Summary
Background Overexpression of apurinic/apyrimidinic endonuclease 1 (APE1) is an important cause of poor chemotherapeutic efficacy in advanced non-small cell lung cancer (NSCLC) patients. Gossypol, a new inhibitor of APE1, in combination with docetaxel and cisplatin is believed to improve the efficacy of chemotherapy for advanced NSCLC with high APE1 expression. Methods Sixty-two patients were randomly assigned to two groups. Thirty-one patients in the experimental group received 75 mg/m2 docetaxel and 75 mg/m2 cisplatin on day 1 with gossypol administered at 20 mg once daily on days 1 to 14 every 21 days. The control group received placebo with the same docetaxel and cisplatin regimen. The primary endpoint was progression-free survival (PFS); secondary endpoints included overall survival (OS), response rate, and toxicity. Results There were no significant differences in PFS and OS between the experimental group and the control group. The median PFS (mPFS) in the experimental and control groups was 7.43 and 4.9 months, respectively (HR = 0.54; p = 0.06), and the median OS (mOS) was 18.37 and 14.7 months, respectively (HR = 0.68; p = 0.27). No significant differences in response rate and serious adverse events were found between the groups. Conclusion The experimental group had a better mPFS and mOS than did the control group, though no significant difference was observed. Because the regimen of gossypol combined with docetaxel and cisplatin was well tolerated, future studies with larger sample sizes should be performed.
Similar content being viewed by others
Introduction
Non-small cell lung cancer (NSCLC) is the most common type of lung cancer, and more than 70% of NSCLC patients are diagnosed with advanced-stage disease (stage III, local progression or stage IV, distant metastasis); thus, the majority of these patients have lost the opportunity for surgical resection [1]. Platinum-based chemotherapy is the cornerstone of treatment for advanced NSCLC [2]. However, chemotherapy is only beneficial for a few patients with advanced NSCLC: the median progression-free survival (mPFS) is 4.2 to 5.5 months [2,3,4], the median overall survival (mOS) is only 8.5 to 10.5 months [4,5,6], and the 5-year survival rate is still less than 10% [7]. Overall, platinum-containing chemotherapeutic drugs may have reached a plateau for the treatment of advanced NSCLC, and platinum resistance may be a key factor in the limited efficacy.
The main antitumor mechanism of platinum drugs involves platinum binding to DNA to form a platinum-DNA adduct, which disrupts DNA replication via intrastrand crosslinking, resulting in DNA damage and cell death [8]. Alterations in DNA repair capacity are an important molecular basis of platinum resistance [9, 10]. The stronger is the DNA repair capacity of the tumor, the more resistant it is to chemotherapeutic drugs. Apurinic/apyrimidinic endonuclease 1 (APE1) is a biomacromolecule functional complex that has dual functions in DNA damage repair and redox [11,12,13,14]. On the one hand, APE1 is the main rate-limiting enzyme in the base excision repair pathway and is involved in the DNA damage repair of purine/pyrimidine deletion sites (AP sites) caused by oxidants and alkylating agents. On the other hand, APE1 is an important mediator in the cellular oxidative stress response pathway. By maintaining the reductive state of DNA binding region-specific cysteines and maintaining the activation and reduction of various transcription factors (such as AP-1, NF-kappa B, Myb, HIF-1α, HLF, PAX, p53), this complex is indirectly involved in the regulation of gene expression [15, 16]. Some of these transcription factors are closely related to chemotherapeutic resistance [17, 18].
Many studies have shown that APE1 expression is increased in various malignant tumors, including NSCLC [19], colorectal cancer [20], ovarian cancer [21, 22], glioma [23], cervical cancer [24], prostate cancer [25] and pancreatic cancer [26]. This increase in APE1 expression is associated with chemotherapeutic resistance [27]. Our previous study confirmed that downregulating APE1 protein expression can increase the sensitivity of A549 lung cancer cell lines to platinum [28]. Clinical data have also confirmed that the survival time of patients with low expression of APE1 is longer than that of patients with high expression of APE1 after platinum adjuvant chemotherapy [28]. Thus, inhibition of APE1 may improve the sensitivity of NSCLC to platinum-containing regimens.
Small molecule inhibitors of APE1 have become a focus of research in this field, but the APE1 inhibitors available only target one of its functions. For example, E3330 only inhibits the redox activity of APE1 but does not affect its endonuclease activity [29]; CRT0044876 only blocks its repair function [30]. In our previous screening of small molecule inhibitors of APE1, we found that gossypol might constitute a new type of inhibitor that simultaneously interferes with both functions of APE1 [31]. Therefore, gossypol combined with platinum has important clinical value in the treatment of NSCLC patients with high APE1 expression. This study is a prospective, randomized clinical trial to assess whether gossypol can enhance the efficacy of docetaxel and cisplatin in patients with high expression of APE1, to provide a new target for targeted chemotherapy of NSCLC and to test a safe and economical combination of drugs to improve the efficacy of advanced NSCLC chemotherapy.
