Abstract
The idiopathic inflammatory bowel diseases (IBD) comprise two types of chronic intestinal disorders: Crohn’s disease and ulcerative colitis. Recruited neutrophils and macrophages contribute to intestinal tissue damage via production of ROS and NF-κB-dependent pro-inflammatory cytokines. The introduction of anti-TNF-α therapies in the treatment of IBD patients was a seminal advance. This therapy is often limited by a loss of efficacy due to the development of adaptive immune response, underscoring the need for novel therapies targeting similar pathways. Vinpocetine is a nootropic drug and in addition to its antioxidant effect, it is known to have anti-inflammatory and analgesic properties, partly by inhibition of NF-κB and downstream cytokines. Therefore, the present study evaluated the effect of the vinpocetine in a model of acid acetic-induced colitis in mice. Treatment with vinpocetine reduced edema, MPO activity, microscopic score and macroscopic damage, and visceral mechanical hyperalgesia. Vinpocetine prevented the reduction of colonic levels of GSH, ABTS radical scavenging ability, and normalized levels of anti-inflammatory cytokine IL-10. Moreover, vinpocetine reduced NF-κB activation and thereby NF-κB-dependent pro-inflammatory cytokines IL-1β, TNF-α, and IL-33 in the colon. Thus, we demonstrate for the first time that vinpocetine has anti-inflammatory, antioxidant, and analgesic effects in a model of acid acetic-induced colitis in mice and deserves further screening to address its suitability as an approach for the treatment of IBD.
Similar content being viewed by others
INTRODUCTION
Inflammatory bowel disease (IBD) is characterized by chronic inflammation of the gastrointestinal tract and includes mainly the ulcerative colitis (UC) and Crohn’s disease (CD) [1]. Its incidence has been increasing in several regions of the world, which makes it a global disease [2]. It takes place with variations in the incidence and predominance in accordance with the region, more commonly in industrialized countries, the urbanization being considered a risk factor [3, 4]. In the USA, IBD is one of the five most common chronic intestinal conditions, with a total cost above 1.7 billion per year [5].
IBD has a great impact on the individuals’ life quality and capacity of work [6] due to the symptoms such as diarrhea (with blood and/or mucus), abdominal pain, vomiting, loss of weight, anemia, fatigue, fever, fistulas, and extra-intestinal manifestations. Focusing on UC, it occurs equally in both sexes, it affects only the colon, in a diffuse manner, recurrent and not transmural [7]. IBD occurs due to an unregulated immune system triggering a response against intestinal microbiota in a genetically sensitive individual [8, 9]. The recruitment of neutrophils and macrophages towards the intestinal tissue is an important event. In the inflammatory foci, these cells produce reactive oxygen species (ROS) and NF-κB-dependent pro-inflammatory cytokines, contributing to tissue damage [6]. In this context, cytokines have a fundamental role in the development and perpetuation of the disease. Pro-inflammatory cytokines such as IL-1β, TNF-α, and IL-33 are found in higher levels in patients with IBD [10,11,12]. Anti-inflammatory cytokines also have a role in controlling IBD development. Patients with mutations in IL-10 production or its receptor have a more severe disease with an early beginning [13]. Chronic intestinal inflammation is associated with the increased production of ROS, which have an important role in the IBD physiopathology in both humans and animals [14, 15].
Vinpocetine is a synthetic ethyl ester derived from vincamine, an alkaloid isolated from the leaves of the Vinca minor [16]. Vinpocetine has been used for the treatment of cerebrovascular diseases, demonstrating a neuroprotective effect and an increase in the cerebral blood flow [17]. Vinpocetine has in vitro and in vivo antioxidant properties [18,19,20,21] in addition to an analgesic effect in different experimental models [19, 20, 22]. Jeon and colleagues demonstrated the anti-inflammatory property of vinpocetine through the inhibition of the IκB kinase (IKK), which prevents the degradation of the IκB (NF-κB cytoplasmic inhibitor) and thereby the translocation of the NF-κB to the nucleus, and consequently the production of pro-inflammatory mediators, such as IL-1β and TNF-α [23]. Vinpocetine also reduces LPS- and carrageenan-induced hyperalgesia by reducing neutrophil recruitment, oxidative stress, NF-κB activation, and consequently pro-inflammatory cytokines, such as IL-1β, TNF-α, and IL-33 [19, 20].
Therefore, vinpocetine is a promising therapeutic approach once targets pro-inflammatory mediators, such as cytokines and ROS that are major players in the pathogenesis of IBD. To our knowledge, this is the first study evaluating the therapeutic effect of vinpocetine in an acid acetic-induced colitis in mice.
MATERIALS AND METHODS
Materials
Vinpocetine was purchased from Tianjin Harmony Technology Development Co. (China) with purity above 99%, bromide of hexadecil trimethyl-ammonium (HTAB); dihydrochloride O-dianisidine; Tween 80; reduced glutathione (GSH); glutaraldehyde; EDTA; iron chloride hexahydrate; 2,4,6-tripiridil-s-triazine (TPTZ); 2,2-azinobis (3-ethylbenzothiazoline-6-sulphonate, diammonium salt; ABTS); Trolox (acid 6-hydroxy-2,5,7,8-tetramethyl croman-2-carboxyl); and potassium persulfate were purchased from Sigma Chemical Co. (St. Louis, USA). Kits for the dosage of IL-1β, IL-33, and IL-10 were purchased from eBioscience (San Diego, USA). For determination of NF-κB activation, primary antibodies were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA), and the secondary antibody purchased from Jackson© ImmunoResearch Inc. (IgG Affinity-Purified Antibodies, West Baltimore Pike, West Grove, PA, USA). All the used reagents were of analytical degree.
Experimental Animals
The experiments were conducted in Swiss male mice, weighing 20 ± 1 g, from the Central vivarium of the Londrina State University, PR, Brazil. At least 2 days before and during the experiments, the animals were maintained in the Department of Pathology of the Londrina State University, in plastic boxes, covered with shavings, with clear/dark cycle of 12 h and temperature between 21 ± 2 °C. The water and food were ad libitum, with the exception of 24 h that preceded the experiments, a period in which the animals were maintained in solid fasting. The proceedings of care and handling of the mice were carried out in accordance with the directions of the International Association for the Study of the Pain (IASP) and approved by the Londrina State University Ethics Committee on Animal Research and Welfare (process number: 3307.2015.37). All the efforts were made to minimize the number of animals and their suffering.
Induction of Experimental Colitis
Mice were anesthetized with ketamine (80 mg/kg, im) and xylazine (10 mg/kg, im) after 24 h of solid fasting. Mice received 100 μL (intracolonic) of sterile saline solution for washing the colon. One hour later, mice received 200 μL (intracolonic) of acetic acid 7.5% (v/v, in saline) or saline (intracolonic). Mice were maintained upside down for 3 min in order to avoid liquid extravasation. Intracolonic injection was performed with a polyethylene cannula of 3 cm length [24].
