Abstract
Glycation of amino acid residues in proteins leads to the eventual formation of advanced glycation end products (AGEs). AGE formation significantly influences human health and the aging process. AGE accumulation rates may be slowed by modifications to lifestyle or by pharmacological strategies. But the use of therapeutic drugs is not an appropriate means of controlling AGEs within the general population. However, phytochemical constituents in plant-based foods exhibit anti-glycation activities and may be more appropriate for general consumption. Among these phytochemicals are iridoids. The anti-AGE potential of iridoids has been demonstrated in vitro and in vivo, while also revealing possible mechanisms of action. Inclusion of iridoid food sources in the diet may be a useful component of strategies intended to mitigate AGE accumulation within the body.

Similar content being viewed by others
References
Luevano-Contreras C., Chapman-Novakofski K.: Dietary advanced glycation end products and aging. Nutrients. 2(12), 1247–1265 (2010)
Vlassara H., Palace M.R.: Diabetes and advanced glycation endproducts. J. Intern. Med. 251(2), 87–101 (2002)
Higgins P.J., Bunn H.F.: Kinetic analysis of the nonenzymatic glycosylation of hemoglobin. J. Biol. Chem. 256(10), 5204–5208 (1981)
Thornalley P.J., Langborg A., Minhas H.S.: Formation of glyoxal, methylglyoxal and 3-deoxyglucosone in the glycation of proteins by glucose. The Biochem. J. 344(1), 109–116 (1999)
Ulrich P., Cerami A.: Protein glycation, diabetes, and aging. Recent Prog. Horm. Res. 56, 1–21 (2001)
Miyata T., Wada Y., Cai Z., Iida Y., Horie K., Yasuda Y., Maeda K., Kurokawa K., van Ypersele de Strihou C.: Implication of an increased oxidative stress in the formation of advanced glycation end products in patients with end-stage renal failure. Kidney Int. 51(4), 1170–1181 (1997)
Brownlee M.: Biochemistry and molecular cell biology of diabetic complications. Nature. 414(6865), 913–820 (2001)
Ramasamy R.: Advanced glycation endproducts: from precursors to RAGE: round and round we go. Amino Acids. 42(4), 1151–1161 (2012)
Sing R., Barden A., Mori T., Beilin L.: Advanced glycation end-products: a review. Diabetologia. 44(2), 129–146 (2001)
Semba R.D., Nicklett E.J., Ferrucci L.: Does accumulation of advanced glycation end products contribute to the aging phenotype? J. Gerontol. A Biol. Sci. Med. Sci. 65(9), 963–975 (2010)
Wolffenbuttel B.H., van Haeften T.W.: Prevention of complications in non-insulin-dependent diabetes mellitus (NIDDM). Drugs. 50(2), 263–288 (1995)
Yamagishi S., Nakamura K., Matsui T., Ueda S., Noda Y., Imaizumi T.: Inhibitors of advanced glycation end products (AGEs): potential utility for the treatment of cardiovascular disease. Cardiovasc. Ther. 26(1), 50–58 (2008)
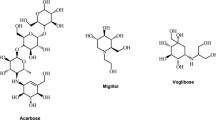
Alam A., Ahsan A., Alam S.: Newer insights in drugs inhibiting formation and accumulation of advanced glycation end products. J. Biochem. Tech. 5(1), 666–672 (2013)
Cerami C., Founds H., Nicholl I., Mitsuhashi T., Giordano D., Vanpatten S., Lee A., Al-Abed Y., Vlassara H., Bucala R., Cerami A.: Tobacco smoke is a source of toxic reactive glycation products. Proc. Natl. Acad. Sci. U. S. A. 94(25), 13915–13920 (1997)
Yamagishi S., Nakajima S., Uwaya A., Isami F.: Association between skin autofluorescence and food and lifestyle measured with the TruAge scanner. Pharma Medica. 31(10), 197–203 (2013) [Article in Japanese]
Nomoto K., Yagi M., Arita S., Ogura M., Yonei Y.: Skin Accumulation of Advanced Glycation End Products and Lifestyle Behaviors in Japanese. Anti-Aging Med. 9(6), 165–173 (2012)
Peng X., Ma J., Chen F., Wang M.: Naturally occurring inhibitors against the formation of advanced glycation end-products. Food Funct. 2(6), 289–301 (2011)
Nagai R., Shirakawa J., Ohno R., Moroishi N., Nagai M.: Inhibition of AGEs formation by natural products. Amino Acids. 46(2), 261–266 (2014)
Rahbar S., Figarola J.L.: Novel inhibitors of advanced glycation endproducts. Arch. Biochem. Biophys. 419(1), 63–79 (2003)
Odjakova M., Popova E., Al Sharif M., Mironova R.: Plant-Derived Agents with Anti-Glycation Activity. In: Petrescu S. (ed.) Glycosylation, pp. 223–256. InTech, Rijeka (2012)
Fujikawa T., Hirata T., Hosoo S., Nakajima K., Wada A., Yurugi Y., Soya H., Matsui T., Yamaguchi A., Ogata M., Nishibe S.: Asperuloside stimulates metabolic function in rats across several organs under high-fat diet conditions, acting like the major ingredient of Eucommia leaves with anti-obesity activity. J. Nutr. Sci. 1(e10), 1–11 (2012)
Li B., Zhang D.M., Luo Y.M., Chen X.G.: Three new and antitumor anthraquinone glycosides from Lasianthus acuminatissimus MERR. Chem. Pharm. Bull. (Tokyo). 54(3), 297–300 (2006)