Materials and methods
Diagnostic criteria
The diagnosis was made according to the 6th Edition of Oncology Diagnostics and the 6th Edition of Internal Medicine published by the People’s Health Publishing House of the People’s Republic of China.
Inclusion criteria
Eligible patients were confirmed to have advanced NSCLC (IIIB/IV) with evaluable lesions by histology or cytology. High expression of APE1 (+++) was detected by immunohistochemistry. All patients, aged between 18 and 75 years, had not previously received platinum-based chemotherapy and had no epidermal growth factor receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK) positivity. The patients may have had a history of brain/meningeal metastasis but underwent local treatment (surgery/radiotherapy) before randomization and were clinically stable for at least 2 months. Eligibility criteria included a performance status (PS) of 0 to 1 and an estimated survival time ≥ 3 months. Routine blood examination results were as follows: hemoglobin ≥ 90 g/L (within 14 days without blood transfusion), absolute neutrophil count ≥ 1.5 × 109/L, and platelet ≥ 80 × 109/L. Biochemical analyses met the following criteria: (1) bilirubin < 1.25 × the upper limit of normal (ULN); (2) alanine aminotransferase and aspartate transaminase < 2.5 × ULN (with liver metastasis, alanine aminotransferase and aspartate transaminase < 5 × ULN); and (3) serum creatinine ≤ 1.25 ml/min; creatinine clearance > 45 ml/min. This trial was consistent with the Helsinki Declaration and was approved by the Ethics Committee of Daping Hospital & Army Medical Center of PLA.
Drug source
The experimental drug was compound gossypol acetate tablets (specification: 20 mg/tablet), which were produced by Xi’an Northern Pharmaceutical Co., Ltd. The control drug was a placebo (gossypol simulated tablet), which was developed and provided by Jiangsu Yasheng Pharmaceutical Development Co., Ltd. The specifications of docetaxel, which was produced by Jiangsu Hengrui Pharmaceutical Co., Ltd., were 20 mg/bottle. Cisplatin was produced by Jiangsu Hausen Pharmaceutical Co., Ltd. with specifications of 10 mg/bottle.
Treatment
The study was randomized and placebo controlled (clinical trial information: NCT01977209), and the patients were randomly assigned to two groups. The experimental group received 75 mg/m2 docetaxel and 75 mg/m2 cisplatin on day 1 with 20 mg gossypol once daily from days 1 to 14 every 21 days. The control group received the same docetaxel and cisplatin regimen as the placebo. Corticosteroids and 5-hydroxytryptamine receptor antagonists were administered on the first and second days of chemotherapy. Patients received at least 4 cycles of treatment in the event of unacceptable toxicity or progressive disease (PD). The full analysis set (FAS) included all patients who had been treated with at least one cycle of treatment and left imaging data records. Effectiveness was evaluated every 6 weeks by computed tomography or other imaging modalities. If the subjects discontinued treatment before the appearance of PD, they were followed up every 42 days for imaging examination to determine if the tumor was progressing. No other antitumor therapy was administered before PD.
Response and toxicity evaluation
NCI-CTC2.0 (National Cancer Institute Common Toxicity Criteria version 2.0) and RECIST1.1 (Response Evaluation Criteria in Solid Tumors guidelines version 1.1) were used to evaluate and grade toxicity and to assess response, respectively. All imaging data were retained and submitted to the independent imaging evaluation committee, which was not related to the trial, to evaluate the curative effect.
Study endpoint and follow-up
Progression-free survival (PFS) was the primary endpoint of the study. The secondary endpoints were overall survival (OS), objective response rate (ORR), disease control rate (DCR), toxicity and safety. PFS was defined as the time between the date on which the patient was randomly enrolled into a group and the date of any recorded PD or death from any cause. Recurrence, appearance of new lesions or death was considered the end of the study for that case, and the use of other systemic or target antitumor therapies was also considered PD. For patients who had not yet experienced PD or death at the end of the study, the time of the last record was considered to be censored data. For patients who were lost to follow-up without PD, these data were also censored if the imaging data were recorded.
Statistical analysis
The sample size was calculated under the assumption that mPFS increased from 4.5 months to 8 months. With an α error of 5%, a β error of 20%, and a predicted 10% of cases lost to follow-up, our anticipated sample size was 256 cases.