Experimental Protocols and Treatment
Two experimental protocols were used: (A) mice were treated 10 and 4 h before colitis induction, and 2 h after the induction. In this protocol, mice were euthanized 4 h after colitis induction. After the euthanasia, the samples of the distal colon (1 cm) were collected for GSH and ABTS assays, and edema [24]. The visceral mechanical hyperalgesia was evaluated 3 h after colitis induction (Fig. 1b). In the second protocol (B), mice were treated 2 h before colitis induction, and 4, 10, and 16 h after colitis induction. In this protocol, mice were euthanized 18 h after colitis induction. After the euthanasia, the samples of the distal colon (1 cm) were collected for the determination of MPO activity, dosage of cytokines (IL-1 β, IL-10, IL-33, and TNF-α) [24], and NF-κB activation. Macroscopic score was evaluated using the whole colon and microscopic score was evaluated using the distal colon [24]. The visceral mechanical hyperalgesia was evaluated 3 and 17 h after colitis induction (Fig. 1a). For both protocols, the following experimental groups were used: (1) control groups, animals without colitis (animals that received only saline, intracolonic); (2) colitis group (animals received intracolonic solution of acetic acid to 7.5%, and were treated with vehicle); and (3) vinpocetine group (animals received intracolonic solution of 7.5% acetic acid and were treated with vinpocetine (1, 3, 10, or 30 mg/kg solubilized in 20% of Tween 80 in saline) orally). The vinpocetine dose was determined after analysis of edema and MPO activity. The time points for the treatment with vinpocetine were selected considering its half-life (approximately 2 h) [25] and time points for analysis of each parameter in the colitis model [24].
Schematic representation of experimental colitis protocols and treatment with vinpocetine. In the protocol B, mice were treated with vinpocetine 2 h before; 4, 10, and 16 h after colitis induction. Visceral mechanical hyperalgesia was assessed 3 and 17 h after colitis induction. Samples from the distal portion of the colon (1 cm) were collected 18 h after colitis induction for determination of MPO activity, microscopic score, macroscopic damage, cytokine production, or NF-κB activation (a). In the protocol A, mice were treated with vinpocetine 10 and 4 h before; and 2 h after colitis induction. Visceral mechanical hyperalgesia was performed 3 h after colitis induction. Samples from the distal portion of the colon (1 cm) were collected 4 h after colitis induction for evaluation of edema, GSH, and ABTS (b).
Colon Edema
Fragment measuring 1 cm of the distal portion of the colon was collected and weighed for evaluation of the edema in the tissue. After determination of the weight in grams of 1 cm of colon tissue, the results were expressed as % of increase (of the weight (g)/length of the colon tissue (cm)), relative to the control group without colitis [24, 26, 27].
Myeloperoxidase (MPO) Activity Assay
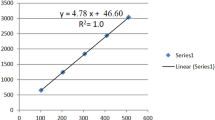
MPO activity in the colon of the mice was measured by the colorimetric method, described by Guazelli et al. [24]. Samples of 1 cm of the distal portion of the colon were collected in ice-cold 50 mM K2HPO4 buffer (pH 6.0) containing 0.5% hexadecyltrimethylammonium bromide (HTAB) and kept at − 80 °C until use. Samples were homogenized, centrifuged (16,100g × 2 min × 4 °C), and the resulting supernatant was assayed for MPO activity spectrophotometrically at 450 nm (Multiskan GO Microplate Spectrophotometer, Thermo Scientific, Vantaa, Finland), with three readings in 1 min. The MPO activity of samples was compared to a standard curve of neutrophils. Briefly, 10 μL of sample was mixed with 200 μL of 50 mM phosphate buffer, pH 6.0, containing 0.167 mg/mL o-dianisidine dihydrochloride and 0.015% hydrogen peroxide. The results are presented as MPO activity.
Macroscopic Damage Score
After the euthanasia, the colon was exposed, opened longitudinally, and the damage scores were determined in accordance with the macroscopic findings using the following criteria outlined elsewhere [24]: no damage (score 0), localized hyperemia but no ulcers (score 1), linear ulcers with no significant inflammation (score 2), linear ulcers with inflammation at one site (score 3), two or more sites of ulceration and inflammation (score 4), one site of inflammation >1 cm along the length of the colon (score 5), and site of inflammation > 2 cm along the length of the colon, with quantification increased by 1 point for each additional centimeter of inflammation (score 6–10). The investigators were blinded to the treatment.
Microscopic Score
Samples of the distal colon were fixed in 10% formalin solution. Formalin-fixed colon samples were embedded in paraffin, and sections (7 μm) were stained with hematoxylin and eosin. Then, the stained tissues were observed with a light microscope (Olympus OX31, Tokyo, Japan), coupled with a digital camera (Lumenera Infinity 1, Ottawa, Canada). The histological assessment of damage was graded semiquantitatively as described previously [24]: (1) loss of mucosal architecture (score 0–3), (2) cellular infiltration (score 0–3), (3) muscle thickening (score 0–3), (4) crypt abscess formation (score 0–3), and (5) goblet cell depletion (score 0–3). The highest possible total score was 15. The investigators were blinded to the treatment.
Visceral Mechanical Hyperalgesia
The visceral mechanical hyperalgesia was valued using an electronic test of von Frey, in accordance with Pereira et al. [28]. Mice were allocated in acrylic cages (12 × 10 × 17 cm) with road surfaces of wire grills in a room with controlled temperature for at least 45 min before the beginning of the measurements. The test consisted in provoking a withdrawal response from the animal with a transducer of portable force (electronic anaesthesiometer; Insight, Ribeirao Preto, SP, Brazil) adapted to a tip of polypropylene of 0.7 mm2, which was applied in the lower abdomen up to the middle abdomen area. The experimenter was trained and care was taken not to stimulate the same point consecutively and the stimulation of the external genitalia was avoided. After withdrawn, the intensity of the pressure was automatically registered, with values of the average of three measurements. One of the following behaviors was considered as a withdrawal response: sharp retraction of the abdomen, immediate licking or scratching of the tip application spot, jump, and flinches [28, 29]). The results were expressed as the delta (∆) of the withdrawal threshold (in grams), calculated subtracting the mean of the values at 3 and 17 h after the colitis induction from the basal values (before treatment with vinpocetine and colitis induction). The investigators were blinded to the treatment.
GSH Assay
The levels of GSH in the samples of the mice’s distal portion of the colon were determined by the spectrophotometric method previously described [24]. Samples of 1 cm of the distal portion of the colon were collected and homogenized in EDTA 0.02 M buffer solution using an ultraturrax (ULTRA-TURRAX®–Ika). The homogenates were treated with acid trichloroacetic at 30% and centrifuged (1.5g × 15 min × 4 °C). Next, 200 μL of Tris-HCl 0.4 M (pH 8.9) buffer was added to the brackets of 150 μL of the supernatant of each sample. After the homogenization, 10 μL of DTNB (dithiobisnitrobenzoic acid) 0.01 M in methanol was added. After 5 min of reaction, the reading was carried out at 412 nm (Multiskan GO Thermo Scientific). The standard curve was prepared with 0.5 μM of GSH, and the results expressed in nanomolar of GSH per milligram of tissue.
ABTS Assay
Samples of 1 cm of the distal colon were homogenized immediately in ice-cold KCl buffer (500 μL, 1.15% weight/volume). The homogenates were centrifuged (0.2 g × 10 min × 4 °C), and the supernatants were used in the assay. Diluted ABTS solution (200 μL) was mixed with 10 μL of sample in each well. After 6 min of incubation (25 °C), the absorbance was measured at 730 nm (Multiskan GO, Thermo Scientific). The ABTS radical scavenging ability in the samples was compared with a standard curve of Trolox (1.5–30 μmol/L), and the results are expressed in millimole of Trolox equivalent per milligram of tissue [24].
