Abstract
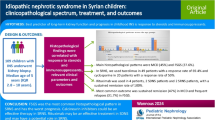
Henoch-Schönlein purpura (HSP) is considered as an immune-mediated inflammatory disease. Serum amyloid A (SAA) is an acute-phase protein with proinflammatory effects. We investigated the levels of SAA in HSP patients and examined whether SAA levels are associated with organ involvement and disease severity. Seventy patients with HSP, including 35 with nephritis (HSPN) and 35 without HSPN, and 20 controls were recruited in our study. SAA levels were measured and other clinical laboratory parameters, including C-reactive protein, erythrocyte sedimentation rate, complement 3 (C3), C4, and immunoglobulin (Ig) A, were recorded. SAA levels were not found to be independently associated with renal, joint involvement, and disease severity. However, higher SAA levels were observed in HSP patients with gastrointestinal (GI) manifestations (p = 0.006, p c = 0.048). Moreover, the levels of SAA were significantly associated with duration of disease (p < 0.005, p c < 0.04). Our findings suggested that SAA was significantly associated with disease duration and GI manifestations in HSP patients.


Similar content being viewed by others
REFERENCES
Yang, Y.H., C.F. Hung, C.R. Hsu, et al. 2005. Nationwide survey on epidemiological characteristics of childhood Henoch—Schönlein purpura in Taiwan. Rheumatology (Oxford, England) 44: 618–622.
Bogdanović, R. 2009. Henoch-Schönlein purpura nephritis in children: risk factors, prevention and treatment. Acta Paediatrica 98: 1882–1889.
Narchi, H. 2005. Risk of long term renal impairment and duration of follow up recommended for Henoch-Schonlein purpura with normal or minimal urinary findings: a systematic review. Archives of Disease in Childhood 90: 916–920.
Lippl, F., W. Huber, M. Werner, et al. 2001. Life-threatening gastrointestinal bleeding due to a jejunal lesion of Henoch-Schönlein purpura. Endoscopy 33: 811–813.
Yang, Y.H., Y.H. Chuang, L.C. Wang, et al. 2008. The immunobiology of Henoch-Schönlein purpura. Autoimmunity Reviews 7: 179–184.
Lin, S.J., J.L. Huang, and K.H. Hsieh. 1998. Clinical and laboratory correlation of acute Henoch-Schönlein purpura in children. Zhonghua Minguo Guo Xiao Er Ke Yi Xue Hui Za Zhi 39: 94–98.
Makay, B., Z. Türkyilmaz, M. Duman, et al. 2009. Mean platelet volume in Henoch-Schönlein purpura: relationship to gastrointestinal bleeding. Clinical Rheumatology 28: 1225–1228.
Zhao, Y., X. He, X. Shi, et al. 2010. Association between serum amyloid A and obesity: a meta-analysis and systematic review. Inflammation Research 59: 323–334.
Urieli-Shoval, S., Z. Finci-Yeheskel, S. Dishon, et al. 2010. Expression of serum amyloid A in human ovarian epithelial tumors: implication for a role in ovarian tumorigenesis. Journal of Histochemistry and Cytochemistry 58: 1015–1023.
Eckhardt, E.R., J. Witta, J. Zhong, et al. 2010. Intestinal epithelial serum amyloid A modulates bacterial growth in vitro and pro-Inflammatory responses in mouse experimental colitis. BMC Gastroenterology 10: 133.
Cunnane, G., S. Grehan, S. Geoghegan, et al. 2000. Serum amyloid A in the assessment of early inflammatory arthritis. Journal of Rheumatology 27: 58–63.
Lange, U., B. Boss, J. Teichmann, et al. 2000. Serum amyloid A an indicator of inflammation in ankylosing spondylitis. Rheumatology International 19: 119–122.
Visvanathan, S., C. Wagner, J. Rojas, et al. 2009. E-selectin, interleukin 18, serum amyloid A, and matrix metalloproteinase 9 are associated with clinical response to golimumab plus methotrexate in patients with active rheumatoid arthritis despite methotrexate therapy. Journal of Rheumatology 36: 1371–1379.
Mitani, Y., H. Sawada, H. Hayakawa, et al. 2005. Elevated levels of high-sensitivity C-reactive protein and serum amyloid-A late after Kawasaki disease: association between inflammation and late coronary sequelae in Kawasaki disease. Circulation 11: 38–43.
Ozen, S., N. Ruperto, M.J. Dillon, et al. 2006. EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides. Annals of the Rheumatic Diseases 65: 936–941.
Mills, J.A., B.A. Michel, D.A. Bloch, et al. 1990. The American College of Rheumatology 1990 criteria for the classification of Henoch–Schönlein purpura. Arthritis and Rheumatism 33: 1114–1121.
He, X., H. Lu, S. Kang, et al. 2010. MEFV E148Q polymorphism is associated with Henoch-Schönlein purpura in Chinese children. Pediatric Nephrology 25: 2077–2082.
Besbas, N., U. Saatci, S. Ruacan, et al. 1997. The role of cytokines in Henoch Schonlein purpura. Scandinavian Journal of Rheumatology 26: 456–460.
Ha, T.S. 2005. The role of tumor necrosis factor-alpha in Henoch-Schonlein purpura. Pediatric Nephrology 20: 149–153.
Yang, Y.H., H.J. Lai, C.M. Huang, et al. 2004. Sera from children with active Henoch-Schönlein purpura can enhance the production of interleukin 8 by human umbilical venous endothelial cells. Annals of the Rheumatic Diseases 63: 1511–1513.
Yang, R.Z., M.J. Lee, H. Hu, et al. 2006. Acute-phase serum amyloid A: an inflammatory adipokine and potential link between obesity and its metabolic complications. PLoS Medicine 3: e287.
Cai, H., C. Song, I. Endoh, et al. 2007. Serum amyloid A induces monocyte tissue factor. Journal of Immunology 178: 1852–1860.
Zhao, Y., S. Zhou, and C.K. Heng. 2007. Impact of serum amyloid A on tissue factor and tissue factor pathway inhibitor expression and activity in endothelial cells. Arteriosclerosis, Thrombosis, and Vascular Biology 27: 1645–1650.
ACKNOWLEDGEMENT
This study was funded by the supporting program of the Ministry of Human Resource of China Oversea Returned scholars.
Author information
Authors and Affiliations
Corresponding author
Additional information
Xuelian He and Yulan Zhao contributed equally.
Rights and permissions
About this article
Cite this article
He, X., Zhao, Y., Li, Y. et al. Serum Amyloid A Levels Associated with Gastrointestinal Manifestations in Henoch-Schönlein Purpura. Inflammation 35, 1251–1255 (2012). https://doi.org/10.1007/s10753-012-9435-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-012-9435-8