Abstract
Background and Aims
Compared with ulcer bleeding (UB) in non-variceal upper gastrointestinal bleeding (NVUGIB), non-ulcer bleeding (NUB) is often considered to have a low risk of poor outcomes and is treated less intensively without any risk stratification. We conducted this study to assess the predictability of scoring systems for NUB and compare the outcomes of NUB and UB.
Methods
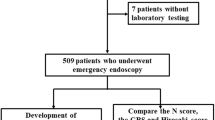
A total of 1831 UGIB patients were registered in the database during the period from February 2011 to December 2013. Among them, 1424 patients with NVUGIB were divided into two groups: Group UB (1101 patients with peptic ulcer bleeding) and Group NUB (323 patients with non-peptic ulcer-related bleeding).
Results
The most common cause of bleeding in Group NUB was Mallory–Weiss tears (51.1%), followed by Dieulafoy lesions (18.9%). A receiver operating characteristic (ROC) analysis revealed that the pre-Rockall score [area under the ROC (AUROC) = 0.798; 95% CI 0.707–0.890] and full Rockall score (AUROC = 0.794; 95% CI 0.693–0.895) were relatively good at predicting overall mortality in NUB. Glasgow–Blatchford score (AUROC = 0.783; 95% CI 0.730–0.836) was the most closely correlated with the need for clinical intervention in NUB. Those who had Glasgow–Blatchford score of 0 did not require any interventions, including blood transfusions. There were no statistical differences in overall mortality (p = 0.387), bleeding-related mortality (p = 0.447), or the incidence of re-bleeding (p = 0.117) between the two groups.
Conclusions
Scoring systems are useful to predict mortality and the need for clinical intervention in patients with NUB.




Similar content being viewed by others
References
Rotondano G, Cipolletta L, Koch M, et al. Predictors of favourable outcome in non-variceal upper gastrointestinal bleeding: implications for early discharge? Dig Liver Dis. 2014;46:231–236.
Barkun AN, Martel M, Toubouti Y, Rahme E, Bardou M. Endoscopic hemostasis in peptic ulcer bleeding for patients with high-risk lesions: a series of meta-analyses. Gastrointest Endosc. 2009;69:786–799.
Church NI, Dallal HJ, Masson J, et al. Validity of the Rockall scoring system after endoscopic therapy for bleeding peptic ulcer: a prospective cohort study. Gastrointest Endosc. 2006;63:606–612.
Church NI, Palmer KR. Relevance of the Rockall score in patients undergoing endoscopic therapy for peptic ulcer haemorrhage. Eur J Gastroenterol Hepatol. 2001;13:1149–1152.
Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996;38:316–321.
Blatchford O, Murray WR, Blatchford M. A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet. 2000;356:1318–1321.
Vreeburg EM, Terwee CB, Snel P, et al. Validation of the Rockall risk scoring system in upper gastrointestinal bleeding. Gut. 1999;44:331–335.
Marmo R, Del Piano M, Rotondano G, et al. Mortality from nonulcer bleeding is similar to that of ulcer bleeding in high-risk patients with nonvariceal hemorrhage: a prospective database study in Italy. Gastrointest Endosc. 2012;75:263–272, 72 e1
Yin J, Tian L. Joint confidence region estimation for area under ROC curve and Youden index. Stat Med. 2014;33:985–1000.
Greenspoon J, Barkun A, Bardou M, et al. Management of patients with nonvariceal upper gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2012;10:234–239.
Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152:101–113.
Boyapati R, Ong SY, Ye B, et al. One fifth of hospitalizations for peptic ulcer-related bleeding are potentially preventable. World J Gastroenterol. 2014;20:10504–10511.
Laine L, Jensen DM. Management of patients with ulcer bleeding. The American journal of gastroenterology. 2012;107:345–360; quiz 61.
Laursen SB, Hansen JM, Schaffalitzky de Muckadell OB. The Glasgow Blatchford score is the most accurate assessment of patients with upper gastrointestinal hemorrhage. Clin Gastroenterol Hepatol. 2012;10:1130–1135 e1.
Bryant RV, Kuo P, Williamson K, et al. Performance of the Glasgow-Blatchford score in predicting clinical outcomes and intervention in hospitalized patients with upper GI bleeding. Gastrointest Endosc. 2013;78:576–583.
Dicu D, Pop F, Ionescu D, Dicu T. Comparison of risk scoring systems in predicting clinical outcome at upper gastrointestinal bleeding patients in an emergency unit. Am J Emerg Med. 2013;31:94–99.
Enns RA, Gagnon YM, Barkun AN, Armstrong D, Gregor JC, Fedorak RN. Validation of the Rockall scoring system for outcomes from non-variceal upper gastrointestinal bleeding in a Canadian setting. World J Gastroenterol. 2006;12:7779–7785.
Lim LG, Ho KY, Chan YH, et al. Urgent endoscopy is associated with lower mortality in high-risk but not low-risk nonvariceal upper gastrointestinal bleeding. Endoscopy. 2011;43:300–306.
Gralnek IM, Dulai GS. Incremental value of upper endoscopy for triage of patients with acute non-variceal upper-GI hemorrhage. Gastrointest Endosc. 2004;60:9–14.
Masaoka T, Suzuki H, Hori S, Aikawa N, Hibi T. Blatchford scoring system is a useful scoring system for detecting patients with upper gastrointestinal bleeding who do not need endoscopic intervention. J Gastroenterol Hepatol. 2007;22:1404–1408.
Dulai GS, Gralnek IM, Oei TT, et al. Utilization of health care resources for low-risk patients with acute, nonvariceal upper GI hemorrhage: an historical cohort study. Gastrointest Endosc. 2002;55:321–327.
Rockall TA, Logan RF, Devlin HB, Northfield TC. Selection of patients for early discharge or outpatient care after acute upper gastrointestinal haemorrhage. National Audit of Acute Upper Gastrointestinal Haemorrhage. Lancet. 1996;347:1138–1140.
Stanley AJ, Ashley D, Dalton HR, et al. Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage: multicentre validation and prospective evaluation. Lancet. 2009;373:42–47.
Chen IC, Hung MS, Chiu TF, Chen JC, Hsiao CT. Risk scoring systems to predict need for clinical intervention for patients with nonvariceal upper gastrointestinal tract bleeding. Am J Emerg Med. 2007;25:774–779.
Stanley AJ. Update on risk scoring systems for patients with upper gastrointestinal haemorrhage. World J Gastroenterol. 2012;18:2739–2744.
Hearnshaw SA, Logan RF, Lowe D, Travis SP, Murphy MF, Palmer KR. Acute upper gastrointestinal bleeding in the UK: patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut. 2011;60:1327–1335.
Lee SY. Current progress toward eradicating Helicobacter pylori in East Asian countries: differences in the 2013 revised guidelines between China, Japan, and South Korea. World J Gastroenterol. 2014;20:1493–1502.
Acknowledgment
We appreciate Daegu-Gyeongbuk Gastrointestinal Study Group (DGSG) members for data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There are no financial or other conflicts of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Park, H.W., Jeon, S.W. Clinical Outcomes of Patients with Non-ulcer and Non-variceal Upper Gastrointestinal Bleeding: A Prospective Multicenter Study of Risk Prediction Using a Scoring System. Dig Dis Sci 63, 3253–3261 (2018). https://doi.org/10.1007/s10620-018-5255-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5255-5