Cytokine Measurements
Samples of 1 cm of the distal colon were homogenized in 500 μL of phosphate buffer saline containing protease inhibitors. Cytokine levels were determined as described previously by an enzyme-linked immunosorbent assay (ELISA) using eBioscience kits (eBioscience, San Diego, CA, USA) accordingly with manufacturer instructions. The results were expressed as picograms (pg) of cytokine per milligram of tissue.
NF-κB Activation
Samples of 1 cm of the distal colon were homogenized in RIPA buffer containing protease and phosphatase inhibitors. The lysates were centrifuged (0.5g × 10 min × 4 °C) and the supernatants used in Western blot analysis. The protein extracts were separated by SDS-PAGE and transferred to a nitrocellulose membrane (GE Healthcare-Amersham, Pittsburgh, PA, USA). Membranes were then incubated in blocking buffer (5% bovine serum albumin (BSA) in Tris-buffered saline (TBS) with Tween 20 or 5% nonfat milk) for 2 h at room temperature and incubated overnight at 4 °C in the presence of primary antibody diluted in 5% BSA in TBS with Tween 20 or 5% nonfat milk. The antibodies and Western blot conditions were p-NF-κB p65 (sc-166748, 1:100) and β-Actin (8H10D10, 1:1000) on 10% gel. The molecular protein mass was confirmed by PageRuler™ Prestained Protein Ladder (Thermo Scientific, Rockford, IL, USA). After washing in PBS with Tween 20, the membrane was incubated with secondary antibody for 2 h at room temperature. Protein was visualized by chemiluminescence with Luminata™ Forte Western HRP Substrate (Merck Millipore Corporation, Darmstadt, Germany). The membranes were reprobed with antibody against the total protein of interest to be used as loading control in addition to loading the same amount of protein. Densitometric data were measured using Scientific Imaging Systems (Image Lab 3.0 software; Bio-Rad Laboratories, Hercules, CA).
Statistical Analysis
Results are expressed as mean ± standard error of the mean (SEM) of measures made in 6 mice per group per experiment and are representative of two independent experiments, except for those in the macroscopic score in which 17 animals were used per group and are representative of two independent experiments. Single time point analysis was evaluated using one-way analysis of variance (ANOVA), followed by Tukey’s test. Multiple time points analysis (hyperalgesia) was evaluated using the two-way analysis of variance (ANOVA) repeated measures, followed by Tukey’s test. Categorical variables (analysis of the macroscopic damage score of the colon) were evaluated using the nonparametric test of Kruskal-Wallis, followed by Dunn’s test. The statistical analyses were performed in the GraphPad Prism 5 software (GraphPad Software Inc., San Diego, USA). The differences were considered significant for corresponding values at p < 0.05.
RESULTS
Vinpocetine Reduces Acetic Acid-Induced Edema and MPO Activity
In the first series of experiments, we evaluated the effect of vinpocetine treatment on acetic acid-induced colon edema and MPO activity. Mice were treated with vinpocetine (1, 3, 10, or 30 mg/kg, p.o.), following protocol A (edema evaluation) or B (MPO activity), respectively (Fig. 1). Sample of the colon (1 cm) was collected 4 h (edema evaluation) or 18 h (MPO activity) after colitis induction. All the doses of vinpocetine reduced edema significantly (Fig. 2a). On the other hand, only the dose of 30 mg/kg of vinpocetine reduced significantly the MPO activity (Fig. 2b). Given that, we choose the dose of 30 mg/kg of vinpocetine for the next experiments.
Vinpocetine reduces acetic acid-induced edema and MPO activity. Mice were treated as per protocol A (a) or as per protocol B (b). Samples from the distal colon were collected 4 h after colitis induction (a) and 18 h after colitis induction (b). Results are presented as means ± SEM, n = 6 mice per group per experiment, two independent experiments (*p < 0.05 vs. saline control; #p < 0.05 vs. 0 mg/kg (vehicle), (ANOVA followed by Tukey’s test)).
Vinpocetine Reduces Acetic Acid-Induced Macroscopic Damage and Microscopic Score
Mice were treated with vinpocetine (30 mg/kg, p.o.) following protocol B (Fig. 1a). The whole colon was collected 18 h after colitis induction. Intracolonic injection of acetic acid induced severe tissue damage as observed at the site of inflammation, which was higher than 2 cm along the length of the colon (Fig. 3b, d). On the other hand, mice treated with vinpocetine (30 mg/kg) presented reduced inflammation with focal sites of milder inflammatory response than the vehicle-treated colitis group (Fig. 3c, d). In terms of microscopic analysis, it was observed that acetic acid induced loss of the architecture of the colon with major recruitment of leukocytes and goblet cells depletion (Fig. 4b, d). On the other hand, treatment with vinpocetine preserved the architecture of the colon and goblet cells depletion (Fig. 4c, d).
Vinpocetine decreases acetic acid-induced macroscopic damage. Mice were as per protocol B. Samples from the distal colon were collected 18 h after colitis induction and the macroscopic damage score was determined. Saline (a), colitis + vehicle (b), colitis + vinpocetine 30 mg/kg (c), and macroscopic score (d). Results are presented as means ± SEM, n = 17 mice per group per experiment, two independent experiments (*p < 0.05 vs. saline control; #p < 0.05 vs. 0 mg/kg (vehicle), (Kruskal-Wallis nonparametric test followed by Dunn’s test)).
Vinpocetine reduces acetic acid-induced microscopic changes in the colon. Mice were as per protocol B. Samples from the distal colon were collected 18 h after colitis induction and the microscopic score was determined. Representative images of saline control (a), colitis + vehicle (b), colitis + vinpocetine 30 mg/kg (c), and microscopic score (d). Results are presented as means ± SEM, n = 12 mice per group per experiment, two independent experiments (*p < 0.05 vs. saline control; #p < 0.05 vs. 0 mg/kg (vehicle), (Kruskal-Wallis nonparametric test followed by Dunn’s test)).
Vinpocetine Reduces Acetic Acid-Induced Visceral Mechanical Hyperalgesia
Mice were treated with vinpocetine (1, 3, 10, or 30 mg/kg, p.o.) as per protocol A (Fig. 1b) or with vinpocetine (30 mg/kg, p.o.) as per protocol B (Fig. 1a). Mechanical hyperalgesia was evaluated 3 h after colitis induction, following protocol A, or 3 and 17 h after colitis induction following protocol B. Intracolonic injection of acetic acid induced visceral mechanical hyperalgesia (as observed with an increase of the delta threshold), which was reduced by the treatment with vinpocetine (30 mg/kg) in both protocols (Fig. 5a, b), indicating that vinpocetine possesses analgesic activity.
Vinpocetine reduces acetic acid-induced visceral mechanical hyperalgesia. Mice were treated as per protocol A (a) or as per protocol B (b). Visceral mechanical hyperalgesia was assessed 3 h after colitis induction (a, one-way ANOVA followed by Tukey’s test); or 3 and 17 h after colitis induction (b, two-way ANOVA followed by Tukey’s test). Results are means ± SEM, n = 6 mice per group per experiment, two independent experiments (*p < 0.05 vs. saline control; #p < 0.05 vs. 0 mg/kg (vehicle)).
Vinpocetine Inhibits Acetic Acid-Induced Oxidative Stress
Next, the antioxidant effect of vinpocetine was evaluated. For this, mice were treated with vinpocetine (30 mg/kg, p.o.), as per protocol A (Fig. 1b). Sample of the colon (1 cm) was collected 4 h after colitis induction. Injection of acetic acid reduced the levels of GSH (Fig. 6a) and depleted the total antioxidant capacity (ABTS radical scavenging ability assay) (Fig. 6b). Treatment with vinpocetine decreased acetic acid-induced oxidative stress as observed by an increase of GSH levels and total antioxidant capacity (Fig. 6).
