Summary
TAS-115 is a novel MET, VEGFR, FMS and PDGFR inhibitor, developed to improve the continuity of drug administration with a relatively short half-life. We assessed its tolerability, safety, pharmacokinetics, efficacy, and pharmacodynamics in patients with solid tumors. This open-label, dose-escalation phase I study of TAS-115 consisted of three parts: part 1 (TAS-115 was administered orally once daily [SID]); part 2 and an expansion part (SID in a 5 days on/2 days off [5-on/2-off] schedule for 21 days per cycle). In part 1 (200–800 mg SID administered to 21 patients), systemic exposure after single administration increased almost dose-proportionally. Three dose-limiting toxicities (DLTs) were observed in three patients: grade 3 rash (650 mg), thrombocytopenia with bleeding, and rash (800 mg). The maximum tolerated dose (MTD) was determined as 650 mg SID. In part 2, the 5-on/2-off schedule was evaluated at the MTD to improve treatment exposure. No DLTs were observed and no patients required treatment interruption in cycle 1. During part 2 and the expansion part (N = 61), grade ≥3 treatment-related adverse events were reported in 47 patients, with neutropenia (24.6%), hypophosphatemia (21.3%), anemia, and thrombocytopenia (14.8% each), and leukocytopenia (11.5%) occurring in ≥10% of patients. The best overall response was stable disease in 31 of 82 patients (37.8%). An apparent reduction in fluorodesoxyglucose-uptake and bone scan index was observed in some patients. TAS-115 was generally well tolerated, with manageable toxicities and recommended phase II dose was estimated as 650 mg SID, 5-on/2-off. Furthermore, promising antitumor activity was observed.
Similar content being viewed by others
Introduction
Vascular endothelial growth factor (VEGF)-mediated angiogenesis is initiated by the binding of VEGF to the specific VEGF receptor (VEGFR) on vascular endothelial cells. VEGFR is subsequently activated via autophosphorylation by tyrosine kinase in the intracellular domain, resulting in signal transduction for cell growth or other events [1]. To date, the blockade of VEGF/VEGFR signal transduction pathways has been demonstrated to inhibit tumor angiogenesis, which leads to the suppression of tumor growth [2].
It has been demonstrated that the binding of hepatocyte growth factor (HGF), a growth factor secreted from tumor cells or surrounding interstitial tissue, to the HGF receptor (MET) induces the autophosphorylation of MET. This then leads to the activation of intracellular signaling cascades involving mitogen-activated protein kinase (MAPK) and phosphatidylinositol 3-kinase (PI3K)/AKT, which in turn promotes proliferation, migration, invasion, and tubulogenesis [3]. In addition, hypoxia in tumor tissues caused by the inhibition of VEGFR has been reported to induce the expression of MET and contribute to the resistance to VEGFR inhibition [4]. McDonough feline sarcoma (FMS), also called colony-stimulating factor-1 receptor (CSF-1R), is a transcription product of the proto-oncogene c-fms [5]. Its ligand CSF-1 (also known as macrophage [M]-CSF) is a hematopoietic growth factor in the mononuclear phagocyte system involved in the differentiation, proliferation, and survival of macrophages [6, 7]. Macrophages exist in various tissues in the body with their known functional diversity and typically include microglia in the brain, osteoclasts involved in bone remodeling, and Kupffer cells participating in lipid metabolism and detoxification in the liver. The abnormal activation of these macrophages causes various disease conditions [8], including increased function of osteoclasts in bone metastases [9]. Platelet-derived growth factor (PDGF), a growth factor primarily involved in migration and proliferation of mesenchymal cells such as fibroblasts, has been reported to participate in various angiogenic processes [10]. Fibroblasts have recently attracted attention for their roles in tumor growth [11, 12].
TAS-115, a novel oral multi-kinase inhibitor, inhibits the autophosphorylation of MET, VEGFR, FMS, PDGF receptor (PDGFR) and other receptors in an adenosine triphosphate (ATP)-competitive manner. The IC50 values of TAS-115 against recombinant VEGFR2 and recombinant MET were 0.030 and 0.032 μmol/L, respectively. In a 192-panel kinase assay, TAS-115 exhibited an IC50 of <1 μmol/L for 53 (28%) kinases, including MET, AXL, c-kit, Src, PDGFR-alpha and –beta [13]. In mouse xenograft models, TAS-115 demonstrated a potent antitumor effect, inhibiting tumor growth and abnormal bone remodeling [13,14,15].