Nakamura T., Nakazawa Y., Onizuka S., Satoh S., Chiba A., Sekihashi K., Miura A., Yasugahira N., Sasaki Y.F.: Antimutagenicity of Tochu tea (an aqueous extract of Eucommia ulmoides leaves): 1. The clastogen-suppressing effects of Tochu tea in CHO cells and mice. Mutat. Res. 388(1), 7–20 (1997)
Qiu J., Chi G., Wu Q., Ren Y., Chen C., Feng H.: Pretreatment with the compound asperuloside decreases acute lung injury via inhibiting MAPK and NFκB signaling in a murine model. Int. Immunopharmacol. 31, 109–115 (2016)
Kim D.H., Lee H.J., Oh Y.J., Kim M.J., Kim S.H., Jeong T.S., Baek N.I.: Iridoid glycosides isolated from Oldenlandia diffusa inhibit LDL-oxidation. Arch. Pharm. Res. 28(10), 1156–1160 (2005)
Ishiguro K., Yamaki M., Takagi S.: Studies on the iridoid related compounds. I. On the antimicrobial activity of aucubigenin and certain iridoid aglycones. Yakugaku Zasshi. 102(8), 755–759 (1982)
West B.J., Deng S., Jensen C.J.: Nutrient and phytochemical analyses of processed noni puree. Food Res. Int. 44(7), 2295–2301 (2011)
Wang M.Y., Peng L., Weidenbacher-Hoper V., Deng S., Anderson G., West B.J.: Noni juice improves serum lipid profiles and other risk markers in cigarette smokers. Scientific World Journal. 2012(article ID), 594657 (2012)
Wang X., Tang S., Zhai H., Duan H.: Studies on anti-tumor metastatic constituents from Ardisia crenata. Zhongguo Zhong Yao Za Zhi. 36(7), 881–885 (2011)
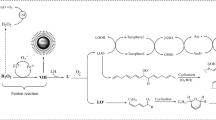
Ling S.K., Tanaka T., Kouno I.: Effects of iridoids on lipoxygenase and hyaluronidase activities and their activation by beta-glucosidase in the presence of amino acids. Biol. Pharm. Bull. 26(3), 352–356 (2003)
Akihisa T., Matsumoto K., Tokuda H., Yasukawa K., Seino K., Nakamoto K., Kuninaga H., Suzuki T., Kimura Y.: Anti-inflammatory and potential cancer chemopreventive constituents of the fruits of Morinda citrifolia (Noni). J. Nat. Prod. 70(5), 754–757 (2007)
Shim K.M., Choi S.H., Jeong M.J., Kang S.S.: Effects of aucubin on the healing of oral wounds. In Vivo. 21(6), 1037–1041 (2007)
Kang Z., Wu W.H., Wang J.J., Ouyang D.S.: Research advances in pharmacology of aucubin and aucubigenin. Zhongguo Zhong Yao Za Zhi. 32(24), 2585–2587 (2007)
Chang I.M.: Liver-protective activities of aucubin derived from traditional oriental medicine. Res. Commun. Mol. Pathol. Pharmacol. 102(2), 189–204 (1998)
Ha H., Ho J., Shin S., Kim H., Koo S., Kim I.H., Kim C.: Effects of Eucommiae Cortex on osteoblast-like cell proliferation and osteoclast inhibition. Arch. Pharm. Res. 26(11), 929–936 (2003)
Wan D., Xue L., Zhu H., Luo Y.: Catalpol induces neuroprotection and prevents memory dysfunction through the cholinergic system and BDNF. Evid. Based Complement. Alternat. Med. 2013(article ID), 134852 (2013)
Bao Q., Shen X., Qian L., Gong C., Nie M., Dong Y.: Anti-diabetic activities of catalpol in db/db mice. Korean J. Physiol. Pharmacol. 20(2), 153–160 (2016)
Yang, S., Deng, H., Zhang, Q., Xie, J., Zeng, H., Jin, X., Ling, Z., Shan, Q., Liu, M., Ma, Y., Tang, J., Wei, Q.: Amelioration of diabetic mouse nephropathy by catalpol correlates with down-regulation of Grb10 expression and activation of insulin-like growth factor 1/insulin-like growth factor 1 receptor signaling. PLoS One 11(3), article ID e0151857 (2016)
Tian Y.Y., Jiang B., An L.J., Bao Y.M.: Neuroprotective effect of catalpol against MPP(+)-induced oxidative stress in mesencephalic neurons. Eur. J. Pharmacol. 568(1–3), 142–148 (2007)
Huang W.J., Niu H.S., Lin M.H., Cheng J.T., Hsu F.L.: Antihyperglycemic effect of catalpol in streptozotocin-induced diabetic rats. J. Nat. Prod. 73(6), 1170–1172 (2010)
Kang D.G., Moon M.K., Lee A.S., Kwon T.O., Kim J.S., Lee H.S.: Cornuside suppresses cytokine-induced proinflammatory and adhesion molecules in the human umbilical vein endothelial cells. Biol. Pharm. Bull. 30(9), 1796–1799 (2007)
Song S.Z., Choi Y.H., Jin G.Y., Li G.Z., Yan G.H.: Protective effect of cornuside against carbon tetrachloride-induced acute hepatic injury. Biosci. Biotechnol. Biochem. 75(4), 656–661 (2011)
Li L., Jin G., Jiang J., Zheng M., Jin Y., Lin Z., Li G., Choi Y., Yan G.: Cornuside inhibits mast cell-mediated allergic response by down-regulating MAPK and NF-κB signaling pathways. Biochem. Biophys. Res. Commun. 473(2), 408–414 (2016)
Deng, S, West, BJ, Jensen, C.J.: UPLC-TOF-MS characterization and identification of bioactive iridoids in Cornus mas fruit. J. Anal. Methods Chem. 2013, article ID 710972 (2013)