All statistical analyses were performed with Statistical Package for Social Sciences (SPSS, Version 23) software. Intent-to-treat (ITT) analysis was performed for data for all patients who entered the study and received treatment. T-tests, chi-square tests and Fisher’s exact tests were employed to evaluate whether the baseline characteristics of the two groups were comparable. OS and PFS were evaluated by stratified log-rank tests, and the results are summarized by a Kaplan-Meier survival curve. All statistical tests were two-sided, and a p value ≤ 0.05 was considered significant. Furthermore, we calculated the hazard ratio (HR) with the 95% confidence interval (CI).
Results
Patient characteristics
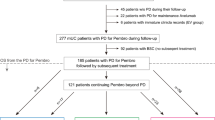
From January 2014 to February 2017, only 102 patients signed informed consent and participated in the study (50 in the experimental group and 52 in the control group). However, because of the poor compliance of patients with advanced NSCLC, 40 were lost to follow-up after only one chemotherapy session without reexamination (19 in the experimental group and 21 in the control group); as no imaging data were available, these cases were excluded. Only 62 cases were in accordance with the analysis. Sixty-two patients (ITT set) were randomly assigned to two groups: 31 received gossypol plus docetaxel and cisplatin, and 31 received the placebo plus docetaxel and cisplatin; all patients received at least one cycle of treatment (Fig. 1). In the placebo group, 31 patients received a total of 88 cycles, with a mean of 2.8 cycles. In the experimental group, fifteen patients (48%) completed four cycles of gossypol plus docetaxel and cisplatin, 8 patients (26%) received three cycles, seven (23%) received two cycles, and 1 (3%) received one cycle.
Table 1 lists the baseline characteristics of the patients, and the two groups of the study were demographically balanced, with no significant differences (p > 0.05). Among all patients, 38 had stage IIIb disease (20 adenocarcinoma, 17 squamous, 1 sarcomatous carcinoma), and 24 had stage IV disease (21 adenocarcinoma and 3 squamous). In the gossypol group, there were 23 males, with a mean age of 56.25 years. Among the 31 patients, 18 smoked, 25 had a PS score of 1, and 5 had only 1 metastatic disease site. The placebo group included 6 females, with a mean age of 59.41 years; 12 were nonsmokers, 7 had a PS score of 0, and 19 had at least 2 metastatic disease sites.
Comparison of short-term efficacy between the two groups
All 62 patients were evaluated for response. No complete responses (CRs) were observed in this study. There were 3 and 1 cases of partial response (PR) in the gossypol and placebo groups, respectively. This finding corresponds to ORRs of 9.7% and 3.2%, respectively. The best response recorded as SD was observed in 23 and 18 patients in the gossypol and placebo groups, respectively. The DCRs were 83.9% and 61.3%, respectively (Table 2).
Comparison of long-term efficacy between the two groups
Forty-four patients (72%), 22 in the gossypol group and 22 in the placebo group, had an event for PFS. In the gossypol group, 17 patients had objective PD, five died due to progression, and 9 were lost to follow-up before PD. In the placebo group, 21 patients had objective PD, one died without objective PD, and nine were lost to follow-up. For OS, 36 patients died, and 26 patients were censored (5 patients with ongoing response). Figure 2 shows the therapeutic process and outcomes for the evaluable patients.
mPFS in the gossypol and placebo groups was 7.43 and 4.9 months, respectively [p = 0.06, HR (95% CI): 0.54 (0.29–1.03)]. The 6-month PFS rate in the gossypol group was 45.2% (Fig. 3), which was higher than that in the placebo group (22.6%). mOS in the gossypol and placebo groups was 18.37 and 14.7 months, respectively [p = 0.27, HR (95% CI): 0.68 (0.34–1.34)]. The benefits for OS remained unchanged during longer follow-up. There were 17 vs. 10 patients who survived more than 12 months in the gossypol group vs. the placebo group (Fig. 4).
Safety and toxicity
There were no treatment-related deaths or discontinuation of treatment due to toxicity. As shown in Table 3, only 1 patient had grade 3 anemia in the gossypol group, but we did not reduce the dose level because the hemoglobin level in that patient later returned to normal. Most patients had mild events (grade 1 or 2 toxicity): the number of patients with anemia in the placebo group was greater than that in the gossypol group (7 vs. 3); 2 patients had neutropenia and three had asthenia in the gossypol group, and 3 patients had leukopenia and three patients had thrombocytopenia in the placebo group. There was no significant increase in toxicity in the gossypol group compared with the placebo group.
Discussion
This study was intended to improve the primary endpoint of PFS. However, the results showed no significant differences in PFS and OS between the gossypol and placebo groups (p > 0.05). Nonetheless, the DCR for the gossypol group improved by 22.6% compared with that of the placebo group. Moreover, gossypol combined with docetaxel and cisplatin was well tolerated, and there was no significant increase in toxicity for the gossypol group compared with the placebo group. The vast majority of events for this study were grade 1 or 2 toxicity, and only one patient with grade 3 neutropenia was found in the experimental group.