The phase I study (JapicCTI-111645) was initially conducted using a tablet formulation of TAS-115. Ten patients were evaluated and no dose-limiting toxicities (DLTs) were observed at 6 dose levels (100, 200, 400, 800, and 1200 mg once daily [SID], and 400 mg twice daily [BID]). The absorption of TAS-115 was saturated between 100 and 1200 mg. Therefore, it was concluded that the maximum tolerated dose (MTD) could not be determined for the formulation (data on file).
Here, we report an ongoing phase I study, using the granule formulation of TAS-115, to investigate the safety, tolerability, pharmacokinetics (PK), MTD, recommended phase II dose (RP2D), and optimal administration schedule for TAS-115 in patients with advanced solid tumors. Antitumor activity and pharmacodynamics were also evaluated by quantification of changes in pharmacodynamic markers.
Patients and methods
Eligibility
Key inclusion criteria included histologically or cytologically confirmed advanced solid tumors, refractory to standard treatment or with no available standard therapy, age ≥20 years (≥15 years for malignant bone tumors), Eastern Cooperative Oncology Group (ECOG) performance status (PS) 0 or 1, ability to take medications orally, adequate organ function (white blood cell count ≤10,000/mm3, neutrophil count ≥1,500/mm3, hemoglobin ≥9.0 g/dL, platelet count ≥75,000/mm3, serum total bilirubin ≤1.5 mg/dL, serum aspartate aminotransferase [AST] <100 U/L and serum alanine aminotransferase [ALT] <100 U/L, even if serum AST and serum ALT values did not meet the criteria, values of up to 200 U/L or less were acceptable when they were considered to be attributed to the primary disease, estimated creatinine clearance ≥50 mL/min (as per Cockcroft-Gault formula), and life expectancy ≥60 days. Key exclusion criteria included clinically significant heart disease, >grade 1 pre-existing adverse events (AEs) based on Common Terminology Criteria Adverse Events (CTCAE) Version 4.03 [16], brain metastasis with clinical symptoms or requiring treatment, and serious complications.
Study design and treatment
This phase I study (JapicCTI-132333) began on December 1, 2013, and is currently ongoing. This is an open-label, nonrandomized, dose-escalation study conducted at five sites in Japan. The study has three parts: a dose-escalation cohort using a traditional 3 + 3 design (part 1), a dosing schedule investigation cohort (part 2), and an expansion cohort to assess the safety at the MTD or lower doses among more patients (expansion part). TAS-115 was orally administered SID for 21 days per cycle in part 1, and on a 5 days on/2 days off (5-on/2-off) schedule in part 2 and the expansion part (Supplementary Fig. S1).
For each dose level in part 1, three to six patients were enrolled. DLTs were evaluated during the first cycle. As the starting dose in the dose-escalation phase, 200 mg/day was selected, which was decided based on the previous phase I study using TAS-115 tablets and a preclinical study in dogs using a tablet and granule formulations (both, data on file). The study drug was orally administered under empty stomach conditions (1 h before or 2 h after a meal) with a cup of water. In part 2, the TAS-115 dose ≤MTD was administered SID or BID using a 5-on/2-off schedule. In the expansion part, ≤MTD was investigated for exposure and safety. Based on the efficacy among initially treated patients with bone lesions, we focused on enrolling patients with bone metastases or osteosarcoma in the expansion part. Additionally, castration-resistant prostate cancer (CRPC) patients with bone metastases were treated with TAS-115 450 mg/day because five of six CRPC patients who had received 650 mg/day in the early expansion part had AEs requiring dose reduction.
All patients in parts 1 and 2 were required to be hospitalized for cycle 1 in order to observe AE. Patients continued to receive the study drug until disease progression or intolerable toxicity. TAS-115 dose interruption criteria included neutrophil count <500/mm3, platelet count <50,000/mm3, grade ≥3 nonhematologic toxicity, and any toxicity at the investigator’s discretion. Patients with continuous dose interruptions for ≥22 days discontinued treatment, except in cases where the clinical benefit of TAS-115 was strongly suspected. A treatment-related AE (TRAE) that fell under DLT occurred during the treatment period required the dose reduction of TAS-115. If a grade ≥2 event or continuing grade 1 event of decreased appetite, malaise, nausea or vomiting which might affect the treatment continuation occurred, the investigator or sub-investigator had to consider the dose reduction. The range of dose reduction was 25% of the dose that led to the decision of dose reduction. The number of dose reductions was up to 2, and the minimum dose was 100 mg/day.