Choi Y.H., Jin G.Y., Li G.Z., Yan G.H.: Cornuside suppresses lipopolysaccharide-induced inflammatory mediators by inhibiting nuclear factor-kappa B activation in RAW 264.7 macrophages. Biol. Pharm. Bull. 34(7), 959–966 (2011)
Jiang W.L., Zhang S.M., Tang X.X., Liu H.Z.: Protective roles of cornuside in acute myocardial ischemia and reperfusion injury in rats. Phytomedicine. 18(4), 266–271 (2011)
Jiang W.L., Chen X.G., Zhu H.B., Tian J.W.: Effect of cornuside on experimental sepsis. Planta Med. 75(6), 614–619 (2009)
Lin M.H., Liu H.K., Huang W.J., Huang C.C., Wu T.H., Hsu F.L.: Evaluation of the potential hypoglycemic and Beta-cell protective constituents isolated from Corni fructus to tackle insulin-dependent diabetes mellitus. J. Agric. Food Chem. 59(14), 7743–7751 (2011)
Wang M.Y., Peng L., Weidenbacher-Hoper V., Deng S., Anderson G., West B.J.: Noni juice improves serum lipid profiles and other risk markers in cigarette smokers. Sci. World J. 2012, Article ID 594657 (2012)
Ma D.L., Chen M., Su C.X., West B.J.: In vivo antioxidant activity of deacetylasperulosidic acid in noni. J. Anal. Methods Chem. 2013, article ID 804504 (2013)
Kapadia G.J., Sharma S.C., Tokuda H., Nishino H., Ueda S.: Inhibitory effect of iridoids on Epstein–Barr virus activation by a short-term in vitro assay for anti-tumor promoters. Cancer Lett. 102(1–2), 223–226 (1996)
Murata K., Abe Y., Futamura-Masuda M., Uwaya A., Isami F., Deng S., Matsuda H.: Effect of Morinda citrifolia fruit extract and its iridoid glycosides on blood fluidity. J. Nat. Med. 68(3), 498–504 (2014)
Liu W., Li G., Hölscher C., Li L.: Neuroprotective effects of geniposide on Alzheimer's disease pathology. Rev. Neurosci. 26(4), 371–383 (2015)
Zhang W.L., Zhu L., Jiang J.G.: Active ingredients from natural botanicals in the treatment of obesity. Obes. Rev. 15(12), 957–967 (2014)
Yao D.D., Yang L., Wang Y., Liu C., Wei Y.J., Jia X.B., Yin W., Shu L.: Geniposide promotes beta-cell regeneration and survival through regulating β-catenin/TCF7L2 pathway. Cell Death Dis. 6, article ID e1746 (2015)
Hwang H., Kim C., Kim S.M., Kim W.S., Choi S.H., Chang I.M., Ahn K.S.: The hydrolyzed products of iridoid glycoside with β-glucosidase treatment exert anti-proliferative effects through suppression of STAT3 activation and STAT3-regulated gene products in several human cancer cells. Pharm. Biol. 50(1), 8–17 (2012)
Liao P., Liu L., Wang B., Li W., Fang X., Guan S.: Baicalin and geniposide attenuate atherosclerosis involving lipids regulation and immunoregulation in ApoE−/− mice. Eur. J. Pharmacol. 740, 488–495 (2014)
Sun P., Chen J.Y., Li J., Sun M.R., Mo W.C., Liu K.L., Meng Y.Y., Liu Y., Wang F., He R.Q., Hua Q.: The protective effect of geniposide on human neuroblastoma cells in the presence of formaldehyde. BMC Complement. Altern. Med. 13, article ID 152 (2013)
Son M., Lee M., Ryu E., Moon A., Jeong C.S., Jung Y.W., Park G.H., Sung G.H., Cho H., Kang H.: Genipin as a novel chemical activator of EBV lytic cycle. J. Microbiol. 53(2), 155–165 (2015)
Manon L., Béatrice B., Thierry O., Jocelyne P., Fathi M., Evelyne O., Alain B.: Antimutagenic potential of harpagoside and Harpagophytum procumbens against 1-nitropyrene. Pharmacogn. Mag. 11(Suppl 1), S29–S36 (2015)
Sun X., Xiong Z., Zhang Y., Meng Y., Xu G., Xia Z., Li J., Zhang R., Ke Z., Xia Z., Hu Y.: Harpagoside attenuates MPTP/MPP+ induced dopaminergic neurodegeneration and movement disorder via elevating glial cell line-derived neurotrophic factor. J. Neurochem. 120(6), 1072–1083 (2012)
Gagnier J.J., Chrubasik S., Manheimer E.: Harpgophytum procumbens for osteoarthritis and low back pain: a systematic review. BMC Complement. Altern. Med. 4, article ID 13 (2004)
Georgiev M.I., Ivanovska N., Alipieva K., Dimitrova P., Verpoorte R.: Harpagoside: from Kalahari Desert to pharmacy shelf. Phytochemistry. 92, 8–15 (2013)
Ma W., Wang K.J., Cheng C.S., Yan G.Q., Lu W.L., Ge J.F., Cheng Y.X., Li N.: Bioactive compounds from Cornus officinalis fruits and their effects on diabetic nephropathy. J. Ethnopharmacol. 153(3), 840–845 (2014)
Yamabe N., Noh J.S., Park C.H., Kang K.S., Shibahara N., Tanaka T., Yokozawa T.: Evaluation of loganin, iridoid glycoside from Corni Fructus, on hepatic and renal glucolipotoxicity and inflammation in type 2 diabetic db/db mice. Eur. J. Pharmacol. 648(1–3), 179–187 (2010)
Park C.H., Tanaka T., Kim J.H., Cho E.J., Park J.C., Shibahara N., Yokozawa T.: Hepato-protective effects of loganin, iridoid glycoside from Corni Fructus, against hyperglycemia-activated signaling pathway in liver of type 2 diabetic db/db mice. Toxicology. 290(1), 14–21 (2011)
Park C.H., Yamabe N., Noh J.S., Kang K.S., Tanaka T., Yokozawa T.: The beneficial effects of morroniside on the inflammatory response and lipid metabolism in the liver of db/db mice. Biol. Pharm. Bull. 32(10), 1734–1740 (2009)
