Abstract
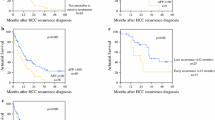
Hepatocellular carcinoma (HCC) as an indication to liver transplant (LT) started as palliative treatment, then moved to potentially curative anti-cancer therapy and more recently entered the era of competition with non-cancer indications, consequent to the need of the society to target equal distribution of the limited resource of donated organs among different indications. Nowadays HCC is a leading indication to LT, currently representing up to 50% of the indications in most transplant Centers. The risk of post-transplant death and the causes of mortality significantly vary along the post-transplant follow-up. Overall, the main causes of death after LT are multiple organ failure and cerebrovascular, cardiovascular, pulmonary, and renal complications. However, after the first post-LT year, mortality for technical complications, infections and general complications significantly decrease, while recurrence of primary liver diseases (particularly malignancies) increase, turning to be the main causes of death. In studies with time-to-event or survival outcomes, a competing risk is an event whose occurrence precludes the occurrence of the primary event of interest. In the setting of LT for HCC, when the primary outcome of interest is death due to HCC recurrence, death due to causes different from this serves as a competing event because subjects who die from such different causes are no longer at risk of death due to HCC recurrence. The introduction of HCC-specific survival as a primary endpoint in studies assessing the outcomes of LT for HCC allows the identification of independent oncologic determinants of post-LT survival and their relative weight on patients’ prognosis. In this view, a continuous model based on level of AFP, tumor size and tumor number that allows to determine the risk of death from HCC-related factors after liver transplantation (www.hcc-olt-metroticket.org/) has been recently developed. Since the endpoint of HCC-specific survival is not influenced by the changes observed in short-term post-LT survival (thanks to advances in the clinical management) nor in long-term post-LT survival (thanks to the introduction of effective treatments achieving control of hepatitis B and C viruses), a model predicting HCC-specific survival will be an helpful prognostic tool in the context of the changing scenarios of LT for HCC.

Similar content being viewed by others
References
Starzl TE, Iwatsuki S, Van Thiel DH, et al. Evolution of liver transplantation. Hepatology. 1982;2:614–636.
Mazzaferro V, Battiston C, Sposito C. Pro (with caution): extended oncologic indications in liver transplantation. Liver Transpl. 2018;24:98–103.
Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2016 annual data report: liver. Am J Transplant. 2018;18(Suppl 1):172–253.
Adam R, Karam V, Delvart V, et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol. 2012;57:675–688.
Iwatsuki S, Gordon RD, Shaw BW Jr, et al. Role of liver transplantation in cancer therapy. Ann Surg. 1985;202:401–407.
Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–699.
Mazzaferro V, Bhoori S, Sposito C, et al. Milan criteria in liver transplantation for hepatocellular carcinoma: an evidence-based analysis of 15 years of experience. Liver Transpl. 2011;17(Suppl 2):S44–S57.
Yao FY, Xiao L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: validation of the UCSF-expanded criteria based on preoperative imaging. Am J Transplant. 2007;7:2587–2596.
Mazzaferro V, Llovet JM, Miceli R, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 2009;10:35–43.
Onaca N, Davis GL, Goldstein RM, et al. Expanded criteria for liver transplantation in patients with hepatocellular carcinoma: a report from the International Registry of Hepatic Tumors in Liver Transplantation. Liver Transpl. 2007;13:391–399.
Toso C, Meeberg G, Hernandez-Alejandro R, et al. Total tumor volume and alpha-fetoprotein for selection of transplant candidates with hepatocellular carcinoma: a prospective validation. Hepatology. 2015;62:158–165.
Duvoux C, Roudot-Thoraval F, Decaens T, et al. Liver transplantation for hepatocellular carcinoma: a model including alpha-fetoprotein improves the performance of Milan criteria. Gastroenterology. 2012;143:986–994.
Halazun KJ, Tabrizian P, Najjar M, et al. Is it time to abandon the milan criteria?: Results of a bicoastal US collaboration to redefine hepatocellular carcinoma liver transplantation selection policies. Ann Surg. 2018;268:690–699.
