Abstract
In this paper we propose an empirically implementable measure of aggregate-level efficiency along the lines of Debreu’s (1951) coefficient of resource utilization but restricted to the production side. The efficiency measure is based on directional distance functions, which allows the overall measure of efficiency to be decomposed into measures of technical and “structural” efficiency. The latter measure, which captures inefficiencies associated with the organization of production within an industry, is further decomposed into measures of scale and mix efficiency. The measures developed in the paper are illustrated using U.S. hospital data. The illustration sheds light on the efficacy of certificate of need (CON) regulations.







Similar content being viewed by others
Notes
Over time other payers followed Medicare’s lead in shifting from FFS to PPS in an effort to contain costs. The Balanced Budget Act of 1997 furthered the transition from FFS to PPS.
See Färe and Grosskopf [11] for an excellent exposition of directional distance functions; in particular, see essay 3 for a discussion of aggregation issues.
Given the ability of resources to move across particular industries or sectors of the economy, Debreu’s first source of inefficiency—underemployment of resources—does not apply at the industry/sectoral level.
Farrell [8] argued that the same approach he proposed for measuring the efficiency of firms (in our case, hospitals) could also be applied to measuring the efficiency of industries. Noting, however, that it may be difficult to find comparable cross-country data for performing industry efficiency analyses, he suggested “…a very satisfactory way of getting around this [data] problem: that is, by comparing an industry’s performance with the efficient production function derived from its own constituent firms” [6, p. 262]. Farrell termed this “technical efficiency” measure “structural efficiency,” and argued that it measured how well an industry performed relative to its best firms, which was a matter of firms being of scale and technically efficient and output being optimally allocated across producers. We borrow Farrell’s term, “structural efficiency,” but separate it from technical efficiency, so that it is more in line with Debreu’s [7] notion of “efficiency of organization.” Thus, our decomposition of overall inefficiency into technical and structural components (with the latter have mix and scale sub-components) is consistent with Debreu’s original decomposition of the CRU.
As defined by Farrell [8], output served as the weight. However, this approach is restricted to the very limited case of a single-output technology.
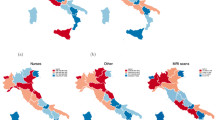
Many hospital regulations—including the certificate of need (CON) program which is the focus of our empirical illustration—and a considerable amount of hospital revenue are determined at the state level, making this an appropriate level of aggregation.
This aggregation of firm level technology to form industry level technology is formally presented in the next subsection of the paper.
CRS is defined here as the minimum of the average cost curve; i.e., the most productive scale size which is the typical measure of scale efficiency from an economics perspective.
This decomposition is analogous to the decomposition of firm level efficiency measures into its constituents.
The 14 states that have discontinued CON regulation are Arizona, California, Colorado, Idaho, Indiana, Kansas, Minnesota, New Mexico, North Dakota, Pennsylvania, South Dakota, Texas, Utah, and Wyoming.
As pointed out by an anonymous referee, there are many ways to measure the scale and size of complex organizations such as hospitals (see [33] for an excellent treatment of this issue).
See O’Neill et al. [34] for a systematic analysis of hospital efficiency studies, including the specifications of inputs and outputs used in these studies.
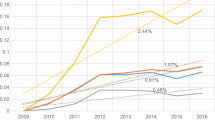
There is no graph for structural inefficiency over time since it is derived by the sum of the mix and the scale efficiencies.
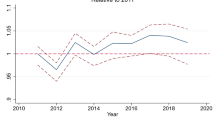
We do not use the Malmquist approach since it is based on the DEA approach and is radial in nature, we cannot aggregate results from the Malmquist as we can in the distance function by year.