Wang W., Xu J., Li L., Wang P., Ji X., Ai H., Zhang L., Li L.: Neuroprotective effect of morroniside on focal cerebral ischemia in rats. Brain Res. Bull. 83(5), 196–201 (2010)
Barbaro B., Toietta G., Maggio R., Arciello M., Tarocchi M., Galli A., Balsano C.: Effects of the olive-derived polyphenol oleuropein on human health. Int. J. Mol. Sci. 15(10), 18508–18524 (2014)
Omar S.H.: Oleuropein in olive and its pharmacological effects. Sci. Pharm. 78(2), 133–154 (2010)
Sumiyoshi M., Kimura Y.: Effects of olive leaf extract and its main component oleuroepin on acute ultraviolet B irradiation-induced skin changes in C57BL/6 J mice. Phytother. Res. 24(7), 995–1003 (2010)
Giamarellos-Bourboulis E.J., Geladopoulos T., Chrisofos M., Koutoukas P., Vassiliadis J., Alexandrou I., Tsaganos T., Sabracos L., Karagianni V., Pelekanou E., Tzepi I., Kranidioti H., Koussoulas V., Giamarellou H.: Oleuropein: a novel immunomodulator conferring prolonged survival in experimental sepsis by Pseudomonas aeruginosa. Shock. 26(4), 410–416 (2006)
Zhou J.: Bioactive glycosides from Chinese medicines. Mem. Inst. Oswaldo Cruz. 86(Suppl. 2), 231–234 (1991)
Sun H., Li L., Zhang A., Zhang N., Lv H., Sun W., Wang X.: Protective effects of sweroside on human MG-63 cells and rat osteoblasts. Fitoterapia. 84, 174–179 (2013)
Oztürk N., Korkmaz S., Oztürk Y., Başer K.H.: Effects of gentiopicroside, sweroside and swertiamarine, secoiridoids from gentian (Gentiana lutea ssp. symphyandra), on cultured chicken embryonic fibroblasts. Planta Med. 72(4), 289–294 (2006)
Kumarasamy Y., Nahar L., Cox P.J., Jaspars M., Sarker S.D.: Bioactivity of secoiridoid glycosides from Centaurium erythraea. Phytomedicine. 10(4), 344–347 (2003)
Deng S., West B., Palu A., Jensen J.: Determination and comparative analysis of major iridoids in different parts and cultivation sources of Morinda citrifolia. Phytochem. Anal. 22(1), 26–30 (2011)
Ranalli R., Marchegiani D., Contento S., Girardi F., Nicolosi M.P., Brullo M.D.: Variations of iridoid oleuropein in Italian olive varieties during growth and maturation. Eur. J. Lipid Sci. Tech. 111(7), 678–687 (2009)
Bianchi G.: Lipids and phenols in table olives. Eur. J. Lipid Sci. Tec. 105(5), 229–242 (2003)
Tuck K.L., Hayball P.J.: Major phenolic compounds in olive oil: metabolism and health effects. J. Nutr. Biochem. 13(11), 636–644 (2002)
Savournin C., Baghdikian B., Elias R., Dargouth-Kesraoui F., Boukef K., Balansard G.: Rapid high-performance liquid chromatography analysis for the quantitative determination of oleuropein in Olea europaea leaves. J. Agric. Food Chem. 49(2), 618–621 (2001)
Lockyer S., Corona G., Yaqoob P., Spencer J.P., Rowland I.: Secoiridoids delivered as olive leaf extract induce acute improvements in human vascular function and reduction of an inflammatory cytokine: a randomised, double-blind, placebo-controlled, cross-over trial. Br. J. Nutr. 114(1), 75–83 (2015)
El S.N., Karakaya S.: Olive tree (Olea europaea) leaves: potential beneficial effects on human health. Nutr. Rev. 67(11), 632–638 (2009)
Jensen S.R., Kjaer A., Nielsen B.J.: The genus Comus: non-flavonoid glucosides as taxonomic markers. Biochem. System. Ecol. 3(2), 75–78 (1975)
Du W., Cai H., Wang M., Ding X., Yang H., Cai B.: Simultaneous determination of six active components in crude and processed Fructus Corni by high performance liquid chromatography. J. Pharm. Biomed. Anal. 48(1), 194–197 (2008)
Kucharskaa A.Z., Szumnyb A., Sokół-Łętowskaa A., Pióreckic N., Klymenkoe S.V.: Iridoids and anthocyanins in cornelian cherry (Cornus mas L.) cultivars. J. Food Comp. Anal. 40, 95–102 (2015)
Yamabe N., Kang K.S., Matsuo Y., Tanaka T., Yokozawa T.: Identification of antidiabetic effect of iridoid glycosides and low molecular weight polyphenol fractions of Corni Fructus, a constituent of Hachimi-jio-gan, in streptozotocin-induced diabetic rats. Biol. Pharm. Bull. 30(7), 1289–1296 (2007)
West B.J., Deng S., Jensen C.J., Palu A.K., Berrio L.F.: Antioxidant, toxicity, and iridoid tests of processed Cornelian cherry fruits. Int. J. Food Sc. Tech. 47(7), 1392–1397 (2012)
Jensen, H.D., Krogfelt, K.A., Cornett, C., Hansen, S.H., Christensen, S.B.: Hydrophilic carboxylic acids and iridoid glycosides in the juice of American and European cranberries (Vaccinium macrocarpon and V. oxycoccos), lingonberries (V. vitis-idaea), and blueberries (V. myrtillus). J. Agric. Food Chem. 50(23), 6871–6874 (2002)
Zhang Q., Su Y., Zhang J.: Seasonal difference in antioxidant capacity and active compounds contents of Eucommia ulmoides Oliver leaf. Molecules. 18(2), 1857–1868 (2013)
