Abstract
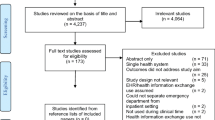
Ambulance offload delay (AOD) occurs when care of incoming ambulance patients cannot be transferred immediately from paramedics to staff in a hospital emergency department (ED). This is typically due to emergency department congestion. This problem has become a significant concern for many health care providers and has attracted the attention of many researchers and practitioners. This article reviews literature which addresses the ambulance offload delay problem. The review is organized by the following topics: improved understanding and assessment of the problem, analysis of the root causes and impacts of the problem, and development and evaluation of interventions. The review found that many researchers have investigated areas of emergency department crowding and ambulance diversion; however, research focused solely on the ambulance offload delay problem is limited. Of the 137 articles reviewed, 28 articles were identified which studied the causes of ambulance offload delay, 14 articles studied its effects, and 89 articles studied proposed solutions (of which, 58 articles studied ambulance diversion and 31 articles studied other interventions). A common theme found throughout the reviewed articles was that this problem includes clinical, operational, and administrative perspectives, and therefore must be addressed in a system-wide manner to be mitigated. The most common intervention type was ambulance diversion. Yet, it yields controversial results. A number of recommendations are made with respect to future research in this area. These include conducting system-wide mitigation intervention, addressing root causes of ED crowding and access block, and providing more operations research models to evaluate AOD mitigation interventions prior implementations. In addition, measurements of AOD should be improved to assess the size and magnitude of this problem more accurately.




Similar content being viewed by others
References
Creemers S, Lambrecht M, Vandaele N (2007) Queueing models in healthcare. Tijdschrift voor economie en management
Aboueljinane L, Sahin E, Jemai Z (2013) A review on simulation models applied to emergency medical service operations. Computers & industrial engineering. https://doi.org/10.1016/j.cie.2013.09.017
Almehdawe E, Jewkes B, He QM (2013) A Markovian queueing model for ambulance offload delays. Eur J Oper Res 226:602–614
Takeda RA, Widmer JA, Morabito R (2007) Analysis of ambulance decentralization in an urban emergency medical service using the hypercube queueing model. Comput Oper Res 34:727–741. https://doi.org/10.1016/j.cor.2005.03.022
Singer M, Donoso P (2008) Assessing an ambulance service with queuing theory. Computers & operations research
Restrepo M, Henderson S, Topaloglu H (2009) Erlang loss models for the static deployment of ambulances. Health Care Manag Sci 12:67–79. https://doi.org/10.1007/s10729-008-9077-4
Spaite D, Benoit R, Brown D, Cales R, Kaufmann C, Pollock D, Yano EM, Ryan S, Glass C, Dawson D (1995) Uniform pre-hospital data elements and definitions: a report from the uniform pre-hospital emergency medical services data conference. Ann Emerg Med 25:525–534. https://doi.org/10.1016/S0196-0644(95)70271-7
Mason AJ (2013) Simulation and real-time optimised relocation for improving ambulance operations. In: Denton BT (ed) Handbook of healthcare operations management: methods and applications. Springer, New York, NY
Pinto LR, Silva PMS, Young TP (2015) A generic method to develop simulation models for ambulance systems. Simul Model Pract Theory 51:170–183. https://doi.org/10.1016/j.simpat.2014.12.001
