Abstract
Objectives
As the largest organ of the human body, the skin is the major exposure route of NO2. However, the evidence for a relationship between NO2 exposure and dermatologic diseases (DMs) is limited. This time-series study was conducted to assess the short-term effect of nitrogen dioxide (NO2) exposure on DMs outpatient visits in Xinxiang, China.
Methods
Daily recordings of NO2 concentrations, meteorological data, and the outpatient visits data for DMs were collected in Xinxiang from January 1st, 2015, to December 31st, 2018. The analysis method used was based on the generalized additive model (GAM) with quasi-Poisson regression to investigate the relationship between NO2 exposure and DMs outpatient visits. Several covariates, such as long-term trends, seasonality, and weather conditions were controlled.
Results
A total of 164,270 DMs outpatients were recorded. A 10 μg/m3 increase in NO2 concentrations during the period was associated with a 1.86% increase in DMs outpatient visits (95% confidence intervals [Cl]: 1.06–2.66%). The effect was stronger (around 6 times) in the cool seasons than in warmer seasons and younger patients (< 15 years of age) appeared to be more vulnerable.
Conclusions
The findings of this study indicate that short-term exposure to NO2 increases the risk of DMs in Xinxiang, China, especially in the cool seasons. Policymakers should implement more stringent air quality standards to improve air quality.
Similar content being viewed by others
Introduction
Epidemiological and animal studies have demonstrated that nitrogen dioxide (NO2) exposure could induce a wide range of adverse health effects, such as respiratory defects, cardiovascular system diseases, neurodevelopmental disorder, preterm birth, depressed lung function, cancers incidence (Luo et al. 2016; Bowatte et al. 2018; Ritz et al. 2019; Lu et al. 2019; Permaul et al. 2020; Yan et al. 2020; Al-Ahmadi and Al-Zahrani 2013), even associated with coronavirus fatality (Ogen 2020). One recently published research analyzed 272 cities found that NO2 exposure (lag01, the moving averages for the current day and the previous day) would increase the risk of death from total natural causes such as cardiovascular disease and respiratory system (Chen et al. 2018). Study conducted in the Middle East evaluated short-term air pollution exposure before death and revealed that the association between NO2 exposure and mortality was slightly larger than PM2.5, and the effect was independent of PM2.5 (Amini et al. 2019). Our previous study found NO2 exposure was significantly associated with increased hospital outpatients due to eye diseases (Song et al. 2019).
Skin, the largest and outermost organ, is susceptible to air pollution (especially those gaseous air pollutants). NO2, as a toxic component, can undergo photolysis and potentially affect the skin (Fussell and Kelly 2019). The Short-term effect refers to the pollution effect that immediately shows biological effects or harmful symptoms due to environmental pollution. Several experimental studies have shown that the skin is the major exposure route of NO2, and short-term exposure to NO2 produced a carcinogen in vivo, like nitrosation agent (NSA) (Mirvish et al. 1983; Mirvish et al. 1988). A single-blind epidemiology study has demonstrated that human epidermal barrier function was disrupted when short-term exposed to low concentrations of NO2 (Eberlein-Konig et al. 1998). More and more epidemiological evidence showed that NO2 exposure has adverse effects on various skin diseases, such as allergic and immunologic skin diseases (e.g., atopic dermatitis, chronic eczema) (Kathuria and Silverberg 2016; Schnass et al. 2018; Kim et al. 2017); chronic skin inflammatory disease such as acne vulgaris (Liu et al. 2018b); and other skin conditions (Huls et al. 2016). However, evidence of short-term NO2 exposure on DMs diseases was still lacking.
NO2 exposure might affect the skin either by direct impairment to the skin barrier or by indirect inflammation or oxidative stress injury (Ryu et al. 2019; Araviiskaia et al. 2019; Schnass et al. 2018; Furue et al. 2019; Hidaka et al. 2017). In another way, NO2 dissolved in water may irritate the cutaneous microflora (Li et al. 2018; Dell et al. 2014), and then break the balance of the skin flora’s immune function between effective protection and damaging inflammation (Kim and Kim 2019).
The activation of AhR (aryl hydrocarbon receptor) was considered a mechanism of air-pollution-induced AD (atopic dermatitis) (Hidaka et al. 2017). A cohort study highlighted that the mechanism of TRAP (traffic-related air pollutant) induced atopic eczema might be mediated by AhR (Schnass et al. 2018).
