Abstract
Background and Aims
The relationship between insulin resistance and post-ERCP pancreatitis (PEP) is not known. We aimed to determine the relation between pre-ERCP insulin resistance and risk of PEP, and to evaluate the relationship of insulin resistance with well-established risk factors for PEP.
Methods
Consecutive patients who underwent ERCP with the diagnosis of choledocolithiasis between January and December 2013 were enrolled in this prospective study. Pre-procedural insulin resistance state and other risk factors were evaluated according to PEP development.
Results
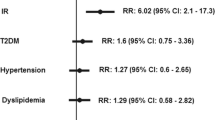
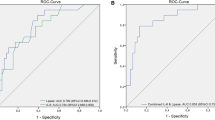
Pancreatitis developed in 16 (11.3 %) of 141 ERCP procedure. Homeostasis model assessment of insulin resistance (HOMA-IR) levels was found statistically significantly higher in patients who developed PEP than the ones who did not (3.37 ± 0.8 vs. 2.38 ± 1.4, p < 0.001). Common bile duct (CBD) diameter of the patients developing PEP was found significantly lower than the non-PEP group (10.1 ± 4 vs. 13.4 ± 4.5 mm, p = 0.01). Mean procedure time was 33.5 min in PEP group and 27.9 min in non-PEP group (p = 0.006). HOMA-IR (OR 2.39), procedure time (OR 1.15), and CBD diameter (OR 0.82) were independent predictors of PEP development.
Conclusions
The presence of insulin resistance is an important risk factor for PEP, and these data can be used as a considerable clue to predict the risk of PEP before ERCP and to decrease related morbidity.

Similar content being viewed by others

References
Freeman ML. Post-ERCP pancreatitis: patient and technique-related risk factors. JOP J Pancreas. 2002;3:169–176.
Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1–10.
Dickinson RJ, Davies S. Post-ERCP pancreatitis and hyperamylasaemia: the role of operative and patient factors. Eur J Gastroenterol Hepatol. 1998;10:423–428.
Wang P, Li Z-S, Liu F, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009;104:31–40.
Cotton PB, Garrow DA, Gallagher J, et al. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80–88.
Masci E, Toti G, Mariani A, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417–423.
Christoforidis E, Goulimaris I, Kanellos I, et al. Post-ERCP pancreatitis and hyperamylasemia: patient-related and operative risk factors. Endoscopy. 2002;34:286–292.
Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111.
Thaker AM, Mosko JD, Berzin TM. Post-endoscopic retrograde cholangiopancreatography pancreatitis. Gastroenterol Rep. 2015;3:32–40.
Chen J-J, Wang X-M, Liu X-Q, et al. Risk factors for post-ERCP pancreatitis: a systematic review of clinical trials with a large sample size in the past 10 years. Eur J Med Res. 2014;19:26.
Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425–434.
Badalov N, Tenner S, Baillie J. The Prevention, recognition and treatment of post-ERCP pancreatitis. JOP J Pancreas. 2009;10:88–97.
Sahakian AB, Buxbaum JL, Van Dam J. Prevention and management of Post-ERCP Pancreatitis. JOP J Pancreas. 2014;15:544–551.
Testoni PA. Unresolved issues about post-ERCP pancreatitis: an overview. JOP J Pancreas. 2002;3:156–161.
Pezzilli R, Romboli E, Campana D, Corinaldesi R. Mechanisms involved in the onset of post-ERCP pancreatitis. JOP J Pancreas. 2002;3:162–168.
Ito K, Fujita N, Noda Y, et al. Relationship between post-ERCP pancreatitis and the change of serum amylase level after the procedure. World J Gastroenterol. 2007;13:3855–3860.
Messmann H, Vogt W, Holstege A, et al. Post-ERP pancreatitis as a model for cytokine induced acute phase response in acute pancreatitis. Gut. 1997;40:80–85.
Leung PS, Chan YC. Role of oxidative stress in pancreatic inflammation. Antioxid Redox Signal. 2009;11:135–165.
Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–1428.
Asrih M, Jornayvaz FR. Inflammation as a potential link between nonalcoholic fatty liver disease and insulin resistance. J Endocrinol. 2013;218:R25–R36.
Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; american heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120:1640–1645.
Aroor AR, McKarns S, Demarco VG, et al. Maladaptive immune and inflammatory pathways lead to cardiovascular insulin resistance. Metabolism. 2013;62:1543–1552.
Stefan N, Kantartzis K, Machann J, et al. Identification and characterization of metabolically benign obesity in humans. Arch Intern Med. 2008;168:1609–1616.
Apovian CM, Bigornia S, Mott M, et al. Adipose macrophage infiltration is associated with insulin resistance and vascular endothelial dysfunction in obese subjects. Arterioscler Thromb Vasc Biol. 2008;28:1654–1659.
Ozkul A, Ayhan M, Akyol A, et al. The effect of insulin resistance on inflammatory response and oxidative stress in acute cerebral ischemia. Neuro Endocrinol Lett. 2013;34:52–57.
Caccamo G, Bonura F, Bonura F, et al. Insulin resistance and acute coronary syndrome. Atherosclerosis. 2010;211:672–675.