Fomundam S, Herrmann J (2007) A survey of queuing theory applications in healthcare. The Institute for systems research
Brotcorne L, Laporte G, Semet F (2003) Ambulance location and relocation models. Eur J Oper Res 147:451–463. https://doi.org/10.1016/S0377-2217(02)00364-8
Cone DC, Davidson SJ, Nguyen Q (1998) A time-motion study of the emergency medical services turnaround interval. Ann Emerg Med 31:241–246
Cooney DR, Millin MG, Carter A, Lawner BJ, Nable JV, Wallus HJ (2011) Ambulance diversion and emergency department offload delay: resource document for the National Association of EMS physicians position statement. Prehosp Emerg Care 15:555–561. https://doi.org/10.3109/10903127.2011.608871
Carter AJ, Overton J, Terashima M, Cone DC (2014) Can emergency medical services use turnaround time as a proxy for measuring ambulance offload time? J Emerg Med 47:30–35. https://doi.org/10.1016/j.jemermed.2013.08.109
Spaite DW, Valenzuela TD, Meislin HW, Criss EA, Hinsberg P (1993) Prospective validation of a new model for evaluating emergency medical services systems by in-field observation of specific time intervals in prehospital care. Ann Emerg Med 22:638–645
Crilly J, Keijzers G, Tippett V, O'Dwyer J, Lind J, Bost N, O'Dwyer M, Shiels S, Wallis M (2015) Improved outcomes for emergency department patients whose ambulance off-stretcher time is not delayed. Emerg Med Australas 27:216–224. https://doi.org/10.1111/1742-6723.12399
Eckstein M, Isaacs SM, Slovis CM, Kaufman BJ, Loflin JR, O'Connor RE, Pepe PE (2005) Facilitating EMS turnaround intervals at hospitals in the face of receiving facility overcrowding. Prehosp Emerg Care 9:267–275. https://doi.org/10.1080/10903120590962102
Patient handover delays being addressed by ambulance service(2012) . Nurs Stand https://doi.org/10.7748/ns.26.48.10.s15
Majedi M (2008) A queueing model to study ambulance offload delays. Dissertation or thesis. University of Waterloo, Canada
Almehdawe E, Jewkes B, He QM (2016) Analysis and optimization of an ambulance offload delay and allocation problem. Omega-International Journal of Management Science
Eckstein M, Chan LS (2004) The effect of emergency department crowding on paramedic ambulance availability. Ann Emerg Med 43:100–105. https://doi.org/10.1016/s0196064403007479
Segal E, Verter V, Colacone A, Afilalo M (2006) The in-hospital interval: a description of EMT time spent in the emergency department. Prehosp Emerg Care 10:378–382. https://doi.org/10.1080/10903120600725884
Silvestri S, Ralls GA, Sun J, Shah KJ, Parrish GA (2006) Evaluation of patients in delayed emergency medical services unit off-load status. Acad Emerg Med 13:S70
Cone DC, Middleton PM, Marashi Pour S (2012) Analysis and impact of delays in ambulance to emergency department handovers. Emerg Med Australas 24:525–533. https://doi.org/10.1111/j.1742-6723.2012.01589.x
Cooney DR, Wojcik S, Seth N, Vasisko C, Stimson K (2013) Evaluation of ambulance offload delay at a university hospital emergency department. Int J Emerg Med 6:15. https://doi.org/10.1186/1865-1380-6-15
Hammond E, Holzhauser K, Shaban R, Melton N (2009) An exploratory study to examine the phenomenon and practice of 'Ambulance Ramping' at hospitals within the southern health service districts of Queensland and Queensland ambulance service. Australas Emerg Nurs J 12:170. https://doi.org/10.1016/j.aenj.2009.08.060
Taylor C, Williamson D, Sanghvi A (2006) When is a door not a door? The difference between documented and actual arrival times in the emergency department. Emerg Med J 23:442–443. https://doi.org/10.1136/emj.2005.029868