Unlike targeted drugs for the treatment of NSCLC, chemotherapeutic drugs (including platinum) are usually administered based on the response rate in previous trials to cancer patients who do not have any specific gene targets. A comparison of serum APE1 protein levels of 523 healthy blood donors with APE1 protein levels in biopsies from 172 NSCLC patients and serum of 412 NSCLC patients receiving platinum chemotherapy showed that APE1 is a predictive biomarker for NSCLC prognosis and treatment effect [32]. Another clinical study was conducted to confirm the role of APE1 in the chemosensitivity of NSCLC to the platinum regimen [33], with 172 patients with advanced NSCLC receiving at least two cycles. APE1 protein expression was detected by immunohistochemistry and used to evaluate the relationship between protein expression and platinum chemotherapy. The results showed an APE1 positivity rate of 75.74%. The chemotherapeutic response rate of patients without expression of APE1 was 48.48%, which was significantly higher than that of APE1-positive patients (26.21%). The mPFS of patients without APE1 expression was significantly longer than that in APE1-positive patients (11.1 vs. 8.4 months and p = 0.008). Gossypol, an inhibitor of APE1, is a natural compound extracted from cottonseed that was originally used as an antifertility agent and later as a cytotoxic agent [34,35,36]. It has been proven to be a antineoplastic drug that can act on various cancers [37,38,39,40]. Although the antitumor mechanism of gossypol has not been fully clarified, its molecular targets are gradually being revealed. As an inhibitor of various B-cell lymphoma 2 (Bcl-2) molecules and a nonselective Bcl-2 homology 3 (BH3) analog, gossypol can bind to the BH3 domain of members of the Bcl-2 family (such as Bcl-2, Bcl-XL, Mcl-1, Bcl-W), inactivate their functions and promote apoptosis [41]. Gossypol not only specifically binds to intracellular BH3 sites and replaces apoptotic proteins such as Bax/Bak, which can indirectly inhibit the activities of Bcl-2 and Bcl-XL, but it also directly binds to the BH3 sites of proapoptotic proteins such as Bax and Bak to promote apoptosis [42]. Importantly, some studies have found that Bcl-2 directly interacts with APE1 through its BH domain [43], which might be the mechanism by which gossypol acts as an APE1 inhibitor. In our previous study [31], we also showed by dual polarization interferometry technology that gossypol was able to interact directly with APE1 and inhibit the repair activity and redox function of APE1. Furthermore, in human cancer cell lines, gossypol was more effective at killing cancer cells with APE1 overexpression than negative controls, and the combination of gossypol and cisplatin resulted in enhanced cell killing and higher antitumor activity in vivo than cisplatin alone. All of these findings might explain why the gossypol group was superior to the control group with regard to both PFS and OS, and we believe that gossypol combined with the platinum regimen has important clinical value.
In this study, the mPFS of the gossypol group was 2.53 months longer than that of the placebo group (7.43 vs. 4.9 months), and the mOS of the gossypol group increased by 3.67 months compared with that of the placebo group (18.37 vs. 14.7 months). Although these parameters of the gossypol group were better than those of the placebo group, there were no significant differences between the two groups for the following reasons. First, the sample size of this experiment was small. Many patients with advanced NSCLC were treated with chemotherapy after diagnosis in the respiratory department or thoracic surgery, and there were few patients who had not received a first-line platinum regimen directly from the oncology department. Second, many censored cases were included. A total of 18 patients were lost to follow-up before PD, which led to no significant difference between the groups. Similarly, although the DCR in the gossypol group was significantly higher than that in the placebo group, there were no CRs and few cases of PR, which might have been due to the large number of censored cases resulting in insufficient treatment cycle and no corresponding efficacy observed.
Gossypol has been shown to have good safety and tolerance profiles [44, 45]. For instance, clinical trials indicate that gossypol is apparently safe at a dosage of 40 mg/day [37]. A lower dose of 20 mg once daily was chosen in the present study. Compared with previous studies on gossypol [46], our results showed no increase in gastrointestinal toxicities, cardiac rhythm abnormalities, liver damage, or other severe adverse events. Because the compound gossypol acetate tablets provided to the experimental group contain potassium chloride, the patients did not show hypokalemia, which is the most common side effect of gossypol [47]. Only one patient in the gossypol group had grade 3 anemia and hemoglobin of 78 g/L, which may have been caused by gossypol-induced suicidal erythrocyte death [48].
The drugs used in our trial (gossypol, docetaxel and cisplatin) have the advantages of being easily available and affordable. Platinum-containing chemotherapy is the basis for the treatment of advanced NSCLC, and thus, gossypol might be combined with most first-line chemotherapeutic drugs. One limitation of our study was that it was carried out in a single institution. The patients were mostly from Southwest China and were not diverse. Moreover, although all imaging was assessed by seasoned thoracic oncologic radiologists, our trial lacked a centralized, blinded radiology review.