With the rapid development of urbanization, industrialization, and motorization, Chinese cities have been heavily polluted (Feng et al. 2018; Wang et al. 2018; Liu et al. 2018a). According to the report on the State of the Ecology and Environment in China (http://english.mee.gov.cn/Resources/Reports/soe/), in 2015–2018, the average concentrations of PM2.5, PM10, O3, SO2, NO2 and CO were 47 μg/m3, 81 μg/m3, 151 μg/m3, 20 μg/m3, 35 μg/m3, and 1.8 mg/m3, respectively. Since the APPCAP (Air Pollution Prevention and Control Action Plan) issued in 2013, the air quality was substantially enhanced in China, however, the concentrations of NO2 have not been significantly changed (Huang et al. 2018). Cui et al. (2019) found that high NO2 concentrations mainly occurred in North China Plain (Cui et al. 2019). Xinxiang, which lies in the south-west of the North China Plain, experiences the most serious environmental pollution (Song et al. 2019), the average annual concentrations of NO2 were 48.4 μg/m3 in 2015–2018. While the daily and annual limit of NO2 concentrations in the National Ambient Air Quality of China were 80 µg/m3 and 40 μg/m3, respectively. Thus, we conducted this epidemiology study to investigate the effect of short-term NO2 exposure on DMs outpatient visits in Xinxiang, China.
Materials and methods
Xinxiang (113°54′E 35°18′N), an important industrial area in the Central Plains region of China (Fig. 1), is a medium-sized city with a history of around 2,400 years. Briefly, Xinxiang covers a 140 km2 area. In 2015, it housed approximately 6.67 million individuals. Xinxiang, a prefecture-level city in Henan province, compared to metropolis (such as Beijing, Shanghai, even Zhengzhou), its population migration rate is lower and most of the patients come from local region.
Health data
Records of DMs outpatients from January 1st, 2015, to December 31st, 2018, were obtained from the First Affiliated Hospital of Xinxiang Medical University. This is the largest hospital located in Xinxiang, which covers all citizens of Xinxiang and has more than 850,000 outpatients and 100,000 inpatients per year (Song et al. 2019). Moreover, unlike lots of metropolis’ hospitals which have over-saturation patients, the First Affiliated Hospital of Xinxiang Medical University showing better outpatient volatility. The primary health outcome investigated in this study was hospital outpatient visits in the Dermatology department with a main diagnosis of skin and subcutaneous tissue diseases according to the international classification of diseases 10th revision (ICD10 code L00-L99). Several representative diseases such as dermatitis (L30.900), eczema (L30.902), psoriasis (L40.900), urticaria (L50.900), acne (L70.900), and vitiligo (L80.X00) were also calculated. The data cleaning procedures were carried out by MySQL server (version 5.6.26). Briefly, duplicate records and those patients who live outside the urban areas of Xinxiang were deleted, and all records were recorded with ICD-10 code (Song et al. 2018).
Meteorological and air pollution data
Hourly air pollution levels of NO2 were obtained from China’s National Urban Air Quality Real Time Publishing Platform (http://106.37.208.233:20035/). Daily average concentrations of NO2 were calculated from four fixed-site air quality-monitoring stations, which were distributed in the urban districts of Xinxiang. These stations were located away from major roads, industrial sources, or residential sources of emission from the burning of coal, or waste; thus, the monitoring results reflect the general urban background level.
Meteorological data, including average temperatures and relative humidity, were obtained from the China Meteorological data sharing service for the same period. Those meteorological data were incorporated into GAM model to adjust for their confounding.
Statistical analysis
The method in the time-series study was based on the generalized additive model (GAM) with quasi-Poisson regression. In the core model, we introduced nonparametric smoothing functions to control for several confounding factors, such as long-term time trends, seasonality, meteorology, public holidays, and day of the week (DOW). A natural cubic regression smooth function of calendar time with 8 degrees of freedom (df) per year was used to control for seasons and long-term trends, 6 (df) were used for temperature, and 3 (df) for relative humidity (Song et al. 2019). The main model is described as follow:
where Yt is the expected number of DMs outpatients at day t; β represents the log-related rate of DMs outpatients associated with a unit increase in NO2; Zt represents the NO2 concentration at day t; ns is the natural cubic spline; and DOW is the day of the week of day t.
The potentially delayed effects were examined using various lag structures. These lag structures were classified into two categories: single lag exposure (lag0–lag7) and cumulative lag exposure (moving averages for the current day and the previous one to seven days: lag01–lag07). The Akaike information criterion and generalized cross-validation (GCV) value were calculated to determine the best lag structure.
We performed five sensitivity analyses to examine the stability of our models. Firstly, the df for long-term and season trends were changed from 5 to 10 df/year to test the robustness of the model. Secondly, two-pollutant models were fitted to assess stability. Thirdly, we analyzed the relationship between daily NO2 concentrations and outpatient amount of virus warts (B07), which were caused by human papillomavirus.