Steer S, Bhalla MC, Zalewski J, Frey J, Nguyen V, Mencl F (2016) Use of radio frequency identification to establish emergency medical service offload times. Prehosp Emerg Care 20:254–259. https://doi.org/10.3109/10903127.2015.1076093
Cooney DR, Wojcik S, Seth N (2011) Can NEDOCS score be used to predict ambulance offload delay? Ann Emerg Med 58:S217
Cooney DR, Vasisko C, Stimson K, Wojcik S (2013) Analysis of ambulance offload delay at an academic level 1 trauma center with adult and pediatric emergency departments. Ann Emerg Med 62:S2
Richardson DB, Mountain D (2009) Myths versus facts in emergency department overcrowding and hospital access block. Med J Aust
Silvestri S, Ralls GA, Papa L, Barnes M (2006) Impact of emergency department bed capacity on emergency medical services unit off-load time. Acad Emerg Med 13:S70
Lee YJ, Shin SD, Lee EJ, Cho JS, Cha WC (2015) Emergency department overcrowding and ambulance turnaround time. PLoS One 10:e0130758. https://doi.org/10.1371/journal.pone.0130758
Almehdawe E (2012) Queueing network models of ambulance offload delays. University of Waterloo, Dissertation or thesis
Derlet RW, Richards JR (2000) Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med 35:63–68
Fatovich DM, Hirsch RL (2003) Entry overload, emergency department overcrowding, and ambulance bypass. Emerg Med J 20:406–409. https://doi.org/10.1136/emj.20.5.406
El Sayed M, Mitchell PM, White LF, Rubin-Smith J, Maciejko TM, Obendorfer DT, Ulrich AS, Dyer S, Olshaker JS (2012) Impact of an emergency department closure on the local emergency medical services system. Prehosp Emerg Care https://doi.org/10.3109/10903127.2011.640418, 16, 198, 203
Richardson LD, Asplin BR, Lowe RA (2002) Emergency department crowding as a health policy issue: past development, future directions. Ann Emerg Med 40:388–393. https://doi.org/10.1067/mem.2002.128012
Schafermeyer RW, Asplin BR (2003) Hospital and emergency department crowding in the United States. Emerg Med 15:22–27. https://doi.org/10.1046/j.1442-2026.2003.00403.x
Ay D (2010) Patient population and factors determining length of stay in adult ED of a Turkish university medical center. Am J Emerg Med 28:325–330. https://doi.org/10.1016/j.ajem.2008.12.011
Hoot NR, Aronsky D (2008) Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med 52:126–136.e1. https://doi.org/10.1016/j.annemergmed.2008.03.014
Derlet RW, Richards JR, Kravitz RL (2001) Frequent overcrowding in U.S. emergency departments. Acad Emerg Med 8:151–155. https://doi.org/10.1111/j.1553-2712.2001.tb01280.x
Schwartz B, Hospital emergency department and ambulance effectiveness working Group (2005) Improving access to emergency services: a system commitment
Derlet RW, Richards JR (2002) Emergency department overcrowding in Florida, New York, and Texas. South Med J 95:846–849
Olshaker JS, Rathlev NK (2006) Emergency department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the emergency department. J Emerg Med 30:351–356. https://doi.org/10.1016/j.jemermed.2005.05.023
Schull MJ, Lazier K, Vermeulen M, Mawhinney S, Morrison LJ (2003) Emergency department contributors to ambulance diversion: a quantitative analysis. Ann Emerg Med 41:467–476. https://doi.org/10.1067/mem.2003.23
Moskop JC, David PS, Gelderman JM, Schears RM, Bookman KJ (2009) Emergency department crowding, part 1--concept, causes, and moral consequences. Ann Emerg Med 53:605–611. https://doi.org/10.1016/j.annemergmed.2008.09.019