In conclusion, gossypol, as a new small molecule inhibitor of APE1, has the advantages of abundant sources, low cost, high safety, and low toxicity in clinical applications. Although there was no significant difference, the gossypol group had better outcomes of increased mPFS and mOS than the placebo group. The lack of significant differences between the groups may be due to the sample size and the censored data. In the future, we will expand the sample size and improve the follow-up rate of patients to observe the curative effect of this treatment.
Data availability
The data and materials used in this study are available from the corresponding author on reasonable request.
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- mPFS:
-
Median progression-free survival
- mOS:
-
Median overall survival
- APE1:
-
Apurinic/apyrimidinic endonuclease 1
- PS:
-
Performance status
- EGFR:
-
Epidermal growth factor receptor
- ALK:
-
Anaplastic lymphoma kinase
- ULN:
-
Upper limit of normal
- PD:
-
Progressive disease
- FAS:
-
Full analysis set
- NCI-CTC2.0:
-
National Cancer Institute Common Toxicity Criteria version 2.0
- RECIST1.1:
-
Response Evaluation Criteria in Solid Tumors guidelines version 1.1
- ORR:
-
Objective response rate
- DCR:
-
Disease control rate
- ITT:
-
Intent-to-treat
- HR:
-
Hazard ratio
- CR:
-
Complete response
- PR:
-
Partial response
- SD:
-
Stable disease
- CI:
-
Confidence interval
- Bcl-2:
-
B-cell lymphoma 2
- BH3:
-
Bcl-2 homology 3
References
Bai H, Mao L, Wang HS, Zhao J, Yang L, An TT, Wang X, Duan CJ, Wu NM, Guo ZQ, Liu YX, Liu HN, Wang YY, Wang J (2009) Epidermal growth factor receptor mutations in plasma DNA samples predict tumor response in Chinese patients with stages IIIB to IV non-small-cell lung cancer. J Clin Oncol 27(16):2653–2659. https://doi.org/10.1200/JCO.2008.17.3930
Digumarti R, Wang Y, Raman G, Doval DC, Advani SH, Julka PK, Parikh PM, Patil S, Nag S, Madhavan J, Bapna A, Ranade AA, Varadhachary A, Malik R (2011) A randomized, double-blind, placebo-controlled, phase II study of oral talactoferrin in combination with carboplatin and paclitaxel in previously untreated locally advanced or metastatic non-small cell lung cancer. J Thorac Oncol 6(6):1098–1103. https://doi.org/10.1097/JTO.0b013e3182156250
Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, Lilenbaum R, Johnson DH (2006) Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med 355(24):2542–2550. https://doi.org/10.1056/NEJMoa061884
Scagliotti GV, De Marinis F, Rinaldi M, Crino L, Gridelli C, Ricci S, Matano E, Boni C, Marangolo M, Failla G, Altavilla G, Adamo V, Ceribelli A, Clerici M, Di Costanzo F, Frontini L, Tonato M (2002) Phase III randomized trial comparing three platinum-based doublets in advanced non-small-cell lung cancer. J Clin Oncol 20(21):4285–4291. https://doi.org/10.1200/JCO.2002.02.068
Liu SV, Camidge DR, Gettinger SN, Giaccone G, Heist RS, Hodi FS, Ready NE, Zhang W, Wallin J, Funke R, Waterkamp D, Foster P, Iizuka K, Powderly J (2018) Long-term survival follow-up of atezolizumab in combination with platinum-based doublet chemotherapy in patients with advanced non-small-cell lung cancer. Eur J Cancer 101:114–122. https://doi.org/10.1016/j.ejca.2018.06.033
Herbst RS, Prager D, Hermann R, Fehrenbacher L, Johnson BE, Sandler A, Kris MG, Tran HT, Klein P, Li X, Ramies D, Johnson DH, Miller VA, Group TI (2005) TRIBUTE: a phase III trial of erlotinib hydrochloride (OSI-774) combined with carboplatin and paclitaxel chemotherapy in advanced non-small-cell lung cancer. J Clin Oncol 23(25):5892–5899. https://doi.org/10.1200/JCO.2005.02.840
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ (2009) Cancer statistics, 2009. CA Cancer J Clin 59(4):225–249. https://doi.org/10.3322/caac.20006
Shen DW, Pouliot LM, Hall MD, Gottesman MM (2012) Cisplatin resistance: a cellular self-defense mechanism resulting from multiple epigenetic and genetic changes. Pharmacol Rev 64(3):706–721. https://doi.org/10.1124/pr.111.005637