Bodzin AS, Lunsford KE, Markovic D, et al. Predicting mortality in patients developing recurrent hepatocellular carcinoma after liver transplantation: impact of treatment modality and recurrence characteristics. Ann Surg. 2017;266:118–125.
Gelson W, Hoare M, Dawwas MF, et al. The pattern of late mortality in liver transplant recipients in the United Kingdom. Transplantation. 2011;91:1240–1244.
Rana A, Ackah RL, Webb GJ, et al. No gains in long-term survival after liver transplantation over the past three decades. Ann Surg. 2018;264:239–240.
Aberg F, Gissler M, Karlsen TH, et al. Differences in long-term survival among liver transplant recipients and the general population: a population-based Nordic study. Hepatology. 2015;61:668–677.
Belli LS, Perricone G, Adam R, et al. Impact of DAAs on liver transplantation: major effects on the evolution of indications and results. An ELITA study based on the ELTR registry. J Hepatol. 2018;24:4403–4411.
Austin PC, Fine JP. Accounting for competing risks in randomized controlled trials: a review and recommendations for improvement. Stat Med. 2017;36:1203–1209.
Cox D, Oakes D. Analysis of Survival Data. London: Chapman & Hall; 1984.
Cook TD, DeMets DL, Boca Raton FL. Introduction to Statistical Methods for Clinical Trials. London: Chapman & Hall; 2008.
Lacny S, Wilson T, Clement F, et al. Kaplan–Meier survival analysis overestimates cumulative incidence of health-related events in competing risk settings: a meta-analysis. J Clin Epidemiol. 2018;93:25–35.
Cucchetti A, Serenari M. Efficacy of radiofrequency ablation of hepatocellular carcinoma prior to liver transplantation and the need for competing-risk analysis. Hepatobiliary Surg Nutr. 2018;7:294–296.
Cucchetti A, Cescon M, Bigonzi E, et al. Priority of candidates with hepatocellular carcinoma awaiting liver transplantation can be reduced after successful bridge therapy. Liver Transpl. 2011;17:1344–1354.
Lee MW, Raman SS, Asvadi NH, et al. Radiofrequency ablation of hepatocellular carcinoma as bridge therapy to liver transplantation: a 10-year intention-to-treat analysis. Hepatology. 2017;65:1979–1990.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Cucchetti A, Djulbegovic B, Tsalatsanis A, et al. When to perform hepatic resection for intermediate-stage hepatocellular carcinoma. Hepatology. 2015;61:905–914.
Cucchetti A, Sposito C, Pinna AD, et al. Competing risk analysis on outcome after hepatic resection of hepatocellular carcinoma in cirrhotic patients. World J Gastroenterol. 2017;23:1469–1476.
Mazzaferro V, Sposito C, Zhou J, et al. Metroticket 2.0 model for analysis of competing risks of death after liver transplantation for hepatocellular carcinoma. Gastroenterology. 2018;154:128–139.
Dumortier J, Boillot O, Scoazec JY. Natural history, treatment and prevention of hepatitis C recurrence after liver transplantation: past, present and future. World J Gastroenterol. 2014;20:11069–11079.
Cillo U, Burra P, Mazzaferro V, et al. A multistep, consensus-based approach to organ allocation in liver transplantation: toward a “blended principle model”. Am J Transplant. 2015;15:2552–2561.
Younossi Z, Stepanova M, Ong JP, et al. Nonalcoholic steatohepatitis is the fastest growing cause of hepatocellular carcinoma in liver transplant candidates. Clin Gastroenterol Hepatol. 2018;. https://doi.org/10.1016/j.cgh.2018.05.057.
Sposito C, Cucchetti A, Mazzaferro V. Reply. Gastroenterology. 2018;154:2276–2277.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest, in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sposito, C., Cucchetti, A. & Mazzaferro, V. Assessing Competing Risks for Death Following Liver Transplantation for Hepatocellular Carcinoma. Dig Dis Sci 64, 1001–1007 (2019). https://doi.org/10.1007/s10620-019-05538-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05538-1