. (2012). Maternal immune activation yields offspring displaying mouse versions of the three core symptoms of autism. Brain, Behavier, and Immunity, 26(4), 607–616. https://doi.org/10.1016/j.bbi.2012.01.011.
Markowitz, P. I. (1983). Autism in a child with congenital cytomegalovirus infection. Journal of Autism and Developmental Disorders, 13(3), 249–253.
Ornoy, A., Weinstein-Fudim, L., & Ergaz, Z. (2015). Prenatal factors associated with autism spectrum disorder (ASD). Reproductive Toxicology, 56, 155–169. https://doi.org/10.1016/j.reprotox.2015.05.007.
Patterson, P. H. (2011). Maternal infection and immune involvement in autism. Trends in Molecular Medicine, 17(7), 389–394. https://doi.org/10.1016/j.molmed.2011.03.001.
Ross, S. A., et al. (2015). Urine collection method for the diagnosis of congenital cytomegalovirus infection. Pediatric Infectious Disease Journal, 34(8), 903–905. https://doi.org/10.1097/INF.0000000000000757.
Ruiz-Goikoetxea, M., et al. (2017). Risk of unintentional injuries in children and adolescents with ADHD and the impact of ADHD medications: protocol for a systematic review and meta-analysis. British Medical Journal Open, 7(9), e018027. https://doi.org/10.1136/bmjopen-2017-018027.
Saemundsen, E., Magnússon, P., Georgsdóttir, I., Egilsson, E., & Rafnsson, V. (2013). Prevalence of autism spectrum disorders in an Icelandic birth cohort. British Medical Journal Open, 3(6), e002748. https://doi.org/10.1136/bmjopen-2013-002748.
Sakamoto, A., Moriuchi, H., Matsuzaki, J., Motoyama, K., & Moriuchi, M. (2015). Retrospective diagnosis of congenital cytomegalovirus infection in children with autism spectrum disorder but no other major neurologic deficit. Brain & Development, 37(2), 200–205. https://doi.org/10.1016/j.braindev.2014.03.016.
Smithers-Sheedy, H., et al. (2017). Congenital cytomegalovirus among children with cerebral palsy. Journal of Pediatrics. https://doi.org/10.1016/j.jpeds.2016.10.024.
Stevens, B., et al. (2007). The classical complement cascade mediates CNS synapse elimination. Cell, 131(6), 1164–1178. https://doi.org/10.1016/j.cell.2007.10.036.
Stroup, D. F., et al. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA, 283(15), 2008–2012.
Stubbs, E. G., Ash, E., & Williams, C. P. (1984). Autism and congenital cytomegalovirus. Journal of Autism and Developmental Disorders, 14(2), 183–189.
Sweeten, T. L., Posey, D. J., & McDougle, C. J. (2004). Autistic disorder in three children with cytomegalovirus infection. Journal of Autism and Developmental Disorders, 34(5), 583–586.
Tagawa, M., Tanaka, H., Moriuchi, M., & Moriuchi, H. (2009). Retrospective diagnosis of congenital cytomegalovirus infection at a school for the deaf by using preserved dried umbilical cord. Journal of Pediatrics, 155(5), 749–751. https://doi.org/10.1016/j.jpeds.2009.04.033.
Uematsu, M., et al. (2016). Asymptomatic congenital cytomegalovirus infection with neurological sequelae: A retrospective study using umbilical cord. Brain & Development, 38(9), 819–826. https://doi.org/10.1016/j.braindev.2016.03.006.
van der Knaap, M. S., Vermeulen, G., Barkhof, F., Hart, A. A. M., Loeber, J. G., & Weel, J. F. L. (2004). Pattern of white matter abnormalities at MR imaging: Use of polymerase chain reaction testing of Guthrie cards to link pattern with congenital cytomegalovirus infection. Radiology, 230(2), 529–536. https://doi.org/10.1148/radiol.2302021459.
Wells, G. A., et al. (2014). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/ clinical_epidemiology/oxford.asp.
Yamashita, Y., Fujimoto, C., Nakajima, E., Isagai, T., & Matsuishi, T. (2003). Possible association between congenital cytomegalovirus infection and autistic disorder. Journal of Autism and Developmental Disorders, 33(4), 455–459.
Yamazaki, H., et al. (2012). Cochlear implantation in children with congenital cytomegalovirus infection accompanied by psycho-neurological disorders. Acta Oto-Laryngologica, 132(4), 420–427. https://doi.org/10.3109/00016489.2011.653442.
Yoon, B. H., et al. (1996). Interleukin-6 concentrations in umbilical cord plasma are elevated in neonates with white matter lesions associated with periventricular leukomalacia. American Journal of Obstetrics & Gynecology, 174(5), 1433–1440. https://doi.org/10.1016/S0002-9378(96)70585-9.
Yoon, B. H., et al. (1997a). Amniotic fluid cytokines (interleukin-6, tumor necrosis factor-alpha, interleukin-1 beta, and interleukin-8) and the risk for the development of bronchopulmonary dysplasia. American Journal of Obstetrics & Gynecology, 177(4), 825–830. https://doi.org/10.1016/S0002-9378(97)70432-0.
Yoon, B. H., et al. (1997b). High expression of tumor necrosis factor-alpha and interleukin-6 in periventricular leukomalacia. American Journal of Obstetrics & Gynecology, 177(2), 406–411. https://doi.org/10.1016/S0002-9378(97)70206-0.
Acknowledgments
We thank Prof. Takashi Omori (Clinical and Translational Research Center, Kobe University Hospital) for statistical analysis.
Funding
This work was supported in part by Grants for the Research on Child Development and Diseases (16gk0110021s0101) from the Agency for Medical Research and Development (AMED) and the Young Scientists (B) (17K16299) of JSPS KAKENHI.
Author information
Authors and Affiliations
Contributions
All authors were involved in the design of the study. KM, KT, HN, and NN performed the literature search, evaluated the relevant records for inclusion in the systematic review and meta-analysis, and conducted the statistical analysis. KM and NN drafted the initial manuscript. MY, YT, TK, MM, SK, ST, MN, NS, MN, MTI, IM, and KI revised the article critically for important points. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Maeyama, K., Tomioka, K., Nagase, H. et al. Congenital Cytomegalovirus Infection in Children with Autism Spectrum Disorder: Systematic Review and Meta-Analysis. J Autism Dev Disord 48, 1483–1491 (2018). https://doi.org/10.1007/s10803-017-3412-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-017-3412-x