Li C., Dong J., Tian J., Deng Z., Song X.: LC/MS/MS determination and pharmacokinetic study of iridoid glycosides monotropein and deacetylasperulosidic acid isomers in rat plasma after oral administration of Morinda officinalis extract. Biomed. Chromatogr. 30(2), 163–168 (2016)
Luo, Y.D., Chen, J., Cao, J., Wen, X.D., Li, P.: Determination of sweroside in rat plasma and bile for oral bioavailability and hepatobiliary excretion. Chem. Pharm. Bull. (Tokyo) 57(1), 79–83 (2009)
Suh N.J., Shim C.K., Lee M.H., Kim S.K., Chang I.M.: Pharmacokinetic study of an iridoid glucoside: aucubin. Pharm. Res. 8(8), 1059–1063 (1991)
de Bock M., Thorstensen E.B., Derraik J.G., Henderson H.V., Hofman P.L., Cutfield W.S.: Human absorption and metabolism of oleuropein and hydroxytyrosol ingested as olive (Olea europaea L.) leaf extract. Mol. Nutr. Food Res. 57(11), 2079–2085 (2013)
Jemai H., El Feki A., Sayadi S.: Antidiabetic and antioxidant effects of hydroxytyrosol and oleuropein from olive leaves in alloxan-diabetic rats. J. Agric. Food Chem. 57(19), 8798–8804 (2009)
Carluccio M.A., Siculella L., Ancora M.A., Massaro M., Scoditti E., Storelli C., Visioli F., Distante A., De Caterina R.: Olive oil and red wine antioxidant polyphenols inhibit endothelial activation: antiatherogenic properties of Mediterranean diet phytochemicals. Arterioscler. Thromb. Vasc. Biol. 23(4), 622–629 (2003)
Elamin M.H., Daghestani M.H., Omer S.A., Elobeid M.A., Virk P., Al-Olayan E.M., Hassan Z.K., Mohammed O.B., Aboussekhra A.: Olive oil oleuropein has anti-breast cancer properties with higher efficiency on ER-negative cells. Food Chem. Toxicol. 53, 310–316 (2013)
Scoditti, E., Calabriso, N., Massaro, M., Pellegrino, M., Storelli, C., Martines, G., De Caterina, R., Carluccio, M.A.: Mediterranean diet polyphenols reduce inflammatory angiogenesis through MMP-9 and COX-2 inhibition in human vascular endothelial cells: a potentially protective mechanism in atherosclerotic vascular disease and cancer. Arch. Biochem. Biophys. 527(2), 81–89 (2012a)
Kontogianni V.G., Charisiadis P., Margianni E., Lamari F.N., Gerothanassis I.P., Tzakos A.G.: Olive leaf extracts are a natural source of advanced glycation end product inhibitors. J. Med. Food. 16(9), 817–822 (2013)
Navarro M., Morales F.J.: Mechanism of reactive carbonyl species trapping by hydroxytyrosol under simulated physiological conditions. Food Chem. 175, 92–99 (2015)
Wainstein J., Ganz T., Boaz M., Bar Dayan Y., Dolev E., Kerem Z., Madar Z.: Olive leaf extract as a hypoglycemic agent in both human diabetic subjects and in rats. J. Med. Food. 15(7), 605–610 (2012)
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA): Scientific Opinion on the substantiation of health claims related to polyphenols in olive and protection of LDL particles from oxidative damage (ID 1333, 1638, 1639, 1696, 2865), maintenance of normal blood HDL-cholesterol concentrations (ID 1639), maintenance of normal blood pressure (ID 3781), “anti-inflammatory properties” (ID 1882), “contributes to the upper respiratory tract health” (ID 3468), “can help to maintain a normal function of gastrointestinal tract” (3779), and “contributes to body defences against external agents” (ID 3467) pursuant to Article 13(1) of Regulation (EC) No 1924/2006. EFSA Journal 9(4), article ID 2033 (2011)
Marrugat J., Covas M.I., Fitó M., Schröder H., Miró-Casas E., Gimeno E., López-Sabater M.C., de la Torre R., Farré M.: SOLOS Investigators: Effects of differing phenolic content in dietary olive oils on lipids and LDL oxidation–a randomized controlled trial. Eur. J. Nutr. 43(3), 140–147 (2004)
Covas M.I., de la Torre K., Farré-Albaladejo M., Kaikkonen J., Fitó M., López-Sabater C., Pujadas-Bastardes M.A., Joglar J., Weinbrenner T., Lamuela-Raventós R.M., de la Torre R.: Postprandial LDL phenolic content and LDL oxidation are modulated by olive oil phenolic compounds in humans. Free Radic. Biol. Med. 40(4), 608–616 (2006)
de la Torre-Carbot K., Chávez-Servín J.L., Jaúregui O., Castellote A.I., Lamuela-Raventós R.M., Nurmi T., Poulsen H.E., Gaddi A.V., Kaikkonen J., Zunft H.F., Kiesewetter H., Fitó M., Covas M.I., López-Sabater M.C.: Elevated circulating LDL phenol levels in men who consumed virgin rather than refined olive oil are associated with less oxidation of plasma LDL. J. Nutr. 140(3), 501–508 (2010)
Sajithlal G.B., Chandrakasan G.: Role of lipid peroxidation products in the formation of advanced glycation end products: An in vitro study on collagen. Proc. Indian Acad. Sci. (Chem. Sci.). 111(1), 215–229 (1999)