Chen SH, Chang JY (2019) New insights into mechanisms of cisplatin resistance: from tumor cell to microenvironment. Int J Mol Sci 20(17). https://doi.org/10.3390/ijms20174136
Ghosh S (2019) Cisplatin: The first metal based anticancer drug. Bioorg Chem 88:102925. https://doi.org/10.1016/j.bioorg.2019.102925
Hoeijmakers JH (2001) Genome maintenance mechanisms for preventing cancer. Nature 411(6835):366–374. https://doi.org/10.1038/35077232
Tell G, Fantini D, Quadrifoglio F (2010) Understanding different functions of mammalian AP endonuclease (APE1) as a promising tool for cancer treatment. Cell Mol Life Sci 67(21):3589–3608. https://doi.org/10.1007/s00018-010-0486-4
Sun Y, Feng Y, Zhang G, Xu Y (2019) The endonuclease APE1 processes miR-92b formation, thereby regulating expression of the tumor suppressor LDLR in cervical cancer cells. Ther Adv Med Oncol 11:1758835919855859. https://doi.org/10.1177/1758835919855859
Shah F, Goossens E, Atallah NM, Grimard M, Kelley MR, Fishel ML (2017) APE1/Ref-1 knockdown in pancreatic ductal adenocarcinoma - characterizing gene expression changes and identifying novel pathways using single-cell RNA sequencing. Mol Oncol 11(12):1711–1732. https://doi.org/10.1002/1878-0261.12138
Kelley MR, Georgiadis MM, Fishel ML (2012) APE1/Ref-1 role in redox signaling: translational applications of targeting the redox function of the DNA repair/redox protein APE1/Ref-1. Curr Mol Pharmacol 5(1):36–53
Tell G, Quadrifoglio F, Tiribelli C, Kelley MR (2009) The many functions of APE1/Ref-1: not only a DNA repair enzyme. Antioxid Redox Signal 11(3):601–620. https://doi.org/10.1089/ars.2008.2194
Hung JJ, Yang MH, Hsu HS, Hsu WH, Liu JS, Wu KJ (2009) Prognostic significance of hypoxia-inducible factor-1alpha, TWIST1 and Snail expression in resectable non-small cell lung cancer. Thorax 64(12):1082–1089. https://doi.org/10.1136/thx.2009.115691
Mijatovic T, Op De Beeck A, Van Quaquebeke E, Dewelle J, Darro F, de Launoit Y, Kiss R (2006) The cardenolide UNBS1450 is able to deactivate nuclear factor kappaB-mediated cytoprotective effects in human non-small cell lung cancer cells. Mol Cancer Ther 5(2):391–399. https://doi.org/10.1158/1535-7163.MCT-05-0367
Yoo DG, Song YJ, Cho EJ, Lee SK, Park JB, Yu JH, Lim SP, Kim JM, Jeon BH (2008) Alteration of APE1/ref-1 expression in non-small cell lung cancer: the implications of impaired extracellular superoxide dismutase and catalase antioxidant systems. Lung Cancer 60(2):277–284. https://doi.org/10.1016/j.lungcan.2007.10.015
Lou D, Zhu L, Ding H, Dai HY, Zou GM (2014) Aberrant expression of redox protein Ape1 in colon cancer stem cells. Oncol Lett 7(4):1078–1082. https://doi.org/10.3892/ol.2014.1864
Al-Attar A, Gossage L, Fareed KR, Shehata M, Mohammed M, Zaitoun AM, Soomro I, Lobo DN, Abbotts R, Chan S, Madhusudan S (2010) Human apurinic/apyrimidinic endonuclease (APE1) is a prognostic factor in ovarian, gastro-oesophageal and pancreatico-biliary cancers. Br J Cancer 102(4):704–709. https://doi.org/10.1038/sj.bjc.6605541
Zhang Y, Wang J, Xiang D, Wang D, Xin X (2009) Alterations in the expression of the apurinic/apyrimidinic endonuclease-1/redox factor-1 (APE1/Ref-1) in human ovarian cancer and indentification of the therapeutic potential of APE1/Ref-1 inhibitor. Int J Oncol 35(5):1069–1079
Bobola MS, Emond MJ, Blank A, Meade EH, Kolstoe DD, Berger MS, Rostomily RC, Silbergeld DL, Spence AM, Silber JR (2004) Apurinic endonuclease activity in adult gliomas and time to tumor progression after alkylating agent-based chemotherapy and after radiotherapy. Clin Cancer Res 10(23):7875–7883. https://doi.org/10.1158/1078-0432.CCR-04-1161
Xu Y, Moore DH, Broshears J, Liu L, Wilson TM, Kelley MR (1997) The apurinic/apyrimidinic endonuclease (APE/ref-1) DNA repair enzyme is elevated in premalignant and malignant cervical cancer. Anticancer Res 17(5B):3713–3719