References
Brown LD, Sparer MS (2001) Window shopping: state health reform politics in 1990. Health Aff 20(1):50–67. doi:10.1377/hlthaff.20.1.50
Hacker JS, Skocpol T (1997) The new politics of U.S. health policy. J Health Polit Policy Law 22(2):315–337
Oliver TR, Paul-Shaheen P (1997) Translating ideas into actions: entrepreneurial leadership in state health care reforms. J Health Polit Policy Law 22(3):721–786
Saltman RB (2002) Regulating incentives: the past and present role of the state in health care systems. Soc Sci Med 54(11):1677–1684. doi:10.1016/S0277-9536(01)00335-5
Governor’s Health Care Proposal (2007) www.commonwealthfund.org/Content/Innovations/State-Profiles/2007/Mar/California-Governors-Health-Care-Proposal.aspx
The National Health Planning and Resources Development Act, 88 Stat. 2229, 42 U.S.C. §3001, 1976
Debreu G (1951) The coefficient of resource utilization. Econometrica 19(3):273–292. doi:10.2307/1906814
Farrell MJ (1957) The measurement of productive efficiency. J R Stat Soc [Ser A] 120(3):253–290. doi:10.2307/2343100
Charnes A, Cooper WW, Rhodes E (1978) Measuring the efficiency of decision making units. Eur J Oper Res 2(4):429–444. doi:10.1016/0377-2217(78)90138-8
Färe R, Grosskopf S, Lovell CAK (1985) The measurement of production efficiency. Kluwer-Nijhoff, Boston
Färe R, Grosskopf S (2004) New directions: efficiency and productivity. Kluwer Academic, Boston
Førsund FR, Hjalmarsson L (1979) Generalized farrell measures of efficiency: an application to milk processing in Swedish dairy plants. Econ J 89(354):294–315. doi:10.2307/2231603
Bjurek H, Hjalmarsson L, Försund F (1990) Deterministic parametric and nonparametric estimation of efficiency in service production: a comparison. J Econom 46(1/2):213–227. doi:10.1016/0304-4076(90)90056-Y
Torgensen A, Førsund F, Kittelsen S (1996) Slack-adjusted efficiency measures and ranking of efficient units. J Prod Anal 7(4):379–397. doi:10.1007/BF00162048
Ylvinger S (2000) Industry performance and structural efficiency measures: solutions to problems in firm models. Eur J Oper Res 121(1):164–174. doi:10.1016/S0377-2217(99)00014-4
Koopmans TC (1957) Three essays on the state of economic analysis. McGraw-Hill, New York
Färe R, Grosskopf S, Knox Lovell CA (1994) Production frontiers. Cambridge University Press, New York
Li S-K, Ng YC (1995) Measuring the productive efficiency of a group of firms. Int Adv Econ Res 1(4):377–390. doi:10.1007/BF02295790
Chambers RG, Chung Y, Färe R (1998) Profit, directional distance functions and Nerlovian efficiency. J Optim Theory Appl 98(2):351–364. doi:10.1023/A:1022637501082
Briec W (1997) A graph-type extension of Farrell technical efficiency measure. J Prod Anal 8(1):95–110. doi:10.1023/A:1007728515733
Førsund FR, Lovell CAK, Schmidt P (1980) A survey of frontier production functions and their relationship to efficiency measurement. J Econom 13(1):5–25. doi:10.1016/0304-4076(80)90040-8
Owens P, Elixhauser A (2006) “Hospital Admissions That Began in the Emergency Department, 2003” Healthcare Cost and Utilization Project, Statistical Brief #1, February 2006. Agency for Healthcare Research and Quality, Rockville, MD. (http://hcup-us.ahrq.gov/reports/statbriefs/sb1.pdf)
Sloan FA (1981) Regulation and the rising cost of hospital care. Rev Econ Stat 63(4):479–487. doi:10.2307/1935842
Mayo JW, McFarland DA (1989) Regulation, market structure, and hospital costs. South Econ J 55(3):559–569. doi:10.2307/1059572
Conover CJ, Sloan FA (1998) Does removing certificate-of-need regulations lead to a surge in health care spending? J Health Polit Policy Law 23(3):455–481
ICF-Lewin (2000) Report to Congress—Medicare Payment for Post-Surgical Recovery Care Centers, November
Graham GG, Cowing TG (1997) Hospital reserve margins: structural determinants and policy implications using cross-section data. South Econ J 63(3):692–709. doi:10.2307/1061103
Bates LJ, Mukherjee K, Santerre RE (2006) Market structure and technical efficiency in the hospital services sector: a DEA approach. Med Care Res Rev 63(4):499–524. doi:10.1177/1077558706288842
Foreman SE, Keeler TE (1995) Regulation, competition, and cross-subsidization of hospitals: lessons from the economics of regulation. University of California, Berkeley Working Papers, pp 95–236
Banks DA, Foreman SE, Keeler TE (1999) Cross-Subsidization in hospital care: some lessons from the law and economics of regulation. Health Matrix J Law-Medicine 9(1):1–35
Devers KJ, Brewster LR, Casalino LP (2003) Changes in hospital competition strategy: a new medical arms race? Health Serv Res 38(1, Part 2):447–469. doi:10.1111/1475-6773.00124
Berenson R, Bodenheimer T, Pham H (2006) Specialty-service lines: salvos in the new medical arms race. Health Aff 25(5):W337–W343. doi:10.1377/hlthaff.25.w337
Kimberly JR (1976) Organizational size and the structuralist perspective: a review, critique, and proposal. Adm Sci Q 21(4):571–597. doi:10.2307/2391717
O'Neill L, Rauner M, Heidenberger K, Kraus M (2008) A cross-national comparison and taxonomy of DEA-based hospital efficiency studies. Socioecon Plann Sci 42(3):158–189. doi:10.1016/j.seps.2007.03.001
Joskow PL (1980) The effects of competition and regulation on hospital bed supply and the reservation quality of the hospital. Bell J Econ 11(2):421–447. doi:10.2307/3003372
Acknowledgements
We wish to thank Professor Jan Clement (Department of Health Administration, Virginia Commonwealth University) for supplying the case mix indices for the hospitals in this paper and to the editor of the journal and anonymous referees for their suggestions that improved this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferrier, G.D., Leleu, H. & Valdmanis, V.G. The impact of CON regulation on hospital efficiency. Health Care Manag Sci 13, 84–100 (2010). https://doi.org/10.1007/s10729-009-9113-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-009-9113-z