Navarro M., Morales F.J.: In vitro investigation on the antiglycative and carbonyl trapping activities of hydroxytyrosol. Eur. Food Res, Tech (2016). doi:10.1007/s00217-015-2614-8
Kim H.Y., Moon B.H., Lee H.J., Choi D.H.: Flavonol glycosides from the leaves of Eucommia ulmoides O. with glycation inhibitory activity. J. Ethnopharmacol. 93(2–3), 227–230 (2004)
Jin L., Xue H.Y., Jin L.J., Li S.Y., Xu Y.P.: Antioxidant and pancreas-protective effect of aucubin on rats with streptozotocin-induced diabetes. Eur. J. Pharmacol. 582(1–3), 162–167 (2008)
Park K.S.: Aucubin, a naturally occurring iridoid glycoside inhibits TNF-α-induced inflammatory responses through suppression of NF-κB activation in 3 T3-L1 adipocytes. Cytokine. 62(3), 407–412 (2013)
Shin J.S., Yun K.J., Chung K.S., Seo K.H., Park H.J., Cho Y.W., Baek N.I., Jang D., Lee K.T.: Monotropein isolated from the roots of Morinda officinalis ameliorates proinflammatory mediators in RAW 264.7 macrophages and dextran sulfate sodium (DSS)-induced colitis via NF-κB inactivation. Food Chem. Toxicol. 53, 263–271 (2013)
Hong L., Huiqin X., Yunjie H.: Impact of fructus Corni iridoid glycosides on ACE-P of rat serum in vascular complications of diabetes. World Sci. Tech. – Modern. Trad. Chinese Med. Materia Medica. 5(6), 51–53 (2003)
Shi Y., Xu H.Q.: Protecting effect of total iridoid glycoside in fructus Corni officinalis on experimental diabetes models with heart disease. J. Nanjing Univ. Trad. Chinese Med. 2006(1), 35–37 (2006)
Yamabe N., Kang K.S., Goto E., Tanaka T., Yokozawa T.: Beneficial effect of Corni fructus, a constituent of hachimi-jio-gan, on advanced glycation end-product-mediated renal injury in streptozotocin-treated diabetic rats. Biol. Pharm. Bull. 30(3), 520–526 (2007)
Yamabe N., Kang K.S., Matsuo Y., Tanaka T., Yokozawa T.: Identification of antidiabetic effect of iridoid glycosides and low molecular weight polyphenol fractions of Corni Fructus, a constituent of Hachimi-jio-gan, in streptozotocin-induced diabetic rats. Biol. Pharm. Bull. 30(7), 1289–1296 (2007)
Xu H.Q., Hao H.P.: Effects of iridoid total glycoside from Cornus officinalis on prevention of glomerular overexpression of transforming growth factor beta 1 and matrixes in an experimental diabetes model. Biol. Pharm. Bull. 27(7), 1014–1018 (2004)
Rumble J.R., Cooper M.E., Soulis T., Cox A., Wu L., Youssef S., Jasik M., Jerums G., Gilbert R.E.: Vascular hypertrophy in experimental diabetes. Role of advanced glycation end products. J. Clin. Invest. 99(5), 1016–1027 (1997)
Park C.H., Noh J.S., Kim J.H., Tanaka T., Zhao Q., Matsumoto K., Shibahara N., Yokozawa T.: Evaluation of morroniside, iridoid glycoside from Corni Fructus, on diabetes-induced alterations such as oxidative stress, inflammation, and apoptosis in the liver of type 2 diabetic db/db mice. Biol. Pharm. Bull. 34(10), 1559–1565 (2011)
Liu K., Xu H., Lv G., Liu B., Lee M.K., Lu C., Lv X., Wu Y.: Loganin attenuates diabetic nephropathy in C57BL/6 J mice with diabetes induced by streptozotocin and fed with diets containing high level of advanced glycation end products. Life Sci. 123, 78–85 (2015)
Yokozawa T., Yamabe N., Kim H.Y., Kang K.S., Hur J.M., Park C.H., Tanaka T.: Protective effects of morroniside isolated from Corni Fructus against renal damage in streptozotocin-induced diabetic rats. Biol. Pharm. Bull. 31(7), 1422–1428 (2008)
Xu H., Shen J., Liu H., Shi Y., Li L., Wei M.: Morroniside and loganin extracted from Cornus officinalis have protective effects on rat mesangial cell proliferation exposed to advanced glycation end products by preventing oxidative stress. Can. J. Physiol. Pharmacol. 84(12), 1267–1273 (2006)
Meerwaldt R., Graaff R., Oomen P.H.N., Links T.P., Jager J.J., Alderson N.L., Thorpe S.R., Baynes J.W., Gans R.O.B., Smit A.J.: Simple non-invasive assessment of advanced glycation endproduct accumulation. Diabetologia. 47(7), 1324–1330 (2004)
West B.J., Uwaya A., Isami F., Deng S., Nakajima S., Jensen C.J.: Antiglycation activity of iridoids and their food sources. Int. J. Food Sci. 2014, article ID 276950 (2014)
Cerami C., Founds H., Nicholl I., Mitsuhashi T., Giordano D., Vanpatten S., Lee A., Al-Abed Y., Vlassara H., Bucala R., Cerami A.: Tobacco smoke is a source of toxic reactive glycation products. Proc. Nat. Acad. Sci. U.S.A. 94(25), 13915–13920 (1997)
Ambrose J.A., Barua R.S.: The pathophysiology of cigarette smoking and cardiovascular disease: an update. J. Am. Coll. Cardiol. 43(10), 1731–1737 (2004)
Reynolds P.R., Kasteler S.D., Schmitt R.E., Hoidal J.R.: Receptor for advanced glycation end-products signals through Ras during tobacco smoke-induced pulmonary inflammation. Am. J. Respir. Cell Mol. Biol. 45(2), 411–418 (2011)
