Abstract
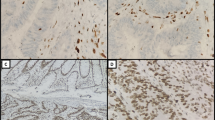
To determine the diagnostic test characteristics and inter-observer variation of pathology features for identifying high microsatellite instability (MSI-H) colorectal cancer (CRC). Six pathologists blindly evaluated 177 CRC for the presence of MSI-H associated pathology features. Inter-observer agreement was determined by using Kappa-statistics. In the first random 88/177 cases, mucinous carcinoma, tumor-infiltrating lymphocytes (TIL) and Crohns-like infiltrate (CLI) were the best discriminators between MSI-H and microsatellite stable CRC [OR 5.6 (95 % CI 1.7–19), 5.4 (1.8–17) and 3.5 (1.1–11), respectively], with high specificity (89–91 %). The sensitivities for MSI-H, however, were low (31–41 %). In addition, inter-observer agreement was moderate for TIL and CLI (κ 0.38 and 0.48, respectively), but very good for mucinous carcinoma (κ 0.86). Interpretation of overall histopathology as suggestive for MSI-H performed better than any individual feature; OR 15 (5.2–44), and area under the curve 0.79. However, inter-observer agreement was moderate (κ 0.53). In the second set, TIL and CLI were scored according to updated scoring systems. Although both remained the best individual discriminators, test characteristics and inter-observer agreement did not improve. MSI-H pathology features have moderate accuracy for identifying MSI-H CRC, and are identified with moderate inter-observer agreement. These findings highlight the limitations of clinical strategies, such as the revised Bethesda guidelines, which incorporate the MSI-H associated pathology features in their strategy to identify persons with lynch syndrome.

Similar content being viewed by others
References
Aaltonen LA, Salovaara R, Kristo P et al (1998) Incidence of hereditary nonpolyposis colorectal cancer and the feasibility of molecular screening for the disease. N Engl J Med 338:1481–1487
Moreira L, Balaguer F, Lindor N et al (2012) Identification of Lynch syndrome among patients with colorectal cancer. JAMA 308:1555–1565
Watson P, Lynch HT (1993) Extracolonic cancer in hereditary nonpolyposis colorectal cancer. Cancer 71:677–685
Jarvinen HJ, Aarnio M, Mustonen H et al (2000) Controlled 15-year trial on screening for colorectal cancer in families with hereditary nonpolyposis colorectal cancer. Gastroenterology 118:829–834
Umar A, Boland CR, Terdiman JP et al (2004) Revised Bethesda guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst 96:261–268
Boland CR, Shike M (2010) Report from the Jerusalem workshop on Lynch syndrome-hereditary nonpolyposis colorectal cancer. Gastroenterology 138(2197):e2191–e2197
Perez-Carbonell L, Ruiz-Ponte C, Guarinos C et al (2012) Comparison between universal molecular screening for Lynch syndrome and revised Bethesda guidelines in a large population-based cohort of patients with colorectal cancer. Gut 61:865–872
Jenkins MA, Hayashi S, O’Shea AM et al (2007) Pathology features in Bethesda guidelines predict colorectal cancer microsatellite instability: a population-based study. Gastroenterology 133:48–56
Kievit W, de Bruin JH, Adang EM et al (2005) Cost effectiveness of a new strategy to identify HNPCC patients. Gut 54:97–102
van Lier MG, Leenen CH, Wagner A et al (2012) Yield of routine molecular analyses in colorectal cancer patients ≤70 years to detect underlying Lynch syndrome. J Pathol 226:764–774
Kastrinos F, Steyerberg EW, Mercado R et al (2012) The PREMM(1,2,6) model predicts risk of MLH1, MSH2, and MSH6 germline mutations based on cancer history. Gastroenterology 140:73–81
Jass JR, Sobin LH (1989) Histological typing of intestinal tumours. WHO international histological classification of tumours, 2nd edn. Springer, Heidelberg, pp 29–40
van Lier MG, Wagner A, van Leerdam ME et al (2010) A review on the molecular diagnostics of Lynch syndrome: a central role for the pathology laboratory. J Cell Mol Med 14:181–197
Sim J, Wright CC (2005) The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther 85:257–268
Alexander J, Watanabe T, Wu TT et al (2001) Histopathological identification of colon cancer with microsatellite instability. Am J Pathol 158:527–535
Shia J, Ellis NA, Paty PB et al (2003) Value of histopathology in predicting microsatellite instability in hereditary nonpolyposis colorectal cancer and sporadic colorectal cancer. Am J Surg Pathol 27:1407–1417
Smyrk TC, Watson P, Kaul K, Lynch HT (2001) Tumor-infiltrating lymphocytes are a marker for microsatellite instability in colorectal carcinoma. Cancer 91:2417–2422
Overbeek LI, Hoogerbrugge N, van Krieken JH et al (2008) Most patients with colorectal tumors at young age do not visit a cancer genetics clinic. Dis Colon Rectum 51:1249–1254
Van Lier MG, De Wilt JH, Wagemakers JJ et al (2009) Underutilization of microsatellite instability analysis in colorectal cancer patients at high risk for Lynch syndrome. Scand J Gastroenterol 44:600–604
Koch LH, Lampros JN, Delong LK et al (2009) Randomized comparison of virtual microscopy and traditional glass microscopy in diagnostic accuracy among dermatology and pathology residents. Hum Pathol 40:662–667
Sanders DS, Grabsch H, Harrison R et al (2012) Comparing virtual with conventional microscopy for the consensus diagnosis of Barrett’s neoplasia in the AspECT Barrett’s chemoprevention trial pathology audit. Histopathology 61:795–800
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Putten, P.G., van Lier, M.G.F., Hage, M. et al. Limited diagnostic value of microsatellite instability associated pathology features in colorectal cancer. Familial Cancer 13, 351–359 (2014). https://doi.org/10.1007/s10689-014-9705-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-014-9705-8