Abstract
Background
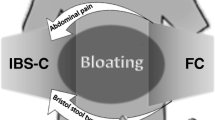
Irritable bowel syndrome (IBS) is a common chronic disorder of the gastrointestinal tract. Several treatments have been developed, including rifaximin for the treatment of IBS without constipation (non-IBS-C), but no studies have evaluated the effect of these therapies on patient referral rates to tertiary care gastroenterology clinics.
Aim
To assess referral patterns for IBS patients at a tertiary motility clinic over a 10-year period.
Methods
Data from consecutive patients referred to the clinic during 2006–2016 were analyzed. Trends in the proportion of referrals and prior rifaximin use in IBS-C versus non-IBS-C groups were compared.
Results
A total of 814 adult patients were referred to a single physician panel for IBS-related symptoms. Of these, 776 were included in the study [528 females (68%), average age 45.7 ± 15.9 years), comprising 431 IBS-C (55.5%) and 345 non-IBS-C (44.5%) patients. The proportion of non-IBS-C referrals declined significantly from 53.0% in 2006 to 27.3% in 2016 (Chi-square, p < 0.0001, Cochran–Armitage trend test p = 0.0001), and the proportion of IBS-C referrals increased significantly from 46.9% in 2006 to 72.7% in 2016 (Chi-square, p < 0.0001, Cochran–Armitage trend test p = 0.0004). Non-IBS-C referrals with prior rifaximin use significantly increased from 22.7% in 2006 to 66.7% in 2016 (Cochran–Armitage trend test, p = 0.008).
Conclusions
The results indicate a significantly declining tertiary care referral rate for non-IBS-C over the past decade. While not directly linked, there has been an increase in rifaximin use in the same population during the same time interval.


Similar content being viewed by others
References
Ford AC, Lacy BE, Talley NJ. Irritable bowel syndrome. N Engl J Med. 2017;376:2566–2578.
Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150:1393-1407.e1395.
Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712-721.e714.
Buono JL, Mathur K, Averitt AJ, Andrae DA. Economic burden of inadequate symptom control among US commercially insured patients with irritable bowel syndrome with diarrhea. J Med Econ. 2017;20:353–362.
Simrén M, Abrahamsson H, Svedlund J, Björnsson E. Quality of life in patients with irritable bowel syndrome seen in referral centers versus primary care: the impact of gender and predominant bowel pattern. Scand J Gastroenterol. 2001;36:545–552.
Porsch U, Wanitschke R, Linhart P, et al. A consecutive study of patients with irritable bowel syndrome disease in two tertiary referral centers. Psychother Psych Med. 2001;51:267–275.
Pimentel M. Evidence-based management of irritable bowel syndrome with diarrhea. Am J Managed Care. 2018;24:S35–S46.
Hulisz D. The burden of illness of irritable bowel syndrome: current challenges and hope for the future. J Managed Care Pharm. 2004;10:299–309.
Chey WD, Chey WY, Heath AT, et al. Long-term safety and efficacy of alosetron in women with severe diarrhea-predominant irritable bowel syndrome. Am J Gastroenterol. 2004;99:2195.
FDA Drug Safety Communication. FDA warns about increased risk of serious pancreatitis with irritable bowel drug Viberzi (eluxadoline) in patients without a gallbladder. Silver Spring: Food and Drug Administration; 2017.
Pimentel M, Lembo A, Chey WD, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22–32.
Lembo A, Pimentel M, Rao SS, et al. Repeat treatment with rifaximin is safe and effective in patients with diarrhea-predominant irritable bowel syndrome. Gastroenterology. 2016;151:1113–1121.
Menees SB, Maneerattannaporn M, Kim HM, Chey WD. The efficacy and safety of rifaximin for the irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2011;107:28.
Shah E, Pimentel M. Evaluating the functional net value of pharmacologic agents in treating irritable bowel syndrome. Aliment Pharmacol Therapeut. 2014;39:973–983.
Armitage P. Tests for linear trends in proportions and frequencies. Biometrics. 1955;11:375–386.
Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71–80.
Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712-721 e714.
Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015;313:949–958.
Chandar AK. Diagnosis and treatment of irritable bowel syndrome with predominant constipation in the primary-care setting: focus on linaclotide. Int J Gen Med. 2017;10:385–393.
Engsbro AL, Begtrup LM, Kjeldsen J, et al. Patients suspected of irritable bowel syndrome—cross-sectional study exploring the sensitivity of Rome III criteria in primary care. Am J Gastroenterol. 2013;108:972.
Sommers T, Corban C, Sengupta N, et al. Emergency department burden of constipation in the United States from 2006 to 2011. Am J Gastroenterol. 2015;110:572.
Kumar L, Barker C, Emmanuel A. Opioid-induced constipation: pathophysiology, clinical consequences, and management. Gastroenterol Res Pract. 2014;2014:141737.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Cedars-Sinai has licensing agreements with Salix Pharmaceuticals, Naia Pharmaceuticals, Gemelli Biotech, Inc., and Synthetic Biologics Inc. Mark Pimentel is a consultant for Salix Pharmaceuticals, Naia Pharmaceuticals, Synthetic Biologics Inc., Shire, and US Medical, is a board member of Gemelli Biotech and has received research funding from Salix Pharmaceuticals and Synthetic Biologics Inc. Ruchi Mathur is a board member of Gemelli Biotech and has received research funding from Valeant Pharmaceuticals and the American Diabetes Association. Ali Rezaie has received speaker and consultant fees from Commonwealth Laboratories, Actavis, and Salix Pharmaceuticals, and has received research funding from Valeant Pharmaceuticals, the American College of Gastroenterology, and the Kenneth Rainin Foundation. The remaining authors have no conflicts to disclose.
Rights and permissions
About this article
Cite this article
Oh, S.J., Tashjian, V.C., Mirocha, J. et al. Declining Rates of Referral for Irritable Bowel Syndrome Without Constipation at a Tertiary Care Center. Dig Dis Sci 64, 182–188 (2019). https://doi.org/10.1007/s10620-018-5302-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5302-2