Ramasamy R.: Advanced glycation endproducts: from precursors to RAGE: round and round we go. Amino Acids. 42(4), 1151–1161 (2012)
Nicholl I.D., Stitt A.W., Moore J.E., Ritchie A.J., Archer D.B., Bucala R.: Increased levels of advanced glycation endproducts in the lenses and blood vessels of cigarette smokers. Mol. Med. 4(9), 594–601 (1998)
Koetsier M., Lutgers H.L., de Jonge C., Links T.P., Smit A.J., Graaff R.: Reference values of skin autofluorescence. Diabetes Technol. Ther. 12(5), 399–403 (2010)
Yue X., Hu H., Koetsier M., Graaff R., Han C.: Reference values for the Chinese population of skin autofluorescence as a marker of advanced glycation end products accumulated in tissue. Diabet. Med. 28(7), 818–823 (2011)
Monami M., Lamanna C., Gori F., Bartalucci F., Marchionni N., Mannucci E.: Skin autofluorescence in type 2 diabetes: beyond blood glucose. Diabetes Res. Clin. Pract. 79(1), 56–60 (2008)
Sandby-Moller J., Thieden E., Philipsen P.A., Heydenreich J., Wulf H.C.: Skin autofluorescence as a biological UVR dosimeter. Photodermatol. Photoimmunol. Photomed. 20(1), 33–40 (2004)
Nomoto K., Yagi M., Arita S., Ogura M., Yonei Y.: Skin accumulation of advanced glycation end products and lifestyle behaviors in Japanese. Anti-aging Med. 9(6), 165–173 (2012)
Hoonhorst S.J., Lo Tam Loi A.T., Hartman J.E., Telenga E.D., van den Berge M., Koenderman L., Lammers J.W., Marike Boezen H., Postma D.S., Ten Hacken N.H.: Advanced glycation end products in the skin are enhanced in COPD. Metabolism. 63(9), 1149–1156 (2014)
Gopal P., Reynaert N.L., Scheijen J.L., Engelen L., Schalkwijk C.G., Franssen F.M., Wouters E.F., Rutten E.P.: Plasma advanced glycation end-products and skin autofluorescence are increased in COPD. Eur. Respir. J. 43(2), 430–438 (2014)
Wang M.Y., Lutfiyya M.N., Weidenbacher-Hoper V., Anderson G., Su C.X., West B.J.: Antioxidant activity of noni juice in heavy smokers. Chem. Cent. J. 3, article ID 13 (2009)
Wang M.Y., Peng L., Jensen C.J., Deng S., West B.J.: Noni juice reduces lipid peroxidation–derived DNA adducts in heavy smokers. Food Sci. Nutr. 1(2), 141–149 (2013)
Brownlee M.: Biochemistry and molecular cell biology of diabetic complications. Nature. 414(6865), 913–820 (2001)
Miyata T., Wada Y., Cai Z., Iida Y., Horie K., Yasuda Y., Maeda K., Kurokawa K., van Ypersele de Strihou C.: Implication of an increased oxidative stress in the formation of advanced glycation end products in patients with end-stage renal failure. Kidney Int. 51(4), 1170–1181 (1997)
Smith P.R., Thornalley P.J.: Mechanism of the degradation of non-enzymatically glycated proteins under physiological conditions. Studies with the model fructosamine, N epsilon-(1-deoxy-D-fructos-1-yl)hippuryl-lysine. Eur. J. Biochem. 210(3), 729–739 (1992)
Nishikawa T., Edelstein D., Du X.L., Yamagishi S., Matsumura T., Kaneda Y., Yorek M.A., Beebe D., Oates P.J., Hammes H.P., Giardino I., Brownlee M.: Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature. 404(6779), 787–790 (2000)
Araki E., Nishikawa T.: Oxidative stress: A cause and therapeutic target of diabetic complications. J Diabetes Investig. 1(3), 90–96 (2010)
Parzonko A., Czerwińska M.E., Kiss A.K., Naruszewicz M.: Oleuropein and oleacein may restore biological functions of endothelial progenitor cells impaired by angiotensin II via activation of Nrf2/heme oxygenase-1 pathway. Phytomedicine. 20(12), 1088–1094 (2013)
Koriyama Y., Chiba K., Yamazaki M., Suzuki H., Muramoto K., Kato S.: Long-acting genipin derivative protects retinal ganglion cells from oxidative stress models in vitro and in vivo through the Nrf2/antioxidant response element signaling pathway. J. Neurochem. 115(1), 79–91 (2010)
Okada K., Shoda J., Kano M., Suzuki S., Ohtake N., Yamamoto M., Takahashi H., Utsunomiya H., Oda K., Sato K., Watanabe A., Ishii T., Itoh K., Yamamoto M., Yokoi T., Yoshizato K., Sugiyama Y., Suzuki H.: Inchinkoto, a herbal medicine, and its ingredients dually exert Mrp2/MRP2-mediated choleresis and Nrf2-mediated antioxidative action in rat livers. Am. J. Physiol. Gastrointest. Liver Physiol. 292(5), G1450–G1463 (2007)
Gacche R.N., Dhole N.A.: Profile of aldose reductase inhibition, anti-cataract and free radical scavenging activity of selected medicinal plants: an attempt to standardize the botanicals for amelioration of diabetes complications. Food Chem. Toxicol. 49(8), 1806–1813 (2011)
Lee C.M., Jung H.A., Oh S.H., Park C.H., Tanaka T., Yokozawa T., Choi J.S.: Kinetic and molecular docking studies of loganin and 7-O-galloyl-D-sedoheptulose from Corni Fructus as therapeutic agents for diabetic complications through inhibition of aldose reductase. Arch. Pharm. Res. 38(6), 1090–1098 (2015)
