Abstract
Background and Study Aim
Although propofol is widely used for sedation for endoscopic procedures, concerns remain regarding cardiopulmonary adverse events. Etomidate has little effect on the cardiovascular and respiratory systems, but patient satisfaction analysis is lacking. We compared the efficacy and safety of balanced propofol and etomidate sedation during advanced endoscopic procedures.
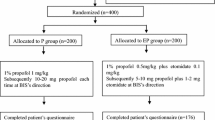
Methods
As a randomized noninferiority trial, balanced endoscopic sedation was achieved using midazolam and fentanyl, and patients were randomly assigned to receive propofol (BPS) or etomidate (BES) as add-on drug. The main outcomes were sedation efficacy measured on a 10-point visual analog scale (VAS) and safety.
Results
In total, 186 patients (94 in the BPS group and 92 in the BES group) were evaluated. BES did not show noninferiority in terms of overall patient satisfaction, with a difference in VAS score of −0.35 (97.5 % confidence interval −1.03 to ∞, p = 0.03). Among endoscopists and nurses, BES showed noninferiority to BPS, with differences in VAS scores of 0.06 and 0.08, respectively. Incidence of cardiopulmonary adverse events was lower in the BES group (27.7 versus 14.1 %, p = 0.023). Hypoxia occurred in 5.3 and 1.1 % of patients in the BPS and BES group (p = 0.211). Myoclonus occurred in 12.1 % (11/92) in the BES group. BES had lower risk of overall cardiopulmonary adverse events (odds ratio 0.401, p = 0.018).
Conclusions
BES was not noninferior to BPS in terms of patient satisfaction. However, BES showed better safety outcomes in terms of cardiopulmonary adverse events.



Similar content being viewed by others
References
Gouda B, Gouda G, Borle A, et al. Safety of non-anesthesia provider administered propofol sedation in non-advanced gastrointestinal endoscopic procedures: a meta-analysis. Saudi J Gastroenterol. 2017;23:133–143.
Burtea DE, Dimitriu A, Malos AE, et al. Current role of non-anesthesiologist administered propofol sedation in advanced interventional endoscopy. World J Gastrointest Endosc. 2015;7:981–986.
Yusoff IF, Raymond G, Sahai AV. Endoscopist administered propofol for upper-GI EUS is safe and effective: a prospective study in 500 patients. Gastrointest Endosc. 2004;60:356–360.
Dumonceau JM, Riphaus A, Schreiber F, et al. Non-anesthesiologist administration of propofol for gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates Guideline. Endoscopy. 2015;47:1175–1189.
Lee CK, Lee SH, Chung IK, et al. Balanced propofol sedation for therapeutic GI endoscopic procedures: a prospective, randomized study. Gastrointest Endosc. 2011;73:206–214.
Lee SJ, Lee TH, Park SH, et al. Efficacy of carbon dioxide versus air insufflation according to different sedation protocols during therapeutic endoscopic retrograde cholangiopancreatography: prospective, randomized, double-blind study. Dig Endosc. 2015;27:512–521.
Lee TH, Lee CK, Park SH, et al. Balanced propofol sedation versus propofol monosedation in therapeutic pancreaticobiliary endoscopic procedures. Dig Dis Sci. 2012;57:2113–2121. https://doi.org/10.1007/s10620-012-2234-0.
Cote GA, Hovis RM, Ansstas MA, et al. Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol. 2010;8:137–142.
Triantafillidis JK, Merikas E, Nikolakis D, et al. Sedation in gastrointestinal endoscopy: current issues. World J Gastroenterol. 2013;19:463–481.
Forman SA. Clinical and molecular pharmacology of etomidate. Anesthesiology. 2011;114:695–707.
Falk J, Zed PJ. Etomidate for procedural sedation in the emergency department. Ann Pharmacother. 2004;38:1272–1277.
Zhou X, Li BX, Chen LM, et al. Etomidate plus propofol versus propofol alone for sedation during gastroscopy: a randomized prospective clinical trial. Surg Endosc. 2016;30:5108–5116.
Kim MG, Park SW, Kim JH, et al. Etomidate versus propofol sedation for complex upper endoscopic procedures: a prospective double-blinded randomized controlled trial. Gastrointest Endosc. 2017;86:452–461.
