Abstract
Background
There are a limited number of studies investigating the type of serum proteins capable of differentiating intraductal papillary mucinous neoplasms from benign or malignant diseases of the pancreas.
Aims
To select proteins able to differentiate intraductal papillary mucinous neoplasms from benign and malignant pancreatic disease using semiquantitative proteomics.
Methods
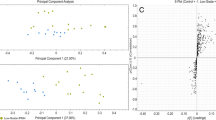
Serum samples were obtained from 74 patients (19 with type II intraductal papillary mucinous neoplasms, 8 with type I/III intraductal papillary mucinous neoplasms, 24 with chronic pancreatitis, 23 with pancreatic ductal adenocarcinomas) and 21 healthy subjects. Small proteins and peptides were assayed by matrix-assisted laser desorption/ionization for the detection of differentially abundant species possibly related to tumor onset. Serum pancreatic amylase, lipase, carcinoembryonic antigen and carbohydrate antigen 19-9 (CA 19-9) were also assayed.
Results
Twenty-six of 84 peaks detected were dysregulated (7 more abundant and 19 less abundant in the type II intraductal papillary mucinous neoplasms, p < 0.05). Of the differentially abundant peaks, 17 were commonly dysregulated (3 peaks more abundant and 13 less abundant in type II intraductal papillary mucinous neoplasms, and one at m/z = 9961 at variance), indicating a protein fingerprint shared by types I/III and type II intraductal papillary mucinous neoplasms and pancreatic ductal adenocarcinomas.
Conclusions
These results suggest that our approach can be used to differentiate type II intraductal papillary mucinous neoplasms from type I/III neoplasms, and type II intraductal papillary mucinous neoplasms from pancreatic ductal adenocarcinomas.





Similar content being viewed by others
References
Buscarini E, Pezzilli R, Cannizzaro R, et al. Italian consensus guidelines for the diagnostic work-up and follow-up of cystic pancreatic neoplasms. Dig Liver Dis. 2014;46:479–493.
Falconi M, Crippa S, Chari S, et al. Quality assessment of the guidelines on cystic neoplasms of the pancreas. Pancreatology. 2015;15:463–469.
Capurso G, Boccia S, Salvia R, et al. Risk factors for intraductal papillary mucinous neoplasm (IPMN) of the pancreas: a multicentre case–control study. Am J Gastroenterol. 2013;108:1003–1009.
Pezzilli R, Melzi dʼEril G, Barassi A. Can serum pancreatic amylase and lipase levels be used as diagnostic markers to distinguish between patients with mucinous cystic lesions of the pancreas, chronic pancreatitis, and pancreatic ductal adenocarcinoma? Pancreas. 2016;45:1272–1275.
Pezzilli R, Calculli L, Melzi d’Eril G, et al. Serum tumor markers not useful in screening patients with pancreatic mucinous cystic lesions associated with malignant changes. Hepatobiliary Pancreat Dis Int.. 2016;15:553–557.
Rebours V, Le Faouder J, Laouirem S, et al. In situ proteomic analysis by MALDI imaging identifies ubiquitin and thymosin-β4 as markers of malignant intraductal pancreatic mucinous neoplasms. Pancreatology. 2014;14:117–124.
Corcos O, Couvelard A, Dargère D, et al. Proteomic assessment of markers for malignancy in the mucus of intraductal papillary mucinous neoplasms of the pancreas. Pancreas. 2012;41:169–174.
Tanaka M, Fernández-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–197.
Fania C, Vasso M, Torretta E, et al. Setup for human sera MALDI profiling: the case of rhEPO treatment. Electrophoresis. 2011;32:1715–1727.
Dudeja GV, Allen PJ. Premalignant cystic neoplasms of the pancreas. Semin Oncol. 2015;42:70–85.
Ohtsuka T, Matsunaga T, Kimura H, et al. Role of pancreatic juice cytology in the preoperative management of intraductal papillary mucinous neoplasm of the pancreas in the era of international consensus guidelines 2012. World J Surg. 2014;38:2994–3001.
Tamura K, Ohtsuka T, Ideno N, et al. Treatment strategy for main duct intraductal papillary mucinous neoplasms of the pancreas based on the assessment of recurrence in the remnant pancreas after resection: a retrospective review. Ann Surg. 2014;259:360–368.