Yancer DA, Foshee D, Cole H, Beauchamp R, de lP, Keefe T, Smith W, Zimmerman K, Lavine M, Toops B (2006) Managing capacity to reduce emergency department overcrowding and ambulance diversions. Jt Comm J Qual Patient Saf
Andrulis DP, Kellermann A, Hintz EA, Hackman BB, Weslowski VB (1991) Emergency departments and crowding in United States teaching hospitals. Ann Emerg Med 20:980–986
Schneider S, Zwemer F, Doniger A, Dick R, Czapranski T, Davis E (2001) Rochester, New York: a decade of emergency department overcrowding. Acad Emerg Med 8:1044–1050
Cameron PA, Joseph AP, McCarthy SM (2009) Access block can be managed. Med J Aust
Olshaker JS (2009) Managing emergency department overcrowding. Emerg Med Clin North Am 27:593–603. https://doi.org/10.1016/j.emc.2009.07.004
Esensoy AV (2008) Evaluation of the demonstration project to direct low acuity ambulance patients to urgent care centres to improve ambulance availability. University of Toronto (Canada), Dissertation or Thesis
Perry M, Carter D (2017) The ethics of ambulance ramping. Emerg Med Australas 29:116–118. https://doi.org/10.1111/1742-6723.12625
Ting JY (2008) The potential adverse patient effects of ambulance ramping, a relatively new problem at the interface between prehospital and ED care. J Emerg Trauma Shock 1:129. https://doi.org/10.4103/0974-2700.43201
Carter AJ, Gould JB, Vanberkel P, Jensen JL, Cook J, Carrigan S, Wheatley MR, Travers AH (2015) Offload zones to mitigate emergency medical services (EMS) offload delay in the emergency department: a process map and hazard analysis. CJEM 17:670–678. https://doi.org/10.1017/cem.2015.15
Hamilton TE (2006) "parking" of emergency medical service patients in hospitals. U.S. Department of Health and Human Services
Hitchcock M, Crilly J, Gillespie B, Chaboyer W, Tippett V, Lind J (2010) The effects of ambulance ramping on emergency department length of stay and in-patient mortality. Australas Emerg Nurs J 13:17–24. https://doi.org/10.1016/j.aenj.2010.02.004
Kingswell C, Shaban RZ, Crilly J (2015) The lived experiences of patients and ambulance ramping in a regional Australian emergency department: an interpretive phenomenology study. Australas Emerg Nurs J 18:182–189. https://doi.org/10.1016/j.aenj.2015.08.003
Smith L (2013) Modelling Emerg Med Serv Dissertation or Thesis. In: Cardiff University
Schwartz B (2015) Transfer of care and offload delay: continued resistance or integrative thinking? CJEM 17:679–684. https://doi.org/10.1017/cem.2014.62
Nova Scotia Capital District Health Authority (2015) Quarterly performance report emergency departments and system flow. In. http://www.cdha.nshealth.ca/about-us-39
Laan CM, Vanberkel PT, Boucherie RJ, Carter AJE (2016) Offload zone patient selection criteria to reduce ambulance offload delay. Operations Research for Health Care
Newell K (2013) Offload delay - returning paramedic unit hours to the street: the Ottawa approach. Canadian Paramedicine
Clarey A, Allen M, Brace-McDonnell S, Cooke MW (2014) Ambulance handovers: can a dedicated ED nurse solve the delay in ambulance turnaround times? Emerg Med J 31:419–420. https://doi.org/10.1136/emermed-2012-202258
Greaves T, Mitchell M, Zhang P, Crilly J (2017) The impact of an emergency department ambulance offload nurse role: a retrospective comparative study. Int Emerg Nurs 32:39–44. https://doi.org/10.1016/j.ienj.2016.12.005
Han JH, Zhou C, France DJ, Zhong S, Jones I, Storrow AB, Aronsky D (2007) The effect of emergency department expansion on emergency department overcrowding. Acad Emerg Med 14:338–343. https://doi.org/10.1197/j.aem.2006.12.005