Dose resumption and elevation criteria are shown in Supplementary Table S1.
Purpose and assessments
The primary objective was to determine the MTD and RP2D of TAS-115 in patients with advanced solid tumors. The MTD was determined based on DLTs during the first cycle and defined as the highest dose where DLT incidence was <33%. DLTs were defined as grade 4 neutropenia >7 days despite G-CSF use; grade 4 febrile neutropenia (≥38.3 °C [101 °F] of >24-h duration); grade 3 or 4 decrease in platelet count associated with bleeding or grade 4 decrease in platelet count of >7 days duration and not resolved with blood transfusion; grade 3 or 4 nonhematologic toxicity not responding to supportive care; or toxicity requiring discontinuation for >7 days.
The secondary objectives were to investigate the PK profile, safety, tolerability, antitumor activity, and pharmacodynamic profile of TAS-115. AEs were graded according to the CTCAE Version 4.03. Response was assessed by radiologic imaging at 6 and 12 weeks from the first dose, and every 12 weeks thereafter. Antitumor effect was evaluated by investigators using Response Evaluation Criteria in Solid Tumors (RECIST) Version 1.1 [17]. If a patient had bone lesions, evaluation was performed using bone scintigraphy and bone scan index (BSI) were calculated by BONENAVI® software (FUJIFILM Toyama Chemical, Co., Ltd., Japan). BSI response was defined as ≥30% reduction in BSI [18]. An exploratory objective was to assess changes in protein levels of soluble MET (sMET), VEGF, and soluble VEGFR2 (sVEGFR2) in plasma, and HGF in serum as pharmacodynamic markers.
Pharmacokinetic and pharmacodynamic sampling
Blood samples were collected for plasma PK assessments pre-dosing and at 1, 2, 3, 4, 6, 8, 12, and 24 h after TAS-115 administration on Days 1 and 8 of cycle 1 in part 1, and on Days 1, 8, and 19 of cycle 1 in part 2 (only pre-dosing on Day 8). TAS-115 concentrations were measured by validated liquid chromatography-tandem mass spectrometry. A preliminary assessment of the effect of food on the PK profile was performed. Blood samples after administration under fed and empty stomach conditions were collected from the first six patients in the expansion part. Pharmacokinetic parameters were determined using non-compartmental analyses (Phoenix® WinNonlin® version 6.4; Certara LP, Princeton, NJ, USA).
For pharmacodynamic analyses, blood samples were collected on Days 1 and 22 (before dosing, each) in part 1, and Days 1 (pre-dosing) and 19 (pre- and post 6 h) in part 2 and the expansion part. Patients provided written informed consent to provide blood samples for exploratory pharmacodynamics assessments.
Statistics
The planned sample size was up to 90 patients, and it was not based on the formal calculation because of experimental phase I trial. For pharmacodynamics parameters, P values were calculated using the paired t-test for measured values from merged doses. The data cut-off date for the analyses presented in this report was August 19, 2018. This study is registered with Japan Pharmaceutical Information Center Clinical Trial registry, number JapicCTI-132333.
Results
Patient disposition and characteristics
Sixty-seven patients received treatment until the cut-off date. A total of 21 patients (three patients for each of the 200, 300, and 450 mg cohorts, and six patients for each of the 650 and 800 mg cohorts) were treated and evaluable for DLTs in part 1. Based on DLTs in cycle 1 of part 1, six patients subsequently received 650 mg SID (MTD) in part 2. In the expansion part, 46 patients received 650 mg SID and nine CRPC patients received 450 mg SID using a 5-on/2-off schedule up to 21 days per cycle. Baseline characteristics of patients are presented in Table 1.
Determination of MTD and RP2D
Overall, three DLTs were reported: grade 3 rash in one patient who received 650 mg SID, and grade 3 thrombocytopenia with bleeding and grade 3 rash each in one patient receiving 800 mg SID. Therefore, the MTD was determined as 650 mg in part 1. However, all patients who received 650 mg SID required treatment interruption during cycle 1 because of AEs (hypophosphatemia, decreased appetite, fibrin D dimer increased, and rash).