The fourth, the temperature and relative humidity were stratified as >17 °C vs. ≤ 17 °C and > 6% vs. ≤ 61%. And finally, we controlled longer lag day's temperature and relative humidity (up to 21 days), as previous studies have found that those meteorological conditions may have prolonged health effect (Ma et al. 2015; Wang et al. 2018).
Statistical analyses were two-sided, with a significance level of 5%. All statistical analyses were performed using the ‘mgcv’ package of the R software (version 3.3.3).
Results
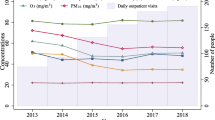
Table 1 shows the descriptive statistics of annual NO2 concentrations, meteorological data, and DMs outpatient data. From January 1st, 2015, to December 31st, 2018, a total of 164,270 outpatient records due to DMs were selected from the electronic information system. On average, there were 113 visits for DMs per day, including 56 male and 57 female patients. For specific diseases, outpatients for dermatitis (L30.900) accounted for the highest number of patients (11.5%), about 13 cases a day. The hospital visits data were slightly lower in the cold seasons than in the warm seasons (103 /day vs. 122 /day, respectively). In the 4-year period, the average annual mean concentrations of NO2 were 48.4 μg/m3 and ranged from 10.0 to 165.0 μg/m3. The Spearman correlation coefficients of NO2 concentrations with PM2.5, PM10, CO and SO2 were 0.67, 0.69, 0.63 and 0.55 (p < 0.01), respectively; but negatively related with O3 and temperature (r = −.57 and −0.53, p < 0.01). The average daily mean temperature of Xinxiang during our study period was 16.0 °C, with a mean relative humidity of 60.0%.
Figure 2 shows the effect estimates on DMs outpatient visits in the single pollutant model. The association between NO2 concentrations and DMs outpatients was statistically significant on lag0, lag01, and lag02 structure. A 10 μg/m3 increase in NO2 concentrations was associated with a 1.86% (95% CI: 1.06%-2.66%) increment in DMs outpatient visits on lag0. For specific dermatology diseases, significant excess risks exhibit between NO2 concentrations and psoriasis, vitiligo, eczema, dermatitis, and acne, with estimate of 3.09% (95% CI: 1.26–4.92%), 3.49% (1.14–5.83%), 2.44% (95% CI: 0.08–4.80%), 1.98% (95% CI: 0.03–3.92%), and 1.98% (95% CI: 0.03–3.92%), respectively (Table 2).
Figure 3 shows the exposure–response relationship curves between NO2 concentrations and DMs outpatient visits. We found a strong linear relationship when the NO2 concentrations ≥60 μg/m3.
We present the estimates and 95% CIs for the associations between NO2 concentrations and DMs outpatient visits stratified by gender, season and age in Table 3. The effect was stronger (around 6 times) in the cool seasons than in warm seasons. Increases in NO2 concentrations were significantly associated with increment risk of DMs outpatient visits in the cool seasons with an estimate of 2.27% (95% CI: 1.17–3.37%). The younger group (under 15 years old) and males appeared to be more sensitive, although these results were non-significant.
The five sensitivity tests show that the effects were not materially influenced. First, when we adjusted the smoothness of time using alternative df, from 5 to 10 per year, the results remained robust (Fig. 4). Second, in the two-pollutant models, we adjusted the annual mean concentrations of other pollutions, such as SO2, O3, CO, PM2.5 and PM10, separately; the estimated effects remained statistically significant (Table 4). In another sensitivity analysis, we analyzed the association between NO2 concentrations and outpatient visits due to viral warts (B07), noncancerous skin growths caused due to viral infection; however, no associations were found (0.35%, 95% CI: -1.98–2.68%), proposing that our results were not attributable to stochastic errors. In addition, two more stratified analyses were carried out for Temperature and relative humidity, while there were no significant differences between > 17 °C and ≤ 17 °C temperature or between > 61% and ≤ 61% relative humidity. Lastly, when we further adjusted for temperature or relative humidity of longer lag days (up to 21 days), results proved that the estimated effect remained consistent (Figure S1).
Discussion
This time series analysis study investigated the relationship between daily DMs outpatient visits and annual outdoor NO2 concentrations levels in Xinxiang from 2015 to 2018. The results showed that NO2 concentrations were significantly associated with DMs outpatient visits on the current day, the association was stronger in the cool seasons than in the warm seasons. This study provides updated evidence to establish the associations between air pollution and adverse health effects.