Pezzilli R, Corsi MM, Barassi A, et al. The role of inflammation in patients with intraductal mucinous neoplasm of the pancreas and in those with pancreatic adenocarcinoma. Anticancer Res. 2010;30:3801–3805.
Salvia R, Malleo G, Marchegiani G, et al. Pancreatic resections for cystic neoplasms: from the surgeon’s presumption to the pathologist’s reality. Surgery. 2012;152:S135–S142.
Crippa S, Pezzilli R, Bissolati M, et al. Active surveillance beyond 5 years is required for presumed branch-duct intraductal papillary mucinous neoplasms undergoing non-operative management. Am. J. Gastroenterol. 2017. (in press).
Pezzilli R, Fabbri D, Corsi MM, et al. Plasma concentrations of angiogenetic factors and angiogenetic inhibitors in patients with ductal pancreatic neoplasms. A pilot study. Clin Chem Lab Med. 2011;49:1047–1051.
Velstra B, Vonk MA, Bonsing BA, et al. Serum peptide signatures for pancreatic cancer based on mass spectrometry: a comparison to CA19-9 levels and routine imaging techniques. J Cancer Res Clin Oncol. 2015;141:531–541.
Xue A, Scarlett CJ, Chung L, et al. Discovery of serum biomarkers for pancreatic adenocarcinoma using proteomic analysis. Br J Cancer. 2010;103:391–400.
Potjer TP, Mertens BJ, Nicolardi S, et al. Application of a serum protein signature for pancreatic cancer to separate cases from controls in a pancreatic surveillance cohort. Transl Oncol.. 2016;9:242–247.
Cecconi D, Palmieri M, Donadelli M. Proteomics in pancreatic cancer research. Proteomics. 2011;11:816–828.
Liu Z, Ma Y, Yang J, et al. Upregulated and downregulated proteins in hepatocellular carcinoma: a systematic review of proteomic profiling studies. OMICS. 2011;15:61–71.
Zapico-Muñiz E, Farré-Viladrich A, Rico-Santana N, et al. Standardized peptidome profiling of human serum for the detection of pancreatic cancer. Pancreas. 2010;39:1293–1298.
Gerdtsson AS, Malats N, Säll A, et al. A multicenter trial defining a serum protein signature associated with pancreatic ductal adenocarcinoma. Int J Proteom. 2015;2015:587250.
Yoneyama T, Ohtsuki S, Honda K, et al. Identification of IGFBP2 and IGFBP3 as compensatory biomarkers for CA19-9 in early-stage pancreatic cancer using a combination of antibody-based and LC-MS/MS-based proteomics. PLoS ONE. 2016;11:e0161009.
Kikkawa S, Sogawa K, Satoh M, et al. Identification of a novel biomarker for biliary tract cancer using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Int J Proteomics.. 2012;2012:108609.
Hart PA, Topazian M, Raimondo M, et al. Endoscopic pancreas fluid collection: methods and relevance for clinical care and translational science. Am J Gastroenterol. 2016;111:1258–1266.
Hortin GL, Sviridov D, Anderson NL. High-abundance polypeptides of the human plasma proteome comprising the top 4 logs of polypeptide abundance. Clin Chem. 2008;54:1608–1616.
Fania C, Sogno I, Vasso M, et al. A PSA-guided approach for a better diagnosis of prostatic adenocarcinoma based on MALDI profiling and peptide identification. Clin Chim Acta. 2015;439:42–49.
Acknowledgments
The authors wish to thank Enrica Torretta of the Department of Biomedical Sciences for Health, University of Milan, Milan, Italy, for the revision of statistical analyses.
Funding
This work was funded by the Italian Ministry of University and Scientific Research (Grant No. FIRB RBRNO78MCT to C. Gelfi).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fania, C., Pezzilli, R., Melzi d’Eril, G. et al. Identification of Small Proteins and Peptides in the Differentiation of Patients with Intraductal Mucinous Neoplasms of the Pancreas, Chronic Pancreatitis and Pancreatic Adenocarcinoma. Dig Dis Sci 63, 920–933 (2018). https://doi.org/10.1007/s10620-018-4944-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-4944-4