Crilly J, O'Dwyer J, Lind J, Tippett V, Thalib L, O'Dwyer M, Keijzers G, Wallis M, Bost N, Shiels S (2013) Impact of opening a new emergency department on healthcare service and patient outcomes: analyses based on linking ambulance, emergency and hospital databases. Intern Med J 43:1293–1303. https://doi.org/10.1111/imj.12202
Crilly JL, Keijzers GB, Tippett VC, O'Dwyer JA, Wallis MC, Lind JF, Bost NF, O'Dwyer MA, Shiels S (2014) Expanding emergency department capacity: a multisite study. Aust Health Rev 38:278–287. https://doi.org/10.1071/ah13085
Lee IH, Chen CT, Lee YT, Hsu YS, Lu CL, Huang HH, Hsu TF, How CK, Yen DH, Yang UC (2017) A new strategy for emergency department crowding: high-turnover utility bed intervention. J Chin Med Assoc 80:297–302. https://doi.org/10.1016/j.jcma.2016.11.002
Alberta Health Services (2010) AHS launches overcapacity protocols. In: http://www.albertahealthservices.ca/news/releases/2010/Page3376.aspx. Accessed Sep 20, 2017
McRae A, Wang D, Blanchard IE, Almansoori W, Lang E, Innes G, Anton A (2012) Benefits on EMS offload delay of a provincial ED overcapacity protocol aimed at reducing ED boarding. Alberta Health Services; University of Calgary
Lagoe RJ, Jastremski MS (1990) Relieving overcrowded emergency departments through ambulance diversion. Hosp Top 68:23–27
Deo S, Gurvich I (2011) Centralized vs. decentralized ambulance diversion: a network perspective. Management Science
Lagoe RJ, Hunt RC, Nadle PA, Kohlbrenner JC (2002) Utilization and impact of ambulance diversion at the community level. Prehosp Emerg Care
Burt CW, McCaig LF, Valverde RH (2006) Analysis of ambulance transports and diversions among US emergency departments. Ann Emerg Med 47:317–326. https://doi.org/10.1016/j.annemergmed.2005.12.001
Warden CR, Bangs C, Norton R, Huie J (2003) Temporal trends in ambulance diversion in a mid-sized metropolitan area. Prehosp Emerg Care
Kuruvilla A (2005) Predicting ambulance diversion. University of Louisville, Dissertation or Thesis
Leegon J, Hoot N, Aronsky D, Storkey A (2007) Predicting ambulance diversion in an adult emergency department using a Gaussian process. AMIA Annu Symp Proc
Hagtvedt R, Ferguson M, Griffin P, Jones GT, Keskinocak P (2009) Cooperative strategies to reduce ambulance diversion. Proceedings of the 2009 Winter Simulation Conference:1861–1874
Ramirez-Nafarrate A, Fowler JW, Wu T (2011) Design of centralized ambulance diversion policies using simulation-optimization. Proceedings of the 2011 Winter Simulation Conference:1251–1262
Ramirez-Nafarrate A, Hafizoglu AB, Gel ES, Fowler JW (2014) Optimal control policies for ambulance diversion. Eur J Oper Res 236:298–312
Lin CH, Kao CY, Huang CY (2015) Managing emergency department overcrowding via ambulance diversion: a discrete event simulation model. J Formos Med Assoc 114:64–71. https://doi.org/10.1016/j.jfma.2012.09.007
Kao CY, Yang JC, Lin CH (2015) The impact of ambulance and patient diversion on crowdedness of multiple emergency departments in a region. PLoS One 10:e0144227. https://doi.org/10.1371/journal.pone.0144227
Scheulen JJ, Li G, Kelen GD (2001) Impact of ambulance diversion policies in urban, suburban, and rural areas of Central Maryland. Acad Emerg Med 8:36–40
Carter AJ, Grierson R (2007) The impact of ambulance diversion on EMS resource availability. Prehosp Emerg Care 11:421–426. https://doi.org/10.1080/10903120701536909
Asplin BR (2003) Does ambulance diversion matter? Ann Emerg Med 41:477–480. https://doi.org/10.1067/mem.2003.112
Redd JM, Bair AE, Jayaraman S (2003) Implications of ambulance diversion. Ann Emerg Med