To the best of our knowledge, this is the first study to suggest that NO2 has a short-term effect on total skin diseases. There was a statistically significant relation between NO2 concentrations and outpatients of DMs diseases in our study. Previous studies just focused on only one or two specific skin diseases. One study conducted in the United States found that higher annual NO2 concentrations were associated with a higher prevalence of eczema (Kathuria and Silverberg 2016). Another study involving 510,158 eczema visits reported that a 10 µg/m3 increase in NO2 (lag06) concentrations was associated with a 2.31% (95% CI: 1.17–3.45%) increase of outpatient visits (Li et al. 2016). Liu et al. (2016, 2018a, b) also observed that NO2 concentrations were significantly associated with childhood atopic eczema and acne vulgaris in outpatients (Liu et al. 2018b, 2016). A cross-sectional study conducted in France found that long-term exposure of NO2 in children was significantly associated with lifetime eczema (Penard-Morand et al. 2010). Schnass et al. (2018) also found that long-term TRAP exposure was associated with a high incidence of eczema in elderly women (Schnass et al. 2018). Using the SALIA cohort data, Huls et al. (2019) found that baseline NO2 concentrations were associated with increased odds of eczema incident (Huls et al. 2019). A panel study in Korea found that a 10 ppb increase in NO2 concentrations could increase the risk of atopic dermatitis by 5.0% (95% CI: 1.4–8.8%) on that day (Kim et al. 2017). A recently published review observed that NO2 exposure could play a role in the development of childhood atopic dermatitis (Hendricks et al. 2019). A panel study conducted in Seoul found that children with atopic dermatitis (33.7%) were sensitive to NO2 concentrations (Noh et al. 2019). To a larger extent, our result was consistent with those studies. Additionally, we analyzed the relationship between NO2 concentrations and several specific skin diseases including urticaria, psoriasis, and vitiligo, results showed statistically significant associations between NO2 concentrations and psoriasis and vitiligo; a positive but non-significant association between NO2 concentrations and urticaria; Psoriasis and vitiligo may be the most sensitive indicators, and therefore may be early signs of NO2 concentrations exposure. Overall, the symptoms of DMs seem exacerbated when people are exposed to high concentrations of NO2.
The mechanisms for the effects of NO2 on the skin are mainly unclear; however, some hypotheses may explain these effects. First, exposure to NO2 has been proved to damage the skin barrier function and thus increase trans-epidermal water loss; then impact the immunological function of the skin, facilitating the development and the relapse of diseases (Pesce et al. 2015; Eberlein-Konig et al. 1998). Besides, NO2 may potentially worsen skin disease via irritant or oxidative stress effects through AhR (Hidaka et al. 2017; Furue et al. 2019; Schnass et al. 2018). The third hypothesis is exposure to NO2 may affect the healthy balance and constituents of the skin microbiome (Prescott et al. 2017). Dysbiosis of the skin microbial community (microbiome) may promote disease progression (Araviiskaia et al. 2019; Sun et al. 2019).
To minimize the effects of meteorological and biological confounding factors on allergic and immunologic skin diseases (e.g., eczema, dermatitis, urticaria, etc.), we conducted a stratified analysis by season. The winter in Xinxiang lasts four months, from Nov 15th to March 15th, and central heating is provided during this period. Coal consumption during this time directly increases the concentration of NO2 (Luo et al. 2016; Liu et al. 2019). Our study detected that the relations were stronger in the cool season. In contrast, Li et al. (2016) found that estimates of NO2 associated with outpatient visits of eczema were much higher in the warm season (Li et al. 2016). Guo et al. (2019) observed that when the temperature was high, NO2 showed a strong positive association with outpatient visits for atopic dermatitis (Guo et al. 2019). For different specific skin diseases, exposure levels and time, along with individual confounders (such as age, gender, smoking, socioeconomic status, and habits), may partially explain the inconsistency.
Our study also found a higher risk in males, though the difference was insignificant. This may be due to females tending to use more skincare, which could improve the skins barrier function to reduce cutaneous pollutant penetration, while males are more likely to go outdoors. A nationwide cross-sectional study conducted in Taiwan demonstrated a significantly positive association between NOx and eczema which was only present among females (Lee et al. 2008), while a panel study in Korea found that males exhibited significant association between atopic dermatitis and NO2, however, this was insignificant in females (Kim et al. 2017). There is no evidence to explain the sex-specific response to NO2; the exact reason requires investigation. The inconsistency of the present results might be due to the difference in study designs, specific diseases, exposure levels, and individual variability of skin penetrability, effects of skincare and makeup, or socioeconomic factors.