When the 650 mg SID dose was repeated using a 5-on/2-off schedule with the aim of improving administration sustainability in part 2, no DLTs were reported, and no patients required treatment interruption in cycle 1. Furthermore, the median relative dose intensity improved from 58% (part 1 level 4) to 100% (part 2) for the 650 mg dose level during cycle 1. The RP2D was estimated as 650 mg 5-on/2-off for 21 days per cycle.
Pharmacokinetic profile
TAS-115 was rapidly absorbed after oral administration, with the median time to maximum concentration (tmax) of 1.0–2.0 h. The area under the curve from 0 to 24 h (AUC0–24) after single administration increased dose-proportionally over the tested range from 200 mg to 650 mg in part 1, although dose-dependent increase between 650 mg and 800 mg was not seen. The 800 mg dose is only approximately 1.2 times the 650 mg dose, and there were large variations between individual patients (Fig. 1a and Supplementary Table S2). Multiple dosing of TAS-115 for 8 days results in no accumulation in part 1 (Supplementary Table S2). In part 2, the exposure of TAS-115 after multiple administration was similar to the dose level of 650 mg in part 1 (Fig. 1b). The mean and individual PK parameters (maximum plasma concentration [Cmax], and AUC0–24) under empty stomach and fed condition were shown in Fig. 1c. The geometric mean ratios (90% CI) of the Cmax and AUC0–24 under fed condition to those under empty stomach condition were 0.545 (0.243–1.224) and 0.812 (0.414–1.593), respectively, however, there were no statistically significant differences.
Correlation of Cmax and AUC0–24 with TAS-115 dose on a Day 1 and b Day 8 (in part 1) or Day 19 (in part 2 and the expansion part), and c preliminary assessment of food effect on the pharmacokinetics of TAS-115 (in the expansion part). Each plot of a circle, triangle, or square indicates a particular patient in parts 1 and 2, and a bar indicates the mean value at each dose level. AUC0–24 area under the time-concentration curve from 0 to 24 h, Cmax maximum plasma concentration
Safety
The most common TRAEs were laboratory abnormalities, gastrointestinal symptoms, general disorders, and skin disorders. In part 1, grade ≥3 TRAEs were reported in 13 patients and no dose-dependent increase in the incidence and grade of TRAEs was observed (Supplementary Table S3). During part 2 and the expansion part (N = 61), the most common TRAEs occurred in more than 30% of patients were increased AST (31patients, 50.8%), fatigue (27 patients, 44.3%), nausea and decreased appetite (26 patients, 42.6% each), increased ALT (23 patients, 37.7%), neutropenia and anemia (21 patients, 34.4% each), hypophosphatemia (20 patients, 32.8%), vomiting and thrombocytopenia (19 patients, 31.1% each). Grade ≥3 TRAEs were reported in 47 patients (77.0%), with neutropenia, hypophosphatemia, anemia, thrombocytopenia, leukocytopenia occurring in ≥10% of patients (Table 2).
TRAEs that led to treatment discontinuation were rash (one patient, 800 mg) in part 1, rash (two patients, 650 mg), pyrexia, peritonitis and neutropenia (one patient each, 650 mg) in part 2 and expansion part. All the patients in cohorts 650 mg and 800 mg in part 1 experienced TRAEs leading to dose interruption, while the frequency in part 2 and the expansion part was decreased (approximately 77%). Serious AEs were reported in seven patients in part 1, two patients in part 2 and thirty one patients in the expansion part. Serious TRAEs were tumor hemorrhage and decreased appetite (one patient, 650 mg each), thrombocytopenia (one patient, 800 mg) in part 1, peritonitis (one patient) in part 2, decreased appetite (three patients), nausea (two patients), interstitial lung disease, rash, enterocolitis, fatigue, thrombocytopenia, and pyrexia (one patient each) in the expansion part. AEs resulted in death were hepatic failure, disease progression and respiratory failure occurred in one patient each in the expansion part (650 mg) and this was not considered related to TAS-115. No treatment-related death was observed in any of the study parts during the treatment period or within 28 days of the last dose of TAS-115.
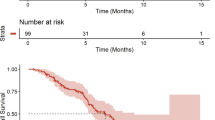
Antitumor effects
Of the 82 patients in all parts, the best overall response was stable disease (SD) in 31 patients (37.8%), and of these, seventeen patients (8 for osteosarcoma, 4 for prostate cancer and 1 each for bladder cancer, renal cancer, breast cancer, clear cell sarcoma, and gastrointestinal stromal tumor [GIST]), had SD lasting 12 weeks or more. Minor tumor shrinkage of target lesions was reported in four patients who were determined as having progressive disease (PD).