Vinpocetine inhibits acetic acid-induced oxidative stress. Mice were treated as per protocol A. Samples from the distal colon were collected 4 h after colitis induction. Results are presented as means ± SEM, n = 6 mice per group per experiment, two independent experiments (*p < 0.05 vs. saline control; #p < 0.05 vs. 0 mg/kg (vehicle), ANOVA followed by Tukey’s test).
Effect of Vinpocetine on Acid Acetic-Induced Cytokine Production
Mice were treated with vinpocetine (30 mg/kg, p.o.), as per protocol B (Fig. 1a). Sample of the colon (1 cm) was collected 18 h after colitis induction. Acetic acid induced the production of pro-inflammatory cytokines (IL-1β, TNF-α, and IL-33), and the treatment with vinpocetine (30 mg/kg) reduced significantly the production of these cytokines (Fig. 7a–c). In addition, intracolonic injection of acetic acid reduced the levels of the anti-inflammatory cytokine IL-10. Treatment with vinpocetine (30 mg/kg) normalized IL-10 levels (Fig. 7d).
Vinpocetine reduces acetic acid-induced pro-inflammatory cytokines (IL-1β, TNF-α, and IL-33) and prevents the depletion of the anti-inflammatory cytokine IL-10. Mice were treated as per protocol B. Samples from the distal colon were collected 18 h after colitis induction for the determination of IL-1β (a), TNF-α (b), IL-33 0 (c), and IL-10 (d) production. Results are presented as means ± SEM, n = 6 mice per group per experiment, two independent experiments (*p < 0.05 vs. saline control; #p < 0.05 vs. 0 mg/kg (vehicle), ANOVA followed by Tukey’s test).
Vinpocetine Inhibits Acetic Acid-Induced NF-κB Activation
Mice were treated with vinpocetine (30 mg/kg, p.o.), as per protocol B (Fig. 1a). Sample of the colon (1 cm) was collected 18 h after colitis induction. The protein levels of phosphorylated NF-κB p65 (pp65) and β-actin were determined by Western blot. We observed that vinpocetine reduced acetic acid-induced NF-κB activation in the colon (Fig. 8a, b) as observed by a reduction of pp65 expression relative to β-actin expression.
Vinpocetine inhibits acetic acid-induced NF-κB activation. Mice were treated as per protocol B. Samples from the distal colon were collected 18 h after colitis induction for the determination of NF-κB activation (a and b). Results are presented as means ± SEM, n = 6 mice per group per experiment, two independent experiments (*p < 0.05 vs. saline control; #p < 0.05 vs. 0 mg/kg (vehicle), ANOVA followed by Tukey’s test).
DISCUSSION
In the present work, we demonstrated that vinpocetine presents anti-inflammatory, antioxidant, and analgesic effects in a model of acetic acid-induced colitis in mice. These effects were observed through the reduction of edema; MPO activity; macro- and microscopic damage; visceral mechanical hyperalgesia; oxidative stress (normalization of GSH levels and ABTS radical scavenging ability); NF-κB activation; production of pro-inflammatory cytokines such as IL-1β, TNF-α, and IL-33; and normalization of the anti-inflammatory cytokine IL-10 levels. To our knowledge, this is the first demonstration of the vinpocetine effect on experimental colitis.
IBD has a great impact on the patients’ quality of life, and the most common symptoms are diarrhea (with blood and/or mucus), abdominal pain, vomiting, loss of weight, anemia, fatigue, fever, fistulas, and extra-intestinal manifestations [6]. IBD is an intermittent disease switching from light to severe manifestations during the acute phase, and lessening during the remission phase [6, 8, 30]. The current treatment of UC consists mainly in the use of mesalazine, corticosteroids, immunosuppressant, and anti-TNF-α monoclonal antibodies [31]. However, these therapies present several side effects and the efficacy of monoclonal antibodies is often limited by a progressive loss of efficacy due to the development of adaptive immune response against it and several side effects. These elements underscore the need for novel therapies [32,33,34,35]. In this sense, some clinical studies demonstrated that long-term use of vinpocetine does not induce significant side effects, indicating that it possesses a safe clinical profile [36,37,38]. Vinpocetine is absorbed in the stomach and intestine, being able to cross the blood-brain barrier. In spite of being known as a phosphodiesterase-1 (PDE-1) inhibitor, evidence demonstrates that vinpocetine also has anti-inflammatory actions independent on targeting PDE-1. In fact, vinpocetine reduces NF-κB activation in vivo in different experimental settings [19,20,21]. The inhibition of IκB kinase (IKK) [23] and inhibition of the NF-κB upstream enzyme Akt [39] are the underlying mechanism of vinpocetine inhibition of NF-κB activation. The inhibition of these enzymes prevents the degradation of IκB and thereby translocation of NF-κB to the nucleus, and consequently inhibition of NF-κB-dependent cytokines, such as IL-1β and TNF-α [23].
The recruitment of neutrophils into the inflamed mucosal membrane is an important histological finding in patients with IBD, specifically in UC. In the inflammatory foci, neutrophils contribute to tissue damage and dysfunction of the mucosal membrane [40]. In fact, neutrophils are important sources of ROS and pro-inflammatory cytokines, which can further contribute to tissue damage. The IBD disease activity correlates with the neutrophils influx in the mucosal membrane, resulting in the formation of abscesses crypts [41, 42]. MPO is an abundant enzyme mainly in azurophilic granules of neutrophils [43]. It is involved in the generation of hypochlorous acid, a powerful oxidant that possesses bactericidal activity, but also induces tissue damage [44]. MPO can be used as a quantitative indicator of the inflammation due to its activity being directly proportional to the number of neutrophils [45]. Our results show that vinpocetine reduces edema, macroscopic and microscopic score, and MPO activity in a model of colitis induced by acetic acid. In lung tissue, vinpocetine was able to reduce TNF-α- and lipopolysaccharide (LPS)-induced neutrophils recruitment [23]. Evidence also demonstrates that vinpocetine reduces MPO activity and leukocyte recruitment in the carrageenan and LPS models of inflammation [19, 20]. Therefore, the reduction of neutrophil recruitment is an important finding.
Reactive oxygen species (ROS) play an important role in the pathophysiology of IBD [14, 15, 46]. In fact, patients with IBD have lower antioxidant capacity (even in the asymptomatic phase of the disease) [47] and present higher levels oxidative DNA damage [48] than healthy individuals. The activation of inflammatory cells such as neutrophils and macrophages triggers the production of superoxide anion, nitric oxide, and peroxynitrite, resulting in the establishment of oxidative stress in the IBD [49]. Importantly, ROS also modulate the NF-κB activation and consequently, increase the expression of pro-inflammatory cytokines, adhesion molecules, and the perpetuation of the inflammation [50,51,52]. In fact, treatment with antioxidants such as the flavonoid quercetin [24] or the GSH precursor N-acetylcysteine (NAC) [53] reduces colitis-induced oxidative stress. In vitro data demonstrated that vinpocetine is a powerful antioxidant molecule [18]. Vinpocetine reduces in vivo lipid peroxidation, nitrite production, and restores GSH and total antioxidant defenses in different models such as carrageenan- and LPS-induced inflammation [19, 20] and diclofenac-induced kidney injury [21]. This mechanism is related to the ability of scavenging hydroxyl radicals and other ROS [54, 55]. Corroborating to this rationale, our results show that vinpocetine inhibited the oxidative stress by normalizing total antioxidant capacity and GSH levels, and prevented the reduction of ABTS radical scavenging ability in acetic acid-induced colitis.