A non-significant correlation was observed in our study among age groups, where younger people (< 15 years) appeared to be more sensitive to NO2. Atopic dermatitis is one of the most prevalent skin conditions seen in infants and children (Kathuria and Silverberg 2016). Liu et al. (2016) concluded that exposure to NO2 is a risk factor for childhood eczema, and suggests that this risk has a concentration threshold (Liu et al. 2016). We speculate that for teenagers, the skin barrier development is not complete yet; so, it is vulnerable to the stimulation from the external environment. During puberty, skin oil secretion is more than in younger years; incorrect care practices may increase skin sensitivity and make individuals more susceptible to external stimuli. Moreover, children have inadequate detoxification systems and exposure to environmental toxic substances may have serious health effects.
In this study, we investigate the acute effect of NO2 on DMs outpatient visits based on a large database in Xinxiang, China. Nevertheless, limitations should be noted in interpreting the results of our study. Firstly, we use the average concentrations of local measuring stations rather than personal measures for NO2 exposures. However, this measurement error may bias our results toward the null hypothesis, underestimating the risks (Kim et al. 2018). Secondly, this time-series study is essentially an ecologic analysis; the results cannot be directly inferred to the individual levels. We also cannot control for potential individual confounding factors (such as genetic predisposition and lifestyles) (Li et al. 2016), further toxicological or epidemiological studies are needed to address causality (Bind 2019). Other limitations related to the data source involved in this study include skin diseases that may be affected by genetics and the relevant information such as family aggregation having not been collected. Lastly, even though we used DMs outpatient visits from the largest hospital in the city, the selection bias might still exist.
Summary
Our results demonstrate that short-term exposure to NO2 is allied with a higher risk of dermatologic diseases, especially in the cool seasons. NO2 may promote or exacerbate symptoms of various skin diseases, in particular psoriasis and vitiligo. The results contribute to the inadequate epidemiologic evidence that NO2 possibly impact the skin health. Currently, our understanding of the effects of NO2 on DMs is limited. Future studies could focus on the effects of long-term and short- term exposure to air pollutants on the skin.
Data availability
Data were available after application.
References
Al-Ahmadi, K., & Al-Zahrani, A. (2013). NO(2) and cancer incidence in Saudi Arabia. International Journal of Environmental Research and Public Health, 10(11), 5844–5862. https://doi.org/10.3390/ijerph10115844.
Amini, H., Trang Nhung, N. T., Schindler, C., Yunesian, M., Hosseini, V., Shamsipour, M., et al. (2019). Short-term associations between daily mortality and ambient particulate matter, nitrogen dioxide, and the air quality index in a Middle Eastern megacity. Environmental Pollution, 254(Pt B), 113121. https://doi.org/10.1016/j.envpol.2019.113121.
Bind, M. A. (2019). Causal modeling in environmental health. Annual Review of Public Health,40, 23–43. https://doi.org/10.1146/annurev-publhealth-040218-044048.
Bowatte, G., Lodge, C. J., Knibbs, L. D., Erbas, B., Perret, J. L., Jalaludin, B., et al. (2018). Traffic related air pollution and development and persistence of asthma and low lung function. Environment International, 113, 170–176. https://doi.org/10.1016/j.envint.2018.01.028.
Chen, R., Yin, P., Meng, X., Wang, L., Liu, C., Niu, Y., et al. (2018). Associations between ambient nitrogen dioxide and daily cause-specific mortality: Evidence from 272 Chinese cities. Epidemiology, 29(4), 482–489. https://doi.org/10.1097/EDE.0000000000000829.
Cui, Y., Jiang, L., Zhang, W., Bao, H., Geng, B., He, Q., et al. (2019). Evaluation of China’s Environmental Pressures Based on Satellite NO2 Observation and the Extended STIRPAT Model. International Journal of Environmental Research and Public Health, 16(9), 1487. https://doi.org/10.3390/ijerph16091487.
Dell, S. D., Jerrett, M., Beckerman, B., Brook, J. R., Foty, R. G., Gilbert, N. L., et al. (2014). Presence of other allergic disease modifies the effect of early childhood traffic-related air pollution exposure on asthma prevalence. Environment International,65, 83–92. https://doi.org/10.1016/j.envint.2014.01.002.
Araviiskaia, E., Berardesca, E., Bieber, T., Gontijo, G., Sanchez Viera, M., Marrot, L., et al. (2019). The impact of airborne pollution on skin. JEADV, 33, 1496–1505.