BSI response rate in patients with bone lesions was 56.0% (14 of 25) among the patients in whom percentage change in BSI was assessed between baseline and at least once post-scan. The primary cancer types of the responders were osteosarcoma in 6 patients, prostate cancer in five patients, epithelioid sarcoma, clear cell sarcoma, and breast cancer in one patient each. The percent change from baseline is shown in the waterfall plots (Fig. 2). The BSI analysis indicated a definite decrease in the quantitative value of primary lesions or metastases to the bone in several patients.
Figure 3 shows the representative antitumor effect of TAS-115 as observed in three patients who received 650 mg in a 5-on/2-off schedule. A marked decrease of hot spots on bone scans and reduction in fluorodesoxyglucose uptake were observed 6 weeks after the first administration in a patient with epithelioid sarcoma with multiple metastases (bone, lung, adrenal glands, and soft tissue) (Fig. 3a). In a patient who had bladder cancer with metastases in lung, pleural lymph nodes, and regional lymph nodes, administration of TAS-115 was discontinued at week 7, and the lung metastatic lesions disappeared after discontinuation of TAS-115 treatment without further antitumor treatment (Fig. 3b). In addition, a notable improvement was observed in the bone scan of a patient with CRPC with multiple bone metastases (Fig. 3c).
Antitumour effect in a a female patient diagnosed with epithelioid sarcoma, b a male patient diagnosed with bladder cancer, and c a male patient diagnosed with prostate cancer. a A female patient in her 20s was initially diagnosed with epithelioid sarcoma. She had received prior treatment for advanced disease with doxorubicin + ifosfamide, carboplatin + etoposide, cisplatin, and pazopanib. At the baseline assessment of this study, she had metastatic disease in bone, lung, adrenal glands, and soft tissue (right-side abdominal). The numbers of hot spots in the bone scan index and fluorodesoxyglucose uptake in the PET-CT scan were reduced at the post-study assessment at Week 6. b A male patient in his 70s was diagnosed with bladder cancer. He had received prior neo-adjuvant treatment with gemcitabine+cisplatin (GC), but had no surgery after GC therapy. At the baseline assessment of this study, he had metastases in pleural lymph nodes, regional lymph nodes, and lung. Administration of TAS-115 650 mg 5-on/2-off was discontinued due to the patient’s withdrawal of consent at Week 7, and lung lesions disappeared after 65 weeks. The patient had only palliative care (no systemic anti-cancer therapy) post-TAS-115 treatment. c A male patient in his 70s was initially diagnosed with prostate cancer. He had received prior treatment with hormone therapy, abiraterone, docetaxel, cabazitaxel, enzalutamide, darolutamide, and docetaxel again. At the baseline assessment of this study, he had metastatic disease in liver, peritoneum, bone, kidney, and pleural effusion. The bone scan index and the number of hot spots of multiple bone metastases were significantly reduced
Pharmacodynamic profile
A significant increase of sMET in plasma was observed on Day 22 in part 1 (P = .0031) and Day 19 (pre-dose and 6 h after TAS-115 administration) in part 2 and the expansion part (P = .0015 and P = .0055, respectively). At 6 h post-dose on Day 19, an increase of VEGF and decrease of VEGFR2 were observed (P = .0844 and P = .0204 respectively), as compared with pre-dose on Day 19 (Supplementary Fig. S2). The relationship between biological changes of the protein levels and antitumor activity was not evaluated due to a limited number of patients with clinical effect.
Discussion
In patients with advanced solid tumors, TAS-115 was generally well tolerated with manageable toxicities. There were no TRAEs that increased dose-dependently in frequency. Although 650 mg SID was determined as the MTD, all patients who received 650 mg SID had treatment interruption due to TRAEs. Thus, a 2-day predefined interruption was included in part 2. Compared with consecutive dosing, the modified dosing schedule led to an improvement in the median relative dose intensity considered to improve recovery from toxicities. Therefore, RP2D was estimated as 650 mg 5-on/2-off for 21 days per cycle.