Abdominal pain is a common symptom reaching up to 70% of the patients who seek medical assistance, either in cases of initial diagnosis or in relapsing episodes [56, 57]. As matter of fact, depression and anxiety are common symptoms of patients with IBD due to the chronic abdominal pain [58]. Inflammatory mediators such IL-1β, TNF-α, IL-33, and the nerve growth factor (NGF) released by neutrophils, macrophages, and mast cells can activate nociceptors and induce pain [59,60,61,62]. In fact, mice lacking ST2 (IL-33 receptor) or TNFR1 (TNF-α receptor) present decreased abdominal pain [63, 64]. In addition to that, ROS such as superoxide anion and peroxynitrite are also able to induce hyperalgesia [65,66,67,68]. In fact, intraperitoneal injection of a superoxide anion donor causes abdominal contortions in mice [68]. Vinpocetine has been shown to reduce pain in different experimental models [19, 20, 22]. Vinpocetine reduces LPS- and carrageenan-induced hyperalgesia by reducing neutrophil recruitment, oxidative stress, NF-κB activation, and consequently pro-inflammatory cytokines, such as IL-1β, TNF-α, and IL-33 [19, 20]. Whole-cell voltage-clamp recording demonstrated that vinpocetine blocks the Nav1.8 sodium inward current [69], indicating another possible mechanism by which vinpocetine exerts its analgesic effect. This is important given that dorsal root ganglion (DRG) nociceptor neurons express the Nav1.8 channel and its activity is related to pain [69]. Vinpocetine also blocks the axoplasmic transport of NGF in the peripheral sensory neurons and reduces the release of the pain-related neuropeptides substance P and CGRP in the spinal cord [70]. Herein, we observed that vinpocetine reduced colonic neutrophils recruitment and production of hyperalgesic cytokines, such as IL-1β, TNF-α, and IL-33, which may account for its analgesic effect. Therefore, the inhibition of acetic acid-induced visceral mechanical hyperalgesia is an important finding, given that abdominal pain is a symptom inherent of patients with IBD [71]. Of note, vinpocetine also presented antidepressant-like activity in the forced swimming test [22]. Given the prevalence of depression in IBD, vinpocetine could not only modulate pain but also modulate mood. However, it is relevant to mention that studies addressing whether vinpocetine would present analgesic and antidepressant effects at the same dose are still required.
Cytokines have a central role in the development and perpetuation of IBD [6]. In fact, high levels of IL-1β were found in the colon of patients with active IBD [12]. This finding correlates with disease activity and colon damage [72]. Another important cytokine, TNF-α attached to the membrane or soluble, is increased in patients with IBD [10]. IL-33 is another important cytokine, given that its level correlated with disease activity and is found in higher levels in patients with UC than patients with CD or healthy individuals [11]. On the other side, the anti-inflammatory cytokine IL-10 has an important role in homeostatic regulation of the intestinal inflammatory response. In fact, mice lacking IL-10 develop spontaneous gut inflammation, which is reversed by treatment with recombinant IL-10 [73]. Patients with mutations in IL-10 production or its receptor have a more severe disease with an early beginning [13]. Our results show that vinpocetine inhibits the NF-κB activation, which explains the reduced levels of pro-inflammatory cytokines such as IL-1β, TNF-α, IL-33, and normalized levels of anti-inflammatory cytokine IL-10. Other studies demonstrated that vinpocetine reduces the production of pro-inflammatory cytokines such as IL-1β, TNF-α, and IL-33 by inhibiting NF-κB activation [19, 20, 23] demonstrating that this signaling pathway is one of the targets of vinpocetine. Importantly, in vitro evidence demonstrate that NF-κB p65 antisense oligonucleotides reduces the expression of the NF-κB p65 subunit and the NF-κB-dependent cytokines IL-1β and IL-8 in the lamina propria mononuclear cells from patients with ulcerative colitis [74], demonstrating the clinical relevance of targeting this signaling pathway.
CONCLUSIONS
The present study demonstrated that vinpocetine ameliorates acetic acid-induced colitis due to inhibition of neutrophils recruitment, abdominal hyperalgesia, oxidative stress, pro-inflammatory cytokines production, and NF-κB activation. To the best of our knowledge, this is the first report demonstrating the effect of vinpocetine in experimental colitis. Given the therapeutic effects herein observed, the fact that vinpocetine is a safe drug because it presents no side effects and is widely used in the clinic for cerebrovascular diseases, our data suggest that vinpocetine is a promising molecule for the treatment of IBD such as ulcerative colitis.
References
de Souza, H.S.P., and C. Fiocchi. 2015. Immunopathogenesis of IBD : Nature Publishing Group 13:13–27. https://doi.org/10.1038/nrgastro.2016.186.
Molodecky, Natalie A., Ing Shian Soon, Doreen M. Rabi, William A. Ghali, Mollie Ferris, Greg Chernoff, Eric I. Benchimol, et al. 2012. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 142. Elsevier Inc: 46–54. https://doi.org/10.1053/j.gastro.2011.10.001.
Burisch, Johan, Tine Jess, Matteo Martinato, and Peter L. Lakatos. 2013. The burden of inflammatory bowel disease in Europe. Journal of Crohn's & Colitis 7. European Crohn’s and Colitis Organisation: 322–337. https://doi.org/10.1016/j.crohns.2013.01.010.
Soon, Ing Shian, Natalie A. Molodecky, Doreen M. Rabi, William A. Ghali, Herman W. Barkema, and Gilaad G. Kaplan. 2012. The relationship between urban environment and the inflammatory bowel diseases: a systematic review and meta-analysis. BMC Gastroenterology 12: 51. https://doi.org/10.1186/1471-230X-12-51.
Abegunde, Ayokunle T., Bashir H. Muhammad, and Tauseef Ali. 2016. Preventive health measures in inflammatory bowel disease. World Journal of Gastroenterology 22. Baishideng Publishing Group Inc: 7625–7644. https://doi.org/10.3748/wjg.v22.i34.7625.
Neurath, Markus F. 2014. Cytokines in inflammatory bowel disease. Nature Reviews Immunology 14. Nature Publishing Group: 329–342. https://doi.org/10.1038/nri3661.
Baumgart, Daniel C., and William J. Sandborn. 2007. Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet 369: 1641–1657. https://doi.org/10.1016/S0140-6736(07)60751-X.
de Lange, Katrina M., and Jeffrey C. Barrett. 2015. Understanding inflammatory bowel disease via immunogenetics. Journal of Autoimmunity 64: 91–100. https://doi.org/10.1016/j.jaut.2015.07.013.
Molodecky, Natalie A., and Gilaad G. Kaplan. 2010. Environmental risk factors for inflammatory bowel disease. Gastroenterology & Hepatology 6: 339–346. https://doi.org/10.1007/s10620-014-3350-9.
Atreya, Raja, Michael Zimmer, Brigitte Bartsch, Maximilian J. Waldner, Imke Atreya, Helmut Neumann, Kai Hildner, et al. 2011. Antibodies against tumor necrosis factor (TNF) induce T-cell apoptosis in patients with inflammatory bowel diseases via TNF receptor 2 and intestinal CD14 + macrophages. Gastroenterology 141. Elsevier Inc: 2026–2038. https://doi.org/10.1053/j.gastro.2011.08.032.