Kelley MR, Cheng L, Foster R, Tritt R, Jiang J, Broshears J, Koch M (2001) Elevated and altered expression of the multifunctional DNA base excision repair and redox enzyme Ape1/ref-1 in prostate cancer. Clin Cancer Res 7(4):824–830
Jiang Y, Zhou S, Sandusky GE, Kelley MR, Fishel ML (2010) Reduced expression of DNA repair and redox signaling protein APE1/Ref-1 impairs human pancreatic cancer cell survival, proliferation, and cell cycle progression. Cancer Invest 28(9):885–895. https://doi.org/10.3109/07357907.2010.512816
Luo M, He H, Kelley MR, Georgiadis MM (2010) Redox regulation of DNA repair: implications for human health and cancer therapeutic development. Antioxid Redox Signal 12(11):1247–1269. https://doi.org/10.1089/ars.2009.2698
Wang D, Xiang DB, Yang XQ, Chen LS, Li MX, Zhong ZY, Zhang YS (2009) APE1 overexpression is associated with cisplatin resistance in non-small cell lung cancer and targeted inhibition of APE1 enhances the activity of cisplatin in A549 cells. Lung Cancer 66(3):298–304. https://doi.org/10.1016/j.lungcan.2009.02.019
Luo M, Delaplane S, Jiang A, Reed A, He Y, Fishel M, Nyland RL 2nd, Borch RF, Qiao X, Georgiadis MM, Kelley MR (2008) Role of the multifunctional DNA repair and redox signaling protein Ape1/Ref-1 in cancer and endothelial cells: small-molecule inhibition of the redox function of Ape1. Antioxid Redox Signal 10(11):1853–1867. https://doi.org/10.1089/ars.2008.2120
Al-Safi RI, Odde S, Shabaik Y, Neamati N (2012) Small-molecule inhibitors of APE1 DNA repair function: an overview. Curr Mol Pharmacol 5(1):14–35
Qian C, Li M, Sui J, Ren T, Li Z, Zhang L, Zhou L, Cheng Y, Wang D (2014) Identification of a novel potential antitumor activity of gossypol as an APE1/Ref-1 inhibitor. Drug Des Devel Ther 8:485–496. https://doi.org/10.2147/DDDT.S62963
Zhang S, He L, Dai N, Guan W, Shan J, Yang X, Zhong Z, Qing Y, Jin F, Chen C, Yang Y, Wang H, Baugh L, Tell G, Wilson DM 3rd, Li M, Wang D (2016) Serum APE1 as a predictive marker for platinum-based chemotherapy of non-small cell lung cancer patients. Oncotarget 7(47):77482–77494. https://doi.org/10.18632/oncotarget.13030
Li Z, Qing Y, Guan W, Li M, Peng Y, Zhang S, Xiong Y, Wang D (2014) Predictive value of APE1, BRCA1, ERCC1 and TUBB3 expression in patients with advanced non-small cell lung cancer (NSCLC) receiving first-line platinum-paclitaxel chemotherapy. Cancer Chemother Pharmacol 74(4):777–786. https://doi.org/10.1007/s00280-014-2562-1
Paoluzzi L, Gonen M, Gardner JR, Mastrella J, Yang D, Holmlund J, Sorensen M, Leopold L, Manova K, Marcucci G, Heaney ML, O’Connor OA (2008) Targeting Bcl-2 family members with the BH3 mimetic AT-101 markedly enhances the therapeutic effects of chemotherapeutic agents in in vitro and in vivo models of B-cell lymphoma. Blood 111(11):5350–5358. https://doi.org/10.1182/blood-2007-12-129833
Lu Y, Li J, Dong CE, Huang J, Zhou HB, Wang W (2017) Recent advances in gossypol derivatives and analogs: a chemistry and biology view. Future Med Chem 9(11):1243–1275. https://doi.org/10.4155/fmc-2017-0046
Kim HY, Lee BI, Jeon JH, Kim DK, Kang SG, Shim JK, Kim SY, Kang SW, Jang H (2019) Gossypol suppresses growth of Temozolomide-resistant glioblastoma tumor spheres. Biomolecules 9(10). https://doi.org/10.3390/biom9100595
Van Poznak C, Seidman AD, Reidenberg MM, Moasser MM, Sklarin N, Van Zee K, Borgen P, Gollub M, Bacotti D, Yao TJ, Bloch R, Ligueros M, Sonenberg M, Norton L, Hudis C (2001) Oral gossypol in the treatment of patients with refractory metastatic breast cancer: a phase I/II clinical trial. Breast Cancer Res Treat 66(3):239–248. https://doi.org/10.1023/a:1010686204736
Xiong J, Li J, Yang Q, Wang J, Su T, Zhou S (2017) Gossypol has anti-cancer effects by dual-targeting MDM2 and VEGF in human breast cancer. Breast Cancer Res 19(1):27. https://doi.org/10.1186/s13058-017-0818-5
Lee S, Lee JS, Seo J, Lee SH, Kang JH, Song J, Kim SY (2018) Targeting Mitochondrial Oxidative Phosphorylation Abrogated Irinotecan Resistance in NSCLC. Sci Rep 8(1):15707. https://doi.org/10.1038/s41598-018-33667-6