Akileshwari C., Muthenna P., Nastasijević B., Joksić G., Petrash J.M., Reddy G.B.: : Inhibition of aldose reductase by Gentiana lutea extracts. Exp. Diabetes Res. 2012, article ID 147965 (2012)
Kohda H., Tanaka S., Yamaoka Y., Yahara S., Nohara T., Tanimoto T., Tanaka A.: Studies on lens-aldose-reductase inhibitor in medicinal plants. II. Active constituents of Monochasma savatierii Franch. et Maxim. Chem. Pharm. Bull (Tokyo). 37(11), 3153–3154 (1989)
Edwards J.L., Vincent A.M., Cheng H.T., Feldman E.L.: Diabetic neuropathy: mechanisms to management. Pharmacol. Ther. 120(1), 1–34 (2008)
Giacco F., Brownlee M.: Oxidative stress and diabetic complications. Circ. Res. 107(9), 1058–1070 (2010)
Levi B., Werman M.J.: Long-term fructose consumption accelerates glycation and several age-related variables in male rats. J. Nutr. 128(9), 1442–1449 (1998)
Hori M., Yagi M., Nomoto K., Ichijo R., Shimode A., Kitano T., Yonei Y.: Experimental models for advanced glycation end product formation using albumin, collagen, elastin, keratin and proteoglycan. Anti-Aging Med. 9(5), 125–134 (2012)
Kawai T., Takei I., Tokui M., Funae O., Miyamoto K., Tabata M., Hirata T., Saruta T., Shimada A., Itoh H.: Effects of epalrestat, an aldose reductase inhibitor, on diabetic peripheral neuropathy in patients with type 2 diabetes, in relation to suppression of N(ɛ)-carboxymethyl lysine. J. Diabetes Complicat. 24(6), 424–432 (2010)
Park C.H., Tanaka T., Kim H.Y., Park J.C., Yokozawa T.: Protective Effects of Corni Fructus against Advanced Glycation Endproducts and Radical Scavenging. Evid. Based Complement. Alternat. Med. 2012, article ID 418953 (2012)
Ghisalberti E.L.: Biological and pharmacological activity of naturally occurring iridoids and secoiridoids. Phytomedicine. 5(2), 147–163 (1998)
West, B.: Bioactivation of deacetylasperulosidic acid: changes in bioactivity. Proceedings of the 2nd Annual International Iridoid Research Symposium, Provo, Utah, 9–10 August (2011)
Ueda S., Iwahashi Y., Tokuda H.: Production of anti-tumor-promoting iridoid glucosides in Genipa americana and its cell cultures. J. Nat. Prod. 54(6), 1677–1680 (1991)
Huh S.O., Kim J.H., Chang I.M.: Effects of iridoid compounds on RNA and protein biosynthesis in Sarcoma 180 cells. Saengyak Hakhoe Chi. 16(99), 99–104 (1985)
Chang I.M.: Antiviral activity of aucubin against hepatitis B virus replication. Phytother. Res. 11(3), 189–195 (1997)
Yamazaki M., Chiba K., Mohri T.: Neuritogenic effect of natural iridoid compounds on PC12h cells and its possible relation to signaling protein kinases. Biol. Pharm. Bull. 19(6), 791–795 (1996)
Isiguro K., Yamaki M., Takagi S., Ikeda Y., Kawakami K., Ito K., Nose T.: Studies on iridoid-related compounds. IV. Antitumor activity of iridoid aglycones. Chem. Pharm. Bull. (Tokyo). 34(6), 2375–2379 (1986)
Takino J., Nagamine K., Hori T., Sakasai-Sakai A., Takeuchi M.: Contribution of the toxic advanced glycation end-products-receptor axis in nonalcoholic steatohepatitis-related hepatocellular carcinoma. World J. Hepatol. 7(23), 2459–2469 (2015)
Pertynska-Marczewska M., Diamanti-Kandarakis E., Zhang J., Merhi Z.: Advanced glycation end products: A link between metabolic and endothelial dysfunction in polycystic ovary syndrome? Metabolism. 64(11), 1564–1573 (2015)
Malik P., Chaudhry N., Mittal R., Mukherjee T.K.: Role of receptor for advanced glycation end products in the complication and progression of various types of cancers. Biochim. Biophys. Acta. 1850(9), 1898–1904 (2015)
Kouidrat Y., Amad A., Arai M., Miyashita M., Lalau J.D., Loas G., Itokawa M.: Advanced glycation end products and schizophrenia: A systematic review. J. Psychiatr. Res. 66-67, 112–117 (2015)
Angeloni C., Zambonin L., Hrelia S.: Role of methylglyoxal in Alzheimer's disease. Biomed. Res. Int. 2014, article ID 238485 (2014)
Prasad C., Imrhan V., Marotta F., Juma S., Vijayagopal P.: Lifestyle and Advanced Glycation End Products (AGEs) Burden: Its Relevance to Healthy Aging. Aging. Dis. 5(3), 212–217 (2014)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors, with the exception of Sho-ichi Yamagishi, have been employed by Morinda, Inc., a manufacturer of food products containing iridoids. Sho-ichi Yamagishi has participated as a guest lecturer at educational conferences organized by Morinda, Inc.
Rights and permissions
About this article
Cite this article
West, B.J., Deng, S., Uwaya, A. et al. Iridoids are natural glycation inhibitors. Glycoconj J 33, 671–681 (2016). https://doi.org/10.1007/s10719-016-9695-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10719-016-9695-x