Beltrán, Caroll J., Lucía E. Núñez, David Díaz-Jiménez, Nancy Farfan, Enzo Candia, Claudio Heine, Francisco López, María Julieta González, Rodrigo Quera, and Marcela A. Hermoso. 2010. Characterization of the novel ST2/IL-33 system in patients with inflammatory bowel disease. Inflammatory Bowel Diseases 16: 1097–1107. https://doi.org/10.1002/ibd.21175.
McAlindon, M.E., C.J. Hawkey, and Y.R. Mahida. 1998. Expression of interleukin 1 beta and interleukin 1 beta converting enzyme by intestinal macrophages in health and inflammatory bowel disease. Gut 42: 214–219.
Lee, Cheng Hiang, Peter Hsu, Brigitte Nanan, Ralph Nanan, Melanie Wong, Kevin J. Gaskin, Rupert W. Leong, Ryan Murchie, Aleixo M. Muise, and Michael O. Stormon. 2014. Novel de novo mutations of the interleukin-10 receptor gene lead to infantile onset inflammatory bowel disease. Journal of Crohn's & Colitis 8. European Crohn’s and Colitis Organisation: 1551–1556. https://doi.org/10.1016/j.crohns.2014.04.004.
Karp, Sean M., and Timothy R. Koch. 2006. Oxidative Stress and Antioxidants in Inflammatory Bowel Disease. Disease-a-Month 52: 199–207. https://doi.org/10.1016/j.disamonth.2006.05.005.
Pavlick, K.P., F.S. Laroux, J. Fuseler, R.E. Wolf, L. Gray, J. Hoffman, and M.B. Grisham. 2002. Role of reactive metabolites of oxygen and nitrogen in inflammatory bowel disease. Free Radical Biology and Medicine 33: 311–322.
Lorincz, C., K. Szasz, and L. Kisfaludy. 1976. The synthesis of ethyl apovincaminate. Arzneimittel-Forschung 26: 1907.
Bereczki, D., and I. Fekete. 1999. Asystematic review of vinpocetine therapy in acute ischaemic stroke. European Journal of Clinical Pharmacology 55: 349–352.
Horvath, Beata, Zsolt Marton, Robert Halmosi, Tamas Alexy, Laszlo Szapary, Judit Vekasi, Zsolt Biro, Tamas Habon, Gabor Kesmarky, and Kalman Toth. 2002. In Vitro Antioxidant Properties of Pentoxifylline, Piracetam, and Vinpocetine. Clinical Neuropharmacology 25: 37–42.
Ruiz-Miyazawa, Kenji W., Felipe A. Pinho-Ribeiro, Ana C. Zarpelon, Larissa Staurengo-Ferrari, Rangel L. Silva, Jose C. Alves-Filho, Thiago M. Cunha, Fernando Q. Cunha, Rubia Casagrande, and Waldiceu A. Verri. 2015. Vinpocetine reduces lipopolysaccharide-induced inflammatory pain and neutrophil recruitment in mice by targeting oxidative stress, cytokines and NF-κB. Chemico-Biological Interactions 237. Elsevier Ireland Ltd: 9–17. https://doi.org/10.1016/j.cbi.2015.05.007.
Ruiz-Miyazawa, Kenji W., Ana C. Zarpelon, Felipe A. Pinho-Ribeiro, Gabriela F. Pavão-De-Souza, Rubia Casagrande, and Waldiceu A. Verri. 2015. Vinpocetine reduces carrageenan-induced inflammatory hyperalgesia in mice by inhibiting oxidative stress, cytokine production and NF-κB activation in the paw and spinal cord. PLoS One 10: 1–18. https://doi.org/10.1371/journal.pone.0118942.
Fattori, Victor, Sergio M. Borghi, Carla F.S. Guazelli, Andressa C. Giroldo, Jefferson Crespigio, Allan J.C. Bussmann, Letícia Coelho-Silva, et al. 2017. Vinpocetine reduces diclofenac-induced acute kidney injury through inhibition of oxidative stress, apoptosis, cytokine production, and NF-κB activation in mice. Pharmacological Research 120. Elsevier Ltd: 10–22. https://doi.org/10.1016/j.phrs.2016.12.039.
Abdel-Salam, Omar M.E. 2006. Vinpocetine and piracetam exert antinociceptive effect in visceral pain model in mice. Pharmacological Reports 58: 680–691.
Jeon, Kye-Im, Xiangbin Xu, Toru Aizawa, Jae Hyang Lim, Hirofumi Jono, Dong-Seok Kwon, Jun-Ichi Abe, Bradford C. Berk, Jian-Dong Li, and Chen Yan. 2010. Vinpocetine inhibits NF-kappaB-dependent inflammation via an IKK-dependent but PDE-independent mechanism. Proceedings of the National Academy of Sciences of the United States of America 107: 9795–9800. https://doi.org/10.1073/pnas.0914414107.
Guazelli, Carla F.S., Victor Fattori, Barbara B. Colombo, Sandra R. Georgetti, Fabiana T.M.C. Vicentini, Rubia Casagrande, Marcela M. Baracat, and Waldiceu A. Verri Jr. 2013. Quercetin-Loaded Microcapsules Ameliorate Experimental Colitis in Mice by Anti-inflammatory and Antioxidant Mechanisms. Journal of Natural Products 76: 200–208.
Polgár, M., L. Vereczkey, and I. Nyáry. 1985. Pharmacokinetics of vinpocetine and its metabolite, apovincaminic acid, in plasma and cerebrospinal fluid after intravenous infusion. Journal of Pharmaceutical and Biomedical Analysis 3: 131–139.
Lee, Ji Yun, Hyo Sook Kang, Byoung Eon Park, Hyo Jin Moon, Sang Soo Sim, and Chang Jong Kim. 2009. Inhibitory effects of Geijigajakyak-Tang on trinitrobenzene sulfonic acid-induced colitis. Journal of Ethnopharmacology 126: 244–251. https://doi.org/10.1016/j.jep.2009.08.035.
Barbosa, Andre Luiz Dos Reis. 2011. Colite experimental induzida pelo ácido trinitrobenzeno sulfônico (TNBS) em ratos reduz a resposta hipernociceptiva inflamatória- papel das vias endocanabinóides, opióides endógenos e NO/GMPC/PKG/K+ATP. Universidade Federal do Ceará.
Pereira, L.M.S., R.C.P. Lima-Júnior, A.X.C. Bem, C.G. Teixeira, L.S. Grassi, R.P. Medeiros, R.D. Marques-Neto, R.B. Callado, K.S. Aragão, D.V.T. Wong, M.L. Vale, G.A.C. Brito, and R.A. Ribeiro. 2013. Blockade of TRPA1 with HC-030031 attenuates visceral nociception by a mechanism independent of inflammatory resident cells, nitric oxide and the opioid system. European Journal of Pain (United Kingdom) 17: 223–233. https://doi.org/10.1002/j.1532-2149.2012.00177.x.
Laird, J.M.A., L. Martinez-Caro, E. Garcia-Nicas, and F. Cervero. 2001. A new model of visceral pain and referred hyperalgesia in the mouse. Pain 92: 335–342. https://doi.org/10.1016/S0304-3959(01)00275-5.