TAS-115 is similar to cabozantinib in mechanism of action. Cabozantinib inhibits the tyrosine kinase activity of MET, VEGFR and so on, while TAS-115 inhibits FMS and PDGFR in addition to MET and VEGFR. Cabozantinib showed that most common TRAEs (>30% of patients) were diarrhea (57%), fatigue (55%), decreased appetite (48%) and nausea (43%) in phase I study for solid tumours [19]. TAS-115 showed similar TRAEs with cabozantinib, but the frequency of diarrhea in TAS-115 was lower compared to cabozantinib. While, neutropenia, anemia, hypophosphatemia, and thrombocytopenia were not observed in cabozantinib, and these TRAEs are considered TAS-115 specific TRAEs.
PK analyses showed rapid absorption of TAS-115 with a moderate dose-dependent increase in TAS-115 exposure, and no unexpected accumulation was observed in parts 1 and 2. The PK profile showing lack of accumulation and a short half-life may contribute to the tolerability of TAS-115. A dose-dependent increase up to 650 mg in TAS-115 exposure was observed. In preliminary PK analyses of food effect, Cmax and AUC0–24 under fed condition to those under empty stomach condition were 0.545 (0.243–1.224) and 0.812 (0.414–1.593). As there were no statistically significant differences in both parameters, it will be confirmed in further study.
Evaluation of pharmacodynamic markers revealed a significant increase in plasma sMET. Increased levels of circulating sMET were reported in previous clinical studies with cabozantinib, rilotumumab, and onartuzumab [19,20,21]. The elevated plasma sMET in this study may be associated with MET inhibition following TAS-115 administration. Marked alterations of VEGF and sVEGFR2 from Day 1 were not observed, which may be a result of the short half-life of TAS-115. However, comparing pre- and post-dose on Day 19, a VEGFR inhibitory activity of TAS-115 was suggested.
Although there were no patients who showed complete or partial response by RECIST evaluation, TAS-115 exhibited encouraging antitumor effects on the bone metastases, which is in line with preclinical data of TAS-115. In vitro data showed that TAS-115 caused a dose-dependent inhibition of osteoclast differentiation induced by M-CSF and receptor activator of nuclear factor-kappa B ligand (RANKL) (data on file). TAS-115 also suppressed HGF, and VEGF-induced phosphorylation of signaling factors (AKT and ERK1/2) in mouse osteoclasts in vitro [14, 15]. The decline of BSI assessed using BONENAVI® has been reported to be associated with survival in patients with CRPC [22], and this effect on bone metastases may improve the quality of life of patients [23]. The efficacy of TAS-115 on bone was supported by non-clinical findings of inhibition of aberrant bone remodeling and FMS as well as VEGFRs and MET. In the expansion part, we investigated 450 mg/day dosage in CRPC patients with bone metastases in order to improve the administration continuity and dose intensity in elderly patients. Furthermore, a phase II trial for CRPC patients is currently in progress (JapicCTI-163448). Remarkably, a patient who had bladder cancer with lung metastases showed the disappearance of the lung metastatic lesions during palliative care after 58 weeks from discontinuation of TAS-115 treatment (Fig. 3b). We speculated that this tumor shrinkage was caused by inhibition of CSF-1R in macrophages with TAS-115. Inhibition of CSF-1R by TAS-115 may suppress the polarization into M2 macrophages that depends on CSF-1 signaling, which promotes tumor growth, invasion, and metastasis, and thus, the immune environment in tumors may be improved.
In conclusion, TAS-115 was generally well tolerated with manageable toxicities at dose levels of up to and including 650 mg on a 5-on/2-off schedule. From safety and PK profile, RP2D was estimated as 650 mg SID, 5-on/2-off. Pharmacodynamic results demonstrated that TAS-115 acts as a multi-kinase inhibitor. Furthermore, antitumor efficacy, particularly in patients with bone metastases, was encouraging and warrants further investigation. A phase II study was started in patients with castration-resistant prostate cancer with bone metastases.