Nakajima Y, Vilke GM (2015) Editorial: ambulance diversion: the con perspective. Am J Emerg Med 33:818–819. https://doi.org/10.1016/j.ajem.2015.03.005
Redelmeier DA, Blair PJ, Collins WE (1994) No place to unload: a preliminary analysis of the prevalence, risk factors, and consequences of ambulance diversion. Ann Emerg Med 23:43–47
Mund E (2011) Ending ambulance diversion. Eighteen hospitals in King County, Wash., work toward a perpetual zero-divert status. EMS World
Vilke GM, Brown L, Skogland P, Simmons C, Guss DA (2004) Approach to decreasing emergency department ambulance diversion hours. J Emerg Med 26:189–192. https://doi.org/10.1016/j.jemermed.2003.07.003
Shealy RM, Sorrell JF, French DM (2014) Ambulance diversion by cooperation: a positive experience with a physician-directed ambulance diversion policy in Charleston County. South Carolina Ann Emerg Med 64:97–98. https://doi.org/10.1016/j.annemergmed.2014.03.021
Glushak C, Delbridge TR, Garrison HG (1997) Ambulance diversion. Prehosp Emerg Care 1:100–103
McConnell KJ, Richards CF, Daya M, Weathers CC, Lowe RA (2006) Ambulance diversion and lost hospital revenues. Ann Emerg Med 48:702–710. https://doi.org/10.1016/j.annemergmed.2006.05.001
Williams RM (2006) Ambulance diversion: economic and policy considerations. Ann Emerg Med 48:711–712. https://doi.org/10.1016/j.annemergmed.2006.06.009
Weaver J (2007) ED overcrowding and ambulance diversion cause potential liabilities. ED Legal Letter
Upfold J (2002) Emergency department overcrowding: ambulance diversion and the legal duty to care. CMAJ
Litzenburg TA, Dorsey NB (2011) Ambulance diversion: solution or problem?. ED Legal Letter
Geiderman JM, Marco CA, Moskop JC, Adams J, Derse AR (2015) Ethics of ambulance diversion. Am J Emerg Med 33:822–827. https://doi.org/10.1016/j.ajem.2014.12.002
Adkins EJ, Werman HA (2015) Ambulance diversion: ethical dilemma and necessary evil. Am J Emerg Med 33:820–821. https://doi.org/10.1016/j.ajem.2015.03.007
Brennan JA, Allin DM, Calkins AM, Enguidanos ER, Heimbach LJ, Pruden JN Sr, Stilley DG (2000) Guidelines for ambulance diversion. American College of Emergency Physicians. Ann Emerg Med
Khaleghi M, Loh A, Vroman D, Chan TC, Vilke GM (2007) The effects of minimizing ambulance diversion hours on emergency departments. J Emerg Med 33:155–159. https://doi.org/10.1016/j.jemermed.2007.02.014
Lindstrom A (2009) Always open: study finds no adverse effects from stopping ambulance diversion. In: JEMS: journal of emergency medical services
Friedman FD, Rathlev NK, White L, Epstein SK, Sayah A, Pearlmutter M, Biddinger P, Zane R, Moyer P (2011) Trial to end ambulance diversion in Boston: report from the conference of the Boston teaching hospitals consortium. Prehosp Disaster Med 26:122–126. https://doi.org/10.1017/s1049023x11000070
Patel PB, Vinson DR (2012) Ambulance diversion reduction and elimination: the 3–2-1 plan. J Emerg Med. https://doi.org/10.1016/j.jemermed.2012.01.031
Patel PB, Derlet RW, Vinson DR, Williams M, Wills J (2006) Ambulance diversion reduction: the Sacramento solution. Am J Emerg Med 24:206–213. https://doi.org/10.1016/j.ajem.2005.09.005
Al Darrab A, Fernandes CM, Worster A, Woolfrey K, Moneta S (2005) A city wide approach to reduce ambulance diversion: the Hamilton model. Ann Emerg Med
Vilke GM, Castillo EM, Stepanski BM, Murrin PA, Upledger-Ray L, Metz MA, Chan TC (2006) San Diego county patient destination trial to decrease ambulance diversion hours: three year follow-up. Ann Emerg Med
Poliakoff R, Vilke GM (2005) New ambulance policy slashes diversion hours: average number of patients drops 70%. ED Management