Eberlein-Konig, B., Przybilla, B., Kuhnl, P., Pechak, J., Gebefugi, I., Kleinschmidt, J., et al. (1998). Influence of airborne nitrogen dioxide or formaldehyde on parameters of skin function and cellular activation in patients with atopic eczema and control subjects. The Journal of Allergy and Clinical Immunology, 101(1 Pt 1), 141–143. https://doi.org/10.1016/S0091-6749(98)70212-X.
Feng, Y., Wang, X., Du, W., & Liu, J. (2018). Effects of Air pollution control on urban development quality in chinese cities based on spatial durbin model. International Journal of Environmental Research and Public Health, 15(12), 2822. https://doi.org/10.3390/ijerph15122822.
Furue, M., Hashimoto-Hachiya, A., & Tsuji, G. (2019). Aryl Hydrocarbon Receptor in Atopic Dermatitis and Psoriasis. International Journal of Molecular Science, 20(21), doi:https://doi.org/10.3390/ijms20215424.
Fussell, J. C., & Kelly, F. J. (2019). Oxidative contribution of air pollution to extrinsic skin ageing. Free Radical Biology & Medicine. https://doi.org/10.1016/j.freeradbiomed.2019.11.038.
Guo, Q., Xiong, X., Liang, F., Tian, L., Liu, W., Wang, Z., et al. (2019). The interactive effects between air pollution and meteorological factors on the hospital outpatient visits for atopic dermatitis in Beijing, China: a time-series analysis. Journal of the European Academy of Dermatology and Venereology, 33(12), 2362–2370. https://doi.org/10.1111/jdv.15820.
Hendricks, A. J., Eichenfield, L. F., & Shi, V. Y. (2019). The impact of airborne pollution on atopic dermatitis-a literature review. British Journal of Dermatology. https://doi.org/10.1111/bjd.18781.
Hidaka, T., Ogawa, E., Kobayashi, E. H., Suzuki, T., Funayama, R., Nagashima, T., et al. (2017). The aryl hydrocarbon receptor AhR links atopic dermatitis and air pollution via induction of the neurotrophic factor artemin. Nature Immunology,18(1), 64–73. https://doi.org/10.1038/ni.3614.
Huang, J., Pan, X., Guo, X., & Li, G. (2018). Health impact of China’s air pollution prevention and control action plan: An analysis of national air quality monitoring and mortality data. The Lancet Planetary Health, 2(7), e313–e323. https://doi.org/10.1016/s2542-5196(18)30141-4.
Huls, A., Abramson, M. J., Sugiri, D., Fuks, K., Kramer, U., Krutmann, J., et al. (2019). Nonatopic eczema in elderly women: Effect of air pollution and genes. Journal of Allergy and Clinical Immunology, 143(1), 378–385. https://doi.org/10.1016/j.jaci.2018.09.031.
Huls, A., Vierkotter, A., Gao, W., Kramer, U., Yang, Y., Ding, A., et al. (2016). Traffic-related air pollution contributes to development of facial lentigines: Further epidemiological evidence from caucasians and Asians. The Journal of Investigative Dermatology,136(5), 1053–1056. https://doi.org/10.1016/j.jid.2015.12.045.
Kathuria, P., & Silverberg, J. I. (2016). Association of pollution and climate with atopic eczema in US children. Pediatric Allergy and Immunology, 27(5), 478–485. https://doi.org/10.1111/pai.12543.
Kim, H., Kim, W., Choi, J. E., Kim, C., & Sohn, J. (2018). Short-term effect of ambient air pollution on emergency department visits for diabetic coma in Seoul Korea. Journal of Preventive Medicine and Public Health, 51(6), 265–274. https://doi.org/10.3961/jpmph.18.153.
Kim, J. E., & Kim, H. S. (2019). Microbiome of the Skin And Gut In Atopic Dermatitis (AD): Understanding the pathophysiology and finding novel management strategies. Journal of Clinical Medicine, 8(4), doi:https://doi.org/10.3390/jcm8040444.
Kim, Y. M., Kim, J., Han, Y., Jeon, B. H., Cheong, H. K., & Ahn, K. (2017). Short-term effects of weather and air pollution on atopic dermatitis symptoms in children: A panel study in Korea. PLoS ONE, 12(4), e0175229. https://doi.org/10.1371/journal.pone.0175229.
Lee, Y. L., Su, H. J., Sheu, H. M., Yu, H. S., & Guo, Y. L. (2008). Traffic-related air pollution, climate, and prevalence of eczema in Taiwanese school children. The Journal of Investigative Dermatology, 128(10), 2412–2420. https://doi.org/10.1038/jid.2008.110.