Bernstein, Charles N., Michael Fried, J.H. Krabshuis, Henry Cohen, R. Eliakim, Suleiman Fedail, Richard Gearry, et al. 2010. World gastroenterology organization practice guidelines for the diagnosis and management of IBD in 2010. Inflammatory Bowel Diseases 16: 112–124. https://doi.org/10.1002/ibd.21048.
Kane, S.V. 2006. Systematic review: Adherence issues in the treatment of ulcerative colitis. Alimentary Pharmacology and Therapeutics 23: 577–585. https://doi.org/10.1111/j.1365-2036.2006.02809.x.
Goldberg, Rimma, and Peter M. Irving. 2015. Toxicity and response to thiopurines in patients with inflammatory bowel disease. Expert Review of Gastroenterology & Hepatology 9: 1–10. https://doi.org/10.1586/17474124.2015.1039987.
Hansen, Richard A., Gerald Gartlehner, Gregory E. Powell, and Robert S. Sandler. 2007. Serious Adverse Events With Infliximab: Analysis of Spontaneously Reported Adverse Events. Clinical Gastroenterology and Hepatology 5: 729–735. https://doi.org/10.1016/j.cgh.2007.02.016.
Higgins, Peter D.R., Martha Skup, Parvez M. Mulani, Jay Lin, and Jingdong Chao. 2015. Increased Risk of Venous Thromboembolic Events With Corticosteroid vs Biologic Therapy for Inflammatory Bowel Disease. Clinical Gastroenterology and Hepatology 13. Elsevier, Inc: 316–321. https://doi.org/10.1016/j.cgh.2014.07.017.
Lukert, B.P., and L.G. Raisz. 1990. Glucocorticoid-induced osteoporosis: pathogenesis and management. Annals of Internal Medicine 112: 352–364. https://doi.org/10.7326/0003-4819-112-5-352.
Balestreri, R., L. Fontana, and F. Astengo. 1987. A double-blind placebo controlled evaluation of the safety and efficacy of vinpocetine in the treatment of patients with chronic vascular senile cerebral dysfunction. Journal of the American Geriatrics Society 35: 425–430.
Thal, L.J., D.P. Salmon, B. Lasker, D. Bower, and M.R. Klauber. 1989. The safety and lack of efficacy of vinpocetine in Alzheimer’s disease. Journal of the American Geriatrics Society 37: 515–520.
Zhang, Weiwei, Yining Huang, Ying Li, Liming Tan, Jianfei Nao, Hongtao Hu, Jingyu Zhang, Chen Li, Yuenan Kong, and Yulin Song. 2016. Efficacy and Safety of Vinpocetine as Part of Treatment for Acute Cerebral Infarction: A Randomized, Open-Label, Controlled, Multicenter CAVIN (Chinese Assessment for Vinpocetine in Neurology) Trial. Clinical Drug Investigation 36. Springer International Publishing: 697–704. https://doi.org/10.1007/s40261-016-0415-x.
Zhuang, Jianhui, Wenhui Peng, Hailing Li, Yuyan Lu, Ke Wang, Fan Fan, Shuang Li, and Yawei Xu. 2013. Inhibitory effects of vinpocetine on the progression of atherosclerosis are mediated by Akt/NF-kB dependent mechanisms in apoE−/− mice. PLoS One 8: 1–12. https://doi.org/10.1371/journal.pone.0082509.
Higa, A., T. Eto, and Y. Nawa. 1997. Evaluation of the role of neutrophils in the pathogenesis of acetic acid-induced colitis in mice. Scandinavian Journal of Gastroenterology 32: 564–568.
Blake, K.M., S.O. Carrigan, A.C. Issekutz, and A.W. Stadnyk. 2004. Neutrophils migrate across intestinal epithelium using β2 integrin (CD11b/CD18)-independent mechanisms. Clinical and Experimental Immunology 136: 262–268. https://doi.org/10.1111/j.1365-2249.2004.02429.x.
Carrigan, Svetlana O., Amy L. Weppler, Andrew C. Issekutz, and Andrew W. Stadnyk. 2005. Neutrophil differentiated HL-60 cells model Mac-1 (CD11b/CD18)-independent neutrophil transepithelial migration. Immunology 115: 108–117. https://doi.org/10.1111/j.1365-2567.2005.02131.x.
Naito, Yuji, Tomohisa Takagi, and Toshikazu Yoshikawa. 2007. Molecular fingerprints of neutrophil-dependent oxidative stress in inflammatory bowel disease. Journal of Gastroenterology 42: 787–798. https://doi.org/10.1007/s00535-007-2096-y.
Klebanoff, Seymour J. 2005. Myeloperoxidase: friend and foe. Journal of Leukocyte Biology 77: 598–625. https://doi.org/10.1189/jlb.1204697.1.
Krawisz, J.E., P. Sharon, and W.F. Stenson. 1984. Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity. Assessment of inflammation in rat and hamster models. Gastroenterology 87: 1344–1350.
Pravda, Jay. 2005. Radical induction theory of ulcerative colitis. World Journal of Gastroenterology 11: 2371–2384.
Achitei, D., A. Ciobica, G. Balan, E. Gologan, C. Stanciu, and G. Stefanescu. 2013. Different profile of peripheral antioxidant enzymes and lipid peroxidation in active and non-active inflammatory bowel disease patients. Digestive Diseases and Sciences 58: 1244–1249. https://doi.org/10.1007/s10620-012-2510-z.
Pereira, Cristiana, Rosa Coelho, Daniela Grácio, Cláudia Dias, Marco Silva, Armando Peixoto, Pedro Lopes, Carla Costa, João Paulo Teixeira, Guilherme Macedo, and Fernando Magro. 2016. DNA Damage and Oxidative DNA Damage in InflammatoryBowel Disease. Journal of Crohn's & Colitis 10: 1316–1323. https://doi.org/10.1093/ecco-jcc/jjw088.
Pacher, Pál, Joseph S. Beckman, and Lucas Liaudet. 2007. Nitric oxide and peroxynitrite in health and disease. Physiological Reviews 87: 315–424. https://doi.org/10.1152/physrev.00029.2006.
Chiurchiu, V., and M. Maccarrone. 2011. Chronic inflammatory disorders and their redox control: from molecular mechanisms to therapeutic opportunities. Antioxidants & Redox Signaling 15: 2605–2641. https://doi.org/10.1089/ars.2010.3547.
Christman, John W., and Timothy S. Blackwell. 2000. Redox Regulation of Nuclear Factor Kappa B: Therapeutic Potential for Attenuating Inflammatory Responses. Critical Care 162: 153–162.
Maloy, Kevin J., and Fiona Powrie. 2011. Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature 474: 298–306. https://doi.org/10.1038/nature10208.
Amrouche-Mekkioui, Ilhem, and Bahia Djerdjouri. 2012. N-acetylcysteine improves redox status, mitochondrial dysfunction, mucin-depleted crypts and epithelial hyperplasia in dextran sulfate sodium-induced oxidative colitis in mice. European Journal of Pharmacology 691. Elsevier: 209–217. https://doi.org/10.1016/j.ejphar.2012.06.014.
Zaki, Hala Fahmy, and Rania Mohsen Abdelsalam. 2013. Vinpocetine protects against liver ischemia-reperfusion injury. Canadian Journal of Physiology and Pharmacology 91: 1064–1070. https://doi.org/10.1139/cjpp-2013-0097.
Santos, M.S., A.I. Duarte, P.I. Moreira, and C.R. Oliveira. 2000. Synaptosomal response to oxidative stress: effect of vinpocetine. Free Radical Research 32: 57–66.