References
Olsson AK, Dimberg A, Kreuger J, Claesson-Welsh L (2006) VEGF receptor signalling – in control of vascular function. Nat Rev Mol Cell Biol 7:359–371
Ferrara N, Gerber HP, LeCouter J (2003) The biology of VEGF and its receptors. Nat Med 9:669–676
Birchmeier C, Birchmeier W, Gherardi E, Vande Woude GF (2003) Met, metastasis, motility and more. Nat Rev Mol Cell Biol 4:915–925
Shojaei F, Lee JH, Simmons BH, Wong A, Esparza CO, Plumlee PA, Feng J, Stewart AE, Hu-Lowe DD, Christensen JG (2010) HGF/c-met acts as an alternative angiogenic pathway in sunitinib-resistant tumors. Cancer Res 70:10090–10100
Sherr CJ, Roussel MF, Rettenmier CW (1988) Colony-stimulating factor-1 receptor (c-fms). J Cell Biochem 38:179–187
Stanley ER, Chen DM, Lin HS (1978) Induction of macrophage production and proliferation by a purified colony stimulating factor. Nature 274:168–170
Chitu V, Stanley ER (2006) Colony-stimulating factor-1 in immunity and inflammation. Curr Opin Immunol 18:39–48
Wynn TA, Chawla A, Pollard JW (2013) Macrophage biology in development, homeostasis and disease. Nature 496:445–455
Weilbaecher KN, Guise TA, McCauley LK (2011) Cancer to bone: a fatal attraction. Nat Rev Cancer 11:411–425
Roberts WG, Whalen PM, Soderstrom E, Moraski G, Lyssikatos JP, Wang HF, Cooper B, Baker DA, Savage D, Dalvie D, Atherton JA, Ralston S, Szewc R, Kath JC, Lin J, Soderstrom C, Tkalcevic G, Cohen BD, Pollack V, Barth W, Hungerford W, Ung E (2005) Antiangiogenic and antitumor activity of a selective PDGFR tyrosine kinase inhibitor, CP-673,451. Cancer Res 65:957–966
Kalluri R, Zeisberg M (2006) Fibroblasts in cancer. Nat Rev Cancer 6:392–401
Kalluri R (2016) The biology and function of fibroblasts in cancer. Nat Rev Cancer 16:582–598
Fujita H, Miyadera K, Kato M, Fujioka Y, Ochiiwa H, Huang J, Ito K, Aoyagi Y, Takenaka T, Suzuki T, Ito S, Hashimoto A, Suefuji T, Egami K, Kazuno H, Suda Y, Nishio K, Yonekura K (2013) The novel VEGF receptor/MET-targeted kinase inhibitor TAS-115 has marked in vivo antitumor properties and a favorable tolerability profile. Mol Cancer Ther 12:2685–2696
Watanabe K, Hirata M, Tominari T, Matsumoto C, Fujita H, Yonekura K, Murphy G, Nagase H, Miyaura C, Inada M (2016) The MET/vascular endothelial growth factor receptor (VEGFR)-targeted tyrosine kinase inhibitor also attenuates FMS-dependent osteoclast differentiation and bone destruction induced by prostate cancer. J Biol Chem 291:20891–20899
Fujita H, Gomori A, Fujioka Y, Kataoka Y, Tanaka K, Hashimoto A, Suzuki T, Ito K, Haruma T, Yamamoto-Yokoi H, Harada N, Sakuragi M, Oda N, Matsuo K, Inada M, Yonekura K (2016) High potency VEGFRs/MET/FMS triple blockade by TAS-115 concomitantly suppresses tumor progression and bone destruction in tumor-induced bone disease model with lung carcinoma cells. PLoS One 11:e0164830
National Cancer Institute: Cancer Therapy Evaluation Program. Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0, 2009 (v4.03, 2010). https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. Accessed Sept 10 2019
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Brown MS, Chu GH, Kim HJ, Allen-Auerbach M, Poon C, Bridges J, Vidovic A, Ramakrishna B, Ho J, Morris MJ, Larson SM, Scher HI, Goldin JG (2012) Computer-aided quantitative bone scan assessment of prostate cancer treatment response. Nucl Med Commun 33:384–394
Kurzrock R, Sherman SI, Ball DW, Forastiere AA, Cohen RB, Mehra R, Pfister DG, Cohen EEW, Janisch L, Nauling F, Hong DS, Ng CS, Ye L, Gagel RF, Frye J, Müller T, Ratain MJ, Salgia R (2011) Activity of XL184 (Cabozantinib), an oral tyrosine kinase inhibitor, in patients with medullary thyroid cancer. J Clin Oncol 29:2660–2666
Schöffski P, Garcia JA, Stadler WM, Gil T, Jonasch E, Tagawa ST, Smitt M, Yang X, Oliner KS, Anderson A, Zhu M, Kabbinavar F (2011) A phase II study of the efficacy and safety of AMG 102 in patients with metastatic renal cell carcinoma. BJU Int 108:679–686