Li, A., Fan, L., Xie, L., Ren, Y., & Li, L. (2018). Associations between air pollution, climate factors and outpatient visits for eczema in West China Hospital, Chengdu, south-western China: A time series analysis. Journal of the European Academy of Dermatology and Venereology, 32(3), 486–494. https://doi.org/10.1111/jdv.14730.
Li, Q., Yang, Y., Chen, R., Kan, H., Song, W., Tan, J., et al. (2016). Ambient Air Pollution, Meteorological Factors and Outpatient Visits for Eczema in Shanghai, China: A Time-Series Analysis. International Journal of Environmental Research and Public Health, 13(11), doi:https://doi.org/10.3390/ijerph13111106.
Liu, F., Qu, F., Zhang, H., Chao, L., Li, R., Yu, F., et al. (2019). The effect and burden modification of heating on adult asthma hospitalizations in Shijiazhuang: a time-series analysis. Respiratory Research, 20(1), 122. https://doi.org/10.1186/s12931-019-1092-0.
Liu, M., Lin, J., Wang, Y., Sun, Y., Zheng, B., Shao, J., et al. (2018a). Spatiotemporal variability of NO2 and PM2.5 over Eastern China: Observational and model analyses with a novel statistical method. Atmospheric Chemistry and Physics Discussions, 1–34, doi:https://doi.org/10.5194/acp-2017-1180.
Liu, W., Cai, J., Huang, C., Hu, Y., Fu, Q., Zou, Z., et al. (2016). Associations of gestational and early life exposures to ambient air pollution with childhood atopic eczema in Shanghai, China. Science of the Total Environment, 572, 34–42. https://doi.org/10.1016/j.scitotenv.2016.07.197.
Liu, W., Pan, X., Vierkotter, A., Guo, Q., Wang, X., Wang, Q., et al. (2018). A time-series study of the effect of air pollution on outpatient visits for acne vulgaris in Beijing. Skin Pharmacol Physiol, 31(2), 107–113. https://doi.org/10.1159/000484482.
Lu, C., Cao, L., Norback, D., Li, Y., Chen, J., & Deng, Q. (2019). Combined effects of traffic air pollution and home environmental factors on preterm birth in China. Ecotoxicology and Environmental Safety, 184, 109639. https://doi.org/10.1016/j.ecoenv.2019.109639.
Luo, K., Li, R., Li, W., Wang, Z., Ma, X., Zhang, R., et al. (2016). Acute effects of nitrogen dioxide on cardiovascular mortality in Beijing: An exploration of spatial heterogeneity and the district-specific predictors. Sci Rep, 6(1), 38328. https://doi.org/10.1038/srep38328.
Ma, W., Wang, L., Lin, H., Liu, T., Zhang, Y., Rutherford, S., et al. (2015). The temperature-mortality relationship in China: An analysis from 66 Chinese communities. Environmental Research, 137, 72−77. https://doi.org/10.1016/j.envres.2014.11.016.
Mirvish, S. S., Sams, J. P., & Issenberg, P. (1983). The nitrosating agent in mice exposed to nitrogen dioxide: Improved extraction method and localization in the skin. Cancer Research, 43(6), 2550–2554.
Noh, S. R., Kim, J. S., Kim, E. H., Jeon, B. H., Kim, J. H., Kim, Y. M., et al. (2019). Spectrum of susceptibility to air quality and weather in individual children with atopic dermatitis. Pediatric Allergy and Immunology, 30(2), 179–187. https://doi.org/10.1111/pai.13005.
Ogen, Y. (2020). Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Science of the Total Environment,726, 138605. https://doi.org/10.1016/j.scitotenv.2020.138605.
Penard-Morand, C., Raherison, C., Charpin, D., Kopferschmitt, C., Lavaud, F., Caillaud, D., et al. (2010). Long-term exposure to close-proximity air pollution and asthma and allergies in urban children. European Respiratory Journal, 36(1), 33–40. https://doi.org/10.1183/09031936.00116109.
Permaul, P., Gaffin, J. M., Petty, C. R., Baxi, S. N., Lai, P. S., Sheehan, W. J., et al. (2020). Obesity may enhance the adverse effects of NO2 exposure in urban schools on asthma symptoms in children. The Journal of Allergy and Clinical Immunology. https://doi.org/10.1016/j.jaci.2020.03.003.
Pesce, G., Marcon, A., Carosso, A., Antonicelli, L., Cazzoletti, L., Ferrari, M., et al. (2015). Adult eczema in Italy: prevalence and associations with environmental factors. Journal of the European Academy of Dermatology and Venereology, 29(6), 1180–1187. https://doi.org/10.1111/jdv.12784.