Holley J (2003) Memphis adopts no-ambulance-diversion policy: simple strategy returns rich rewards. EMS Insider
Rathlev NK, Blank F, Osborne B, Kellogg A, Li H, Blanchet J, Conway RF, Durkin L, Gerstein R, Strzempko S, Vig M, Santoro JP, Visintainer P (2013) No diversion in Western Massachusetts. J Emerg Med 44:313–320. https://doi.org/10.1016/j.jemermed.2012.06.017
Burke LG, Joyce N, Baker WE, Biddinger PD, Dyer KS, Friedman FD, Imperato J, King A, Maciejko TM, Pearlmutter MD, Sayah A, Zane RD, Epstein SK (2013) The effect of an ambulance diversion ban on emergency department length of stay and ambulance turnaround time. Ann Emerg Med 61:303–311.e1. https://doi.org/10.1016/j.annemergmed.2012.09.009
O'Keefe SD, Bibi S, Rubin-Smith J, Feldman J (2014) "no diversion": a qualitative study of emergency medicine leaders in Boston, MA, and the effects of a statewide diversion ban policy. Ann Emerg Med 63:589–597.e7. https://doi.org/10.1016/j.annemergmed.2013.09.007
Burke L (2010) Ending ambulance diversion in Massachusetts. Virtual Mentor 12:483–486. https://doi.org/10.1001/virtualmentor.2010.12.6.pfor2-1006
Beechner PM (2013) A fuzzy inference system for preventing ambulance diversion in emergency departments. Dissertation or Thesis, State University of New York at Binghamton
El-Masri S, Saddik B (2012) An emergency system to improve ambulance dispatching, ambulance diversion and clinical handover communication-a proposed model. J Med Syst 36:3917–3923. https://doi.org/10.1007/s10916-012-9863-x
McLeod B, Zaver F, Avery C, Martin DP, Wang D, Jessen K, Lang ES (2010) Matching capacity to demand: a regional dashboard reduces ambulance avoidance and improves accessibility of receiving hospitals. Acad Emerg Med 17:1383–1389. https://doi.org/10.1111/j.1553-2712.2010.00928.x
Castillo EM, Vilke GM, Williams M, Turner P, Boyle J, Chan TC (2011) Collaborative to decrease ambulance diversion: the California emergency department diversion project. J Emerg Med 40:300–307. https://doi.org/10.1016/j.jemermed.2010.02.023
Barthell EN, Foldy SL, Pemble KR, Felton CW, Greischar PJ, Pirrallo RG, Bazan WJ (2003) Assuring community emergency care capacity with collaborative internet tools: the Milwaukee experience. J Public Health Manag Pract
Lagoe RJ, Kohlbrenner JC, Hall LD, Roizen M, Nadle PA, Hunt RC (2003) Reducing ambulance diversion: a multihospital approach. Prehosp Emerg Care
Strear C, Vissers R, Yoder E, Barnett H, Shanks T, Jones L (2010) Applying the theory of constraints to emergency department workflow: reducing ambulance diversion through basic business practice. Ann Emerg Med 56:S11
Asamoah OK, Weiss SJ, Ernst AA, Richards M, Sklar DP (2008) A novel diversion protocol dramatically reduces diversion hours. Am J Emerg Med 26:670–675. https://doi.org/10.1016/j.ajem.2007.10.020
Pham JC, Patel R, Millin MG, Kirsch TD, Chanmugam A (2006) The effects of ambulance diversion: a comprehensive review. Acad Emerg Med 13:1220–1227. https://doi.org/10.1197/j.aem.2006.05.024
Delgado MK, Meng LJ, Mercer MP, Pines JM, Owens DK, Zaric GS (2013) Reducing ambulance diversion at hospital and regional levels: systemic review of insights from simulation models. West J Emerg Med 14:489–498. https://doi.org/10.5811/westjem.2013.3.12788
Shah MN, Fairbanks RJ, Maddow CL, Lerner EB, Syrett JI, Davis EA, Schneider SM (2006) Description and evaluation of a pilot physician-directed emergency medical services diversion control program. Acad Emerg Med 13:54–60. https://doi.org/10.1197/j.aem.2005.07.026