Yuan Y, Tang AJ, Castoreno AB, Kuo SY, Wang Q, Kuballa P, Xavier R, Shamji AF, Schreiber SL, Wagner BK (2013) Gossypol and an HMT G9a inhibitor act in synergy to induce cell death in pancreatic cancer cells. Cell Death Dis 4:e690. https://doi.org/10.1038/cddis.2013.191
Kitada S, Leone M, Sareth S, Zhai D, Reed JC, Pellecchia M (2003) Discovery, characterization, and structure-activity relationships studies of proapoptotic polyphenols targeting B-cell lymphocyte/leukemia-2 proteins. J Med Chem 46(20):4259–4264. https://doi.org/10.1021/jm030190z
Lian J, Wu X, He F, Karnak D, Tang W, Meng Y, Xiang D, Ji M, Lawrence TS, Xu L (2011) A natural BH3 mimetic induces autophagy in apoptosis-resistant prostate cancer via modulating Bcl-2-Beclin1 interaction at endoplasmic reticulum. Cell Death Differ 18(1):60–71. https://doi.org/10.1038/cdd.2010.74
Zhao J, Gao F, Zhang Y, Wei K, Liu Y, Deng X (2008) Bcl2 inhibits abasic site repair by down-regulating APE1 endonuclease activity. J Biol Chem 283(15):9925–9932. https://doi.org/10.1074/jbc.M708345200
Bushunow P, Reidenberg MM, Wasenko J, Winfield J, Lorenzo B, Lemke S, Himpler B, Corona R, Coyle T (1999) Gossypol treatment of recurrent adult malignant gliomas. J Neurooncol 43(1):79–86. https://doi.org/10.1023/a:1006267902186
Dodou K, Anderson RJ, Small DA, Groundwater PW (2005) Investigations on gossypol: past and present developments. Expert Opin Investig Drugs 14(11):1419–1434. https://doi.org/10.1517/13543784.14.11.1419
Gadelha IC, Fonseca NB, Oloris SC, Melo MM, Soto-Blanco B (2014) Gossypol toxicity from cottonseed products. ScientificWorldJournal 2014:231635. https://doi.org/10.1155/2014/231635
Reidenberg MM, Gu ZP, Lorenzo B, Coutinho E, Athayde C, Frick J, Alvarez F, Brache V, Emuveyan EE (1993) Differences in serum potassium concentrations in normal men in different geographic locations. Clin Chem 39(1):72–75
Zbidah M, Lupescu A, Shaik N, Lang F (2012) Gossypol-induced suicidal erythrocyte death. Toxicology 302(2–3):101–105. https://doi.org/10.1016/j.tox.2012.09.010
Acknowledgements
The authors acknowledge support from the Army Medical Center of PLA, Army Medical University.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81502241) and by the foundation of the Army Medical Center of PLA, Army Medical University (2014YLC01), by the foundation of the Chongqing Science and Technology Commission (cstc2016shms-ztzx10005).
Author information
Authors and Affiliations
Contributions
Yuxiao Wang performed the clinical studies and data acquisition, analyzed and interpreted the data, and drafted the manuscript. Liang Zhang, Mengxia Li and Nan Dai conceptually designed the experiments. Jinlu Shan, Xueqin Yang, Mingfang Xu and Chengxiong Xu performed part of the experiments and edited the manuscript. Yan Feng, Hao Luo and Xuemei Li evaluated the safety and efficacy. Chengyuan Qian and Dong Wang developed the concept for this study and provided technical support and approval of the investigation.
Corresponding authors
Ethics declarations
Conflict of interest
Yuxiao Wang, Liang Zhang, Mengxia Li, Nan Dai, Jinlu Shan, Xueqin Yang, Mingfang Xu, Yan Feng, Hao Luo, Xuemei Li, Chengxiong Xu, Chengyuan Qian and Dong Wang declare that they have no conflicts of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethics committee of the Daping Hospital & Army Medical Center of PLA and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Li, X., Zhang, L. et al. A randomized, double-blind, placebo-controlled study of B-cell lymphoma 2 homology 3 mimetic gossypol combined with docetaxel and cisplatin for advanced non-small cell lung cancer with high expression of apurinic/apyrimidinic endonuclease 1. Invest New Drugs 38, 1862–1871 (2020). https://doi.org/10.1007/s10637-020-00927-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-020-00927-0