Prescott, S. L., Larcombe, D. L., Logan, A. C., West, C., Burks, W., Caraballo, L., et al. (2017). The skin microbiome: Impact of modern environments on skin ecology, barrier integrity, and systemic immune programming. World Allergy Organization Journal,10(1), 29. https://doi.org/10.1186/s40413-017-0160-5.
Ritz, B., Hoffmann, B., & Peters, A. (2019). The effects of fine dust, ozone, and nitrogen dioxide on health. Deutsches Aerzteblatt Online. https://doi.org/10.3238/arztebl.2019.0881.
Ryu, Y. S., Kang, K. A., Piao, M. J., Ahn, M. J., Yi, J. M., Bossis, G., et al. (2019). Particulate matter-induced senescence of skin keratinocytes involves oxidative stress-dependent epigenetic modifications. Experimental & Molecular Medicine,51(9), 108. https://doi.org/10.1038/s12276-019-0305-4.
Schnass, W., Huls, A., Vierkotter, A., Kramer, U., Krutmann, J., & Schikowski, T. (2018). Traffic-related air pollution and eczema in the elderly: Findings from the SALIA cohort. International Journal of Hygiene and Environmental Health,221(6), 861–867. https://doi.org/10.1016/j.ijheh.2018.06.002.
Mirvish, S. S., Ramm, M. D., Sams, J. P., & Babcook, D. M. (1988). Nitrosamine formation from amines applied to the skin of mice after and before exposure to nitrogen dioxide nitrosamine formation from amines applied to the skin of mice. Cancer Research,48, 1095–1099.
Song, J., Liu, Y., Lu, M., An, Z., Lu, J., Chao, L., et al. (2019). Short-term exposure to nitrogen dioxide pollution and the risk of eye and adnexa diseases in Xinxiang China. Atmospheric Environment, 218, 117001. https://doi.org/10.1016/j.atmosenv.2019.117001.
Song, J., Lu, M., Zheng, L., Liu, Y., Xu, P., Li, Y., et al. (2018). Acute effects of ambient air pollution on outpatient children with respiratory diseases in Shijiazhuang China. BMC Pulmonary Medicine, 18(1), 150. https://doi.org/10.1186/s12890-018-0716-3.
Sun, L., Liu, W., & Zhang, L. J. (2019). The role of toll-like receptors in skin host defense, psoriasis, and atopic dermatitis. Journal of Immunolgy Research,2019, 1824624. https://doi.org/10.1155/2019/1824624.
Wang, L., Zhang, F., Pilot, E., Yu, J., Nie, C., Holdaway, J., et al. (2018). Taking action on air pollution control in the Beijing-Tianjin-Hebei (BTH) region: Progress, challenges and opportunities. International journal of environmental research and public health,15(2), 306. https://doi.org/10.3390/ijerph15020306.
Yan, W., Yue, H., Ji, X., Li, G., & Sang, N. (2020). Prenatal NO2 exposure and neurodevelopmental disorders in offspring mice: Transcriptomics reveals sex-dependent changes in cerebral gene expression. Environment International, 138, 105659. https://doi.org/10.1016/j.envint.2020.105659.
Funding
The study was supported by the Ph.D. Research Project of Xinxiang Medical University (XYBSKYZZ201804), Key Scientific Research Projects in Universities of Henan (19B330004) and Peak Subject Project of Public Health in Xinxiang Medical University.
Author information
Authors and Affiliations
Contributions
Ling Chao: Investigation, Methodology, Data curation, Validation, Visualization, Software, Formal analysis, writing—original draft. Mengxue Lu: Methodology, Software, Validation, Visualization, Writing—review. Zhen An: Investigation, Methodology, Validation. Juan Li: Investigation, Methodology, Validation. Yuchun Li: Investigation, Methodology, Validation. Qian Zhao: Investigation, Methodology, Validation. Yinbiao Wang: Investigation, Methodology, Validation. Yue Liu: Investigation, Methodology, Validation. Weidong Wu: Investigation, Methodology, Validation. Jie Song: Conceptualization, Funding acquisition, Supervision, Writing—review & editing, Project administration, Resources, Validation.
Corresponding author
Ethics declarations
This is an observational study. The XYZ Research Ethics Committee has confirmed that no ethical approval is required.
Conflict of interest
The authors state that they have no conflicts to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chao, L., Lu, M., An, Z. et al. Short-term effect of NO2 on outpatient visits for dermatologic diseases in Xinxiang, China: a time-series study. Environ Geochem Health 43, 1–11 (2021). https://doi.org/10.1007/s10653-021-00831-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10653-021-00831-3