Larson G (2008) Ambulance destination determination system for ambulance distribution as an alternative to ambulance diversion. J Emerg Nurs 34:357–358. https://doi.org/10.1016/j.jen.2008.04.004
Halliday MH, Bouland AJ, Lawner BJ, Comer AC, Ramos DC, Fletcher M (2016) The medical duty officer: an attempt to mitigate the ambulance at-hospital interval. West J Emerg Med 17:662–668. https://doi.org/10.5811/westjem.2016.7.30266
Snooks H, Foster T, Nicholl J (2004) Results of an evaluation of the effectiveness of triage and direct transportation to minor injuries units by ambulance crews. Emerg Med J 21:105–111
Clawson JJ (1988) Principles of emergency medical dispatch. Englewood Cliffs, N.J.: Prentice-Hall, Englewood Cliffs, N.J
Shah MN, Bishop P, Lerner EB, Czapranski T, Davis EA (2003) Derivation of emergency medical services dispatch codes associated with low - acuity patients. Prehospital Emergency Care 7:434–439. https://doi.org/10.1080/312703002132
Shah MN, Bishop P, Lerner EB, Fairbanks RJ, Davis EA (2005) Validation of using EMS dispatch codes to identify low-acuity patients. Prehospital Emergency Care 9:24–31. https://doi.org/10.1080/10903120590891651
Woollard M (2003) Emergency calls not requiring an urgent ambulance response: expert consensus. Prehospital Emergency Care 7:384–391. https://doi.org/10.1080/10903120390936626
Villarreal M, Leach J, Kandala N, Dale J (2017) Can a partnership between general practitioners and ambulance services reduce conveyance to emergency care? Emerg Med J 34:459–465. https://doi.org/10.1136/emermed-2015-204924
Millin MG, Brown LH, Schwartz B (2011) EMS provider determinations of necessity for transport and reimbursement for EMS response, medical care, and transport: combined resource document for the National Association of EMS physicians position statements. Prehosp Emerg Care. 15:562–569. https://doi.org/10.3109/10903127.2011.598625
Snooks HA, Dale J, Hartley-Sharpe C, Halter M (2004) On-scene alternatives for emergency ambulance crews attending patients who do not need to travel to the accident and emergency department: a review of the literature. Emerg Med J 21:212–215. https://doi.org/10.1136/emj.2003.005199
Schaefer RA, Rea TD, Plorde M, Peiguss K, Goldberg P, Murray JA (2002) An emergency medical services program of alternate destination of patient care. Prehospital Emergency Care. 6:309–314. https://doi.org/10.1080/10903120290938355
Acknowledgements
The authors thank Leah Boulos, Evidence Synthesis Coordinator at the Maritime SPOR SUPPORT Unit, for her support with the literature search and journal article extraction for this review.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(PDF 391 kb)
Appendix
Appendix
1.1 1. Abbreviations
- AD:
-
Ambulance diversion
- AOD:
-
Ambulance offload delay
- CTAS:
-
Canadian emergency department Triage and acuity scale
- ED:
-
Emergency department
- EMS:
-
Emergency medical services
- NEDOCS:
-
National emergency department Overcrowding scale
- LOS:
-
Length of stay
- OCP:
-
Overcapacity protocol
- OR:
-
Operations research
- OZ:
-
Offload zone
1.2 2. Search Strategy Example (PubMed)
ambulance offload[tiab] OR ambulance diversion[tiab] OR ambulance ramping[tiab] OR ambulance handover[tiab] OR ambulance availability[tiab] OR offload delay[tiab] OR offload time*[tiab] OR offload zone*[tiab] OR turnaround interval*[tiab] OR hospital interval*[tiab]
Rights and permissions
About this article
Cite this article
Li, M., Vanberkel, P. & Carter, A.J.E. A review on ambulance offload delay literature. Health Care Manag Sci 22, 658–675 (2019). https://doi.org/10.1007/s10729-018-9450-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-018-9450-x