Park CH, Park SW, Hyun B, et al. Efficacy and safety of etomidate-based sedation compared with propofol-based sedation during ERCP in low-risk patients: a double-blind, randomized, noninferiority trial. Gastrointest Endosc. 2018;87:174–184.
American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists, Gross JB, Bailey PL, Connis RT et al. Practice guidelines for sedation and analgesia by non-anesthesiologists (An updated report by the American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists). Anesthesiology. 2002;96:1004–1017.
Lovett P, Gomez V, Hodge DO, et al. Propofol versus midazolam/fentanyl sedation for colonoscopy in the elderly patient population. J Perianesth Nurs. 2017;32:210–214.
Han SJ, Lee TH, Park SH, et al. Efficacy of midazolam- versus propofol-based sedations by non-anesthesiologists during therapeutic endoscopic retrograde cholangiopancreatography in patients aged over 80 years. Dig Endosc. 2017;29:369–376.
Khan MA, Akbar A, Baron TH, et al. Endoscopic ultrasound-guided biliary drainage: a systematic review and meta-analysis. Dig Dis Sci. 2016;61:684–703. https://doi.org/10.1007/s10620-015-3933-0.
Yates AM, Wolfson AB, Shum L, et al. A descriptive study of myoclonus associated with etomidate procedural sedation in the ED. Am J Emerg Med. 2013;31:852–854.
Huter L, Schreiber T, Gugel M, et al. Low-dose intravenous midazolam reduces etomidate-induced myoclonus: a prospective, randomized study in patients undergoing elective cardioversion. Anesth Analg. 2007;105:1298–1302.
Meng QT, Cao C, Liu HM, et al. Safety and efficacy of etomidate and propofol anesthesia in elderly patients undergoing gastroscopy: a double-blind randomized clinical study. Exp Ther Med. 2016;12:1515–1524.
Liu J, Liu R, Meng C, et al. Propofol decreases etomidate-related myoclonus in gastroscopy. Medicine. 2017;96:7212.
Wang J, Li QB, Wu YY, et al. Efficacy and safety of opioids for the prevention of etomidate-induced myoclonus: a meta-analysis. Am J Ther. 2016;. https://doi.org/10.1097/mjt.0000000000000404.
van Oss GE, Rachmat Y, Booij LH, et al. Continuous infusion of etomidate as a method for outpatient anesthesia. Acta Anaesthesiol Belg. 1980;31:39–43.
St Pierre M, Dunkel M, Rutherford A, et al. Does etomidate increase postoperative nausea? A double-blind controlled comparison of etomidate in lipid emulsion with propofol for balanced anaesthesia. Eur J Anaesthesiol. 2000;17:634–641.
Ye L, Xiao X, Zhu L. The comparison of etomidate and propofol anesthesia in patients undergoing gastrointestinal endoscopy: a systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech. 2017;27:1–7.
Yeung JK, Zed PJ. A review of etomidate for rapid sequence intubation in the emergency department. Can J Emerg Med. 2002;4:194–198.
Morel J, Salard M, Castelain C, et al. Haemodynamic consequences of etomidate administration in elective cardiac surgery: a randomized double-blinded study. Br J Anaesthesiol. 2011;107:503–509.
Moller Petrun A, Kamenik M. Bispectral index-guided induction of general anaesthesia in patients undergoing major abdominal surgery using propofol or etomidate: a double-blind, randomized, clinical trial. Br J Anaesthesiol. 2013;110:388–396.
Toklu S, Iyilikci L, Gonen C, et al. Comparison of etomidate–remifentanil and propofol–remifentanil sedation in patients scheduled for colonoscopy. Eur J Anaesthesiol. 2009;26:370–376.
Baradari AG, Alipour A, Habibi MR, et al. A randomized clinical trial comparing hemodynamic responses to ketamine-propofol combination (ketofol) versus etomidate during anesthesia induction in patients with left ventricular dysfunction undergoing coronary artery bypass graft surgery. Arch Med Sci. 2017;13:1102–1110.
Acknowledgments
This work was supported by the Soonchunhyang University Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Han, S.J., Lee, T.H., Yang, J.K. et al. Etomidate Sedation for Advanced Endoscopic Procedures. Dig Dis Sci 64, 144–151 (2019). https://doi.org/10.1007/s10620-018-5220-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5220-3