Abstract
Background
Choledocholithiasis is one of the causes of jaundice and may require urgent treatment. Endoscopic retrograde cholangiopancreatography (ERCP) has been the primary management strategy for choledocholithiasis. However, small stones can be overlooked during ERCP.
Aim
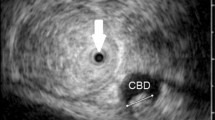
The aim of this study was to evaluate the accuracy of intraductal ultrasonography (IDUS) for detecting choledocholithiasis in icteric patients with highly suspected common bile duct (CBD) stones without definite stone diagnosis on ERCP.
Methods
Ninety-five icteric (bilirubin ≥3 mg/dL) patients who underwent ERCP for highly suspected choledocholithiasis without definite filling defects on cholangiography were prospectively enrolled in the present study. We evaluated the bile duct using IDUS for the presence of stones or sludge. Reference standard for choledocholithiasis was endoscopic extraction of stone or sludge.
Result
Bile duct stones were detected with IDUS in 31 of 95 patients (32.6 %). IDUS findings were confirmed by endoscopic stone extraction in all patients. The mean diameter of CBD stones detected by IDUS was 2.9 mm (range 1–7 mm). IDUS revealed biliary sludge in 24 patients (25.2 %) which was confirmed by sludge extraction in 21 patients (87.5 %). In dilated CBD, detection rate of bile duct stone/sludge based on IDUS was significantly higher than in non-dilated CBD (p = 0.004).
Conclusion
IDUS is useful for the detection of occult CBD stone on ERCP in icteric patients with highly suspected CBD stones.



Similar content being viewed by others
Abbreviations
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- IDUS:
-
Intraductal ultrasonography
- CBD:
-
Common bile duct
- EST:
-
Endoscopic sphincterotomy
- EUS:
-
Endoscopic ultrasonography
- CT:
-
Computed tomography
- MRCP:
-
Magnetic resonance cholangiopancreatography
- US:
-
Ultrasonography
- GB:
-
Gallbladder
- SD:
-
Standard deviation
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- CI:
-
Confidence interval
References
Frank BB. Clinical evaluation of jaundice. A guideline of the Patient Care Committee of the American Gastroenterological Association. JAMA. 1989;262:3031–3034.
Williams EJ, Green J, Beckingham I, et al. Guidelines on the management of common bile duct stones (CBDS). Gut. 2008;57:1004–1021.
Sanders G, Kingsnorth AN. Gallstones. BMJ. 2007;335:295–299.
Das A, Isenberg G, Wong RC, et al. Wire-guided intraductal US: an adjunct to ERCP in the management of bile duct stones. Gastrointest Endosc. 2001;54:31–36.
Buscarini E, Tansini P, Vallisa D, et al. EUS for suspected choledocholithiasis: do benefits outweigh costs? A prospective, controlled study. Gastrointest Endosc. 2003;57:510–518.
Polkowski M, Regula J, Tilszer A, et al. Endoscopic ultrasound versus endoscopic retrograde cholangiography for patients with