Koeppen H, Yu W, Zha J, Pandita A, Penuel E, Rangell L, Raja R, Mohan S, Patel R, Desai R, Fu L, Do A, Parab V, Xia X, Januario T, Louie SG, Filvaroff E, Shames DS, Wistuba I, Lipkind M, Huang J, Lazarov M, Ramakrishnan V, Amler L, Phan SC, Patel P, Peterson A, Yauch RL (2014) Biomarker analyses from a placebo-controlled phase II study evaluating erlotinib±onartuzumab in advanced non-small cell lung cancer: MET expression levels are predictive of patient benefit. Clin Cancer Res 20:4488–4498
Armstrong AJ, Anand A, Edenbrandt L, Bondesson E, Bjartell A, Widmark A, Sternberg CN, Pili R, Tuvesson H, Nordle Ö, Carducci MA, Morris MJ (2018) Phase 3 assessment of the automated bone scan index as a prognostic imaging biomarker of overall survival in men with metastatic castration-resistant prostate cancer: a secondary analysis of a randomized clinical trial. JAMA Oncol 4:944–951
Nilsson S, Cislo P, Sartor O, Vogelzang NJ, Coleman RE, O'Sullivan JM, Reuning-Scherer J, Shan M, Zhan L, Parker C (2016) Patient-reported quality-of-life analysis of radium-223 dichloride from the phase III ALSYMPCA study. Ann Oncol 27:868–874
Acknowledgments
We would like to thank all the patients and their families, as well as the investigators and their teams who participated in this study. Editorial support, in the form of medical writing, assembling tables, and creating high-resolution images based on the authors’ detailed directions, collating author comments, copyediting, fact checking, and referencing, was provided by Cactus Communications K.K, CAC Croit Corporation, funded by Taiho Pharmaceutical. Co., Ltd.
Funding
This study was funded by Taiho Pharmaceutical Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T Doi has recieved consultancy from Lily, Kyowa Hakko Kirin, MSD, Daiichi Sankyo, Amgen, Sumitomo Dainippon, Taiho Pharmaceutical, Novartis, Takeda, Chugai Pharma, Abbvie and Bayer; research funding from Lily, Kyowa Hakko Kirin, MSD, Daiichi Sankyo, Sumitomo Dainippon, Taiho Pharmaceutical, Novartis, Merck Serono, Astellas Pharma, Janssen, Boehringer Ingelheim, Pfizer, Chugai Pharma, Celegene, Bristol-Myers Squibb, Abbvie, Quintiles and Eisai.
N Matsubara has recieved honoraria from Janssen, Taiho Pharmaceutical and MSD; paid consultancy from Janssen, Bayer, MSD, Roche and Sanofi; speaker’s bureau from Janssen, MSD, Sanofi and AstraZeneca; research funding from Janssen, MSD, Bayer, Roche and Taiho Pharmaceutical.
S Takahashi has recieved honoraria from Daiichi Sankyo, Sanofi, Eisai, Bayer, Taiho Pharmaceutical, MSD, Novartis, Chugai Pharma, AstraZeneca, Astellas Pharma, Bristol-Myers Squibb, Ono Pharmaceutical, Kyowa Hakko Kirin and Nihonkayaku; research funding from Daiichi Sankyo, Sanofi, Eisai, Bayer, Taiho Pharmaceutical, MSD, Novartis, Chugai Pharma, AstraZeneca, Bristol-Myers Squibb, Lilly and Ono Pharmaceutical; travel, accommodations, expenses from Daiichi Sankyo and Novartis.
N Yamamoto has received honoraria from AstraZeneca, Pfizer, Chugai Pharma, Bristol-Myers Squibb, Ono Pharmaceutical, Lilly; paid consultancy from Eisai, Takeda, Oncothyrapy, Otsuka Pharmaceutical, Boehringer Ingelheim, ASLAN Pharmaceuticals; research funding from Chugai Pharma, Taiho Pharmaceutical, Eisai, Astellas Pharma, Novartis, Daiichi Sankyo, Lilly, Boehringer Ingelheim, Takeda, Kyowa Hakko Kirin, Bayer, Pfizer, Ono Pharmaceutical, Janssen, IQVIA, MSD, Abbvie, Bristol-Myers Squibb, Merck Serono.
The remaining authors have declared no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 370 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Doi, T., Matsubara, N., Kawai, A. et al. Phase I study of TAS-115, a novel oral multi-kinase inhibitor, in patients with advanced solid tumors. Invest New Drugs 38, 1175–1185 (2020). https://doi.org/10.1007/s10637-019-00859-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-019-00859-4