Aghazadeh, Rahim, Mohammad Reza Zali, Ali Bahari, Kamyar Amin, Farzin Ghahghaie, and Farzad Firouzi. 2005. Inflammatory bowel disease in Iran: A review of 457 cases. Journal of Gastroenterology and Hepatology (Australia) 20: 1691–1695. https://doi.org/10.1111/j.1440-1746.2005.03905.x.
Wagtmans, M.J., H.W. Verspaget, C.B.H.W. Lamers, and R.A. van Hogezand. 1998. Crohn’s Disease in the Elderly: A Comparison With Young Adults. Journal of Clinical Gastroenterology 27: 129–133.
Regueiro, Miguel, Julia B. Greer, and Eva Szigethy. 2017. Etiology and Treatment of Pain and Psychosocial Issues in Patients with Inflammatory Bowel Diseases. Gastroenterology 152. Elsevier Ltd: 430–439. https://doi.org/10.1053/j.gastro.2016.10.036.
Binshtok, A.M., H. Wang, and K. Zimmermann. 2008. Nociceptors Are Interleukin-1ßSensors. J Neurosci 28: 14062–14073. https://doi.org/10.1523/JNEUROSCI.3795-08.2008 Nociceptors.
Jin, X. 2006. Acute p38-Mediated Modulation of Tetrodotoxin-Resistant Sodium Channels in Mouse Sensory Neurons by Tumor Necrosis Factor-α. Journal of Neuroscience 26: 246–255. https://doi.org/10.1523/JNEUROSCI.3858-05.2006.
Wright, A. 1999. Recent concepts in the neurophysiology of pain. Manual Therapy 4: 196–202. https://doi.org/10.1054/math.1999.0207.
Zarpelon, A.C., T.M. Cunha, J.C. Alves-Filho, L.G. Pinto, S.H. Ferreira, D. Xu I B McInnes, F.Y. Liew, F.Q. Cunha, and W.A. Verri. 2013. IL-33/ST2 signalling contributes to carrageenin-induced innate inflammation and inflammatory pain: Role of cytokines, endothelin-1 and prostaglandin E2. British Journal of Pharmacology 169: 90–101. https://doi.org/10.1111/bph.12110.
Yamacita-Borin, Fabiane Y., Ana C. Zarpelon, Felipe A. Pinho-Ribeiro, Victor Fattori, Jose C. Alves-Filho, Fernando Q. Cunha, Thiago M. Cunha, Rubia Casagrande, and Waldiceu A. Verri. 2015. Superoxide anion-induced pain and inflammation depends on TNFα/TNFR1 signaling in mice. Neuroscience Letters 605. Elsevier Ireland Ltd: 53–58. https://doi.org/10.1016/j.neulet.2015.08.015.
Magro, D.A.C., M.S.N. Hohmann, S.S. Mizokami, T.M. Cunha, J.C. Alves-Filho, R. Casagrande, S.H. Ferreira, F.Y. Liew, F.Q. Cunha, and A. Verri Jr. 2013. An interleukin-33/ST2 signaling deficiency reduces overt pain-like behaviors in mice. Brazilian Journal of Medical and Biological Research 46: 601–606. https://doi.org/10.1590/1414-431X20132894.
Ma, Fei, Liping Zhang, and Karin N. Westlund. 2009. Reactive oxygen species mediate TNFR1 increase after TRPV1 activation in mouse DRG neurons. Molecular Pain 5: 31. https://doi.org/10.1186/1744-8069-5-31.
Salvemini, Daniela, Joshua W. Little, Timothy Doyle, and William L. Neumann. 2011. Roles of reactive oxygen and nitrogen species in pain. Free Radical Biology & Medicine 51: 951–966. https://doi.org/10.1016/j.freeradbiomed.2011.01.026.
Wang, Zq, Frank Porreca, and Salvatore Cuzzocrea. 2004. A newly identified role for superoxide in inflammatory pain. The Journal of Pharmacology and Experimental Therapeutics 309: 869–878. https://doi.org/10.1124/jpet.103.064154.increased.
Maioli, N.A., A.C. Zarpelon, S.S. Mizokami, C. Calixto-Campos, C.F.S. Guazelli, M.S.N. Hohmann, F.A. Pinho-Ribeiro, T.T. Carvalho, M.F. Manchope, C.R. Ferraz, R. Casagrande, and W.A. Verri Jr. 2015. The superoxide anion donor, potassium superoxide, induces pain and inflammation in mice through production of reactive oxygen species and cyclooxygenase-2. Brazilian Journal of Medical and Biological Research 48: 321–331. https://doi.org/10.1590/1414-431X20144187.
Zhou, Xiaoping, X.W. Dong, and James Crona. 2003. Vinpocetine is a potent blocker of rat NaV1. 8 tetrodotoxin-resistant sodium channels. Journal of Pharmacology and Experimental Therapeutics 306: 498–504. https://doi.org/10.1124/jpet.103.051086.
Knyihar-Csillik, Elizabeth, Laszlo Vecsei, Andras Mihaly, Robert Fenyo, Ibolya Farkas, Beata Krisztin-Peva, and Bertalan Csillik. 2007. Effect of vinpocetine on retrograde axoplasmic transport. Annals of Anatomy 189: 39–45. https://doi.org/10.1016/j.aanat.2006.07.006.
Akbar, A., Y. Yiangou, P. Facer, J.R.F. Walters, P. Anand, and S. Ghosh. 2008. Increased capsaicin receptor TRPV1-expressing sensory fibres in irritable bowel syndrome and their correlation with abdominal pain. Gut 57: 923–929. https://doi.org/10.1136/gut.2007.138982.
Ludwiczek, O., E. Vannier, I. Borggraefe, A. Kaser, B. Siegmund, C.A. Dinarello, and Herbert Tilg. 2004. Imbalance between interleukin-1 agonists and antagonists: Relationship to severity of inflammatory bowel disease. Clinical and Experimental Immunology 138: 323–329. https://doi.org/10.1111/j.1365-2249.2004.02599.x.
Steidler, L., W. Hans, L. Schotte, S. Neirynck, F. Obermeier, W. Falk, W. Fiers, and E. Remaut. 2000. Treatment of murine colitis by Lactococcus lactis secreting interleukin-10. Science 289: 1352–1355.
Li, Zhi, De Kui Zhang, Wen Quan Yi, Qin Ouyang, You Qin Chen, and Hua Tian Gan. 2008. NF-KB p65 Antisense Oligonucleotides May Serve as a Novel Molecular Approach for the Treatment of Patients with Ulcerative Colitis. Archives of Medical Research 39. Elsevier Inc: 729–734. https://doi.org/10.1016/j.arcmed.2008.08.001.
Acknowledgments
Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Central Multiusuária de Laboratórios de Pesquisa da UEL (CMLP), Fundação Araucária, and Paraná State Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The proceedings of care and handling of the mice were carried out in accordance with the directions of the International Association for the Study of the Pain (IASP) and approved by the Londrina State University Ethics Committee on Animal Research and Welfare (process number: 3307.2015.37).
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Bárbara B. Colombo and Victor Fattori contributed equally to this work.
Rights and permissions
About this article
Cite this article
Colombo, B.B., Fattori, V., Guazelli, C.F.S. et al. Vinpocetine Ameliorates Acetic Acid-Induced Colitis by Inhibiting NF-κB Activation in Mice. Inflammation 41, 1276–1289 (2018). https://doi.org/10.1007/s10753-018-0776-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-018-0776-9