Frossard J-L, Lescuyer P, Pastor CM. Experimental evidence of obesity as a risk factor for severe acute pancreatitis. World J Gastroenterol. 2009;15:5260–5265.
Deenadayalu VP, Blaut U, Watkins JL, et al. Does obesity confer an increased risk and/or more severe course of post-ERCP pancreatitis? A retrospective, multicenter study. J Clin Gastroenterol. 2008;42:1103–1109.
Pokhrel B, Choi EK, Khalid O, et al. Increased fat in pancreas not associated with risk of pancreatitis post-endoscopic retrograde cholangiopancreatography. Clin Exp Gastroenterol. 2014;7:199–204.
Iorgulescu A, Sandu I, Turcu F, Iordache N. Post-ERCP acute pancreatitis and its risk factors. J Med Life. 2013;6:109–113.
Testoni PA, Mariani A, Giussani A, et al. Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterol. 2010;105:1753–1761.
Katsinelos P, Lazaraki G, Chatzimavroudis G, et al. Risk factors for therapeutic ERCP-related complications: an analysis of 2,715 cases performed by a single endoscopist. Ann Gastroenterol Q Publ Hell Soc Gastroenterol. 2014;27:65–72.
Testoni PA. Why the incidence of post-ERCP pancreatitis varies considerably? Factors affecting the diagnosis and the incidence of this complication. J Pancreas. 2002;3:195–201.
Hernández Garcés HR, Almeida Linnet A, Abreu Vázquez MDR, et al. Risk factors associated with the development of hyperamylasemia and post-ERCP pancreatitis in the Cuban National Institute. Rev Gastroenterol Perú Órgano Soc Gastroenterol Perú. 2014;34:127–132.
Leghari A, Ghazanfar S, Qureshi S, et al. Frequency and risk factors in the post-ERCP pancreatitis in a tertiary care centre. J Coll Phys Surg Pak. 2013;23:620–624.
Jacobson BC, Carr-Locke DL. Hypotension during ERCP is common but not a risk factor for post-ERCP pancreatitis. HPB. 2001;3:169–173.
Beyazit Y, Sayilir A, Torun S, et al. Mean platelet volume as an indicator of disease severity in patients with acute pancreatitis. Clin Res Hepatol Gastroenterol. 2012;36:162–168.
Nakai Y, Isayama H, Sasahira N, et al. Risk factors for post-ERCP pancreatitis in wire-guided cannulation for therapeutic biliary ERCP. Gastrointest Endosc. 2015;81:119–126.
Yashima Y, Isayama H, Tsujino T, et al. A large volume of visceral adipose tissue leads to severe acute pancreatitis. J Gastroenterol. 2011;46:1213–1218.
Oskarsson V, Sadr-Azodi O, Orsini N, et al. High dietary glycemic load increases the risk of non-gallstone-related acute pancreatitis: a prospective cohort study. Clin Gastroenterol Hepatol. 2014;12:676–682.
Noel RA, Braun DK, Patterson RE, Bloomgren GL. Increased risk of acute pancreatitis and biliary disease observed in patients with type 2 diabetes: a retrospective cohort study. Diabetes Care. 2009;32:834–838.
Brochu M, Starling RD, Tchernof A, et al. Visceral adipose tissue is an independent correlate of glucose disposal in older obese postmenopausal women. J Clin Endocrinol Metab. 2000;85:2378–2384.
Tulloch-Reid MK, Hanson RL, Sebring NG, et al. Both subcutaneous and visceral adipose tissue correlate highly with insulin resistance in african americans. Obes Res. 2004;12:1352–1359.
Kumar N, Gergi MA, Thompson CC. Obesity is an independent risk factor for post-ERCP pancreatitis: results of a nationwide database analysis [Abstract]. Gastrointest Endosc. 2012;75:AB142.
Johnson GK, Geenen JE, Johanson JF, et al. Evaluation of post-ERCP pancreatitis: potential causes noted during controlled study of differing contrast media. Midwest Pancreaticobiliary Study Group. Gastrointest Endosc. 1997;46:217–222.
Cennamo V, Fuccio L, Zagari RM, et al. Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk? Meta-analysis of randomized controlled trials. Endoscopy. 2010;42:381–388.
Mehta PP, Sanaka MR, Parsi MA, et al. Association of procedure length on outcomes and adverse events of endoscopic retrograde cholangiopancreatography. Gastroenterol Rep. 2014;2:140–144.
Technology Committee ASGE, Kethu SR, Adler DG, Diehl DL, et al. ERCP cannulation and sphincterotomy devices. Gastrointest Endosc. 2010;71:435–445.
Acknowledgments
Special thanks to biostatistician Sinan IYIGUN for advising and performing advanced statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We confirm that there are no financial or other relations that could lead to a conflict to interest.
Rights and permissions
About this article
Cite this article
Koksal, A.R., Boga, S., Alkim, H. et al. Insulin Resistance as a Novel Risk Factor for Post-ERCP Pancreatitis: A Pilot Study. Dig Dis Sci 61, 2397–2405 (2016). https://doi.org/10.1007/s10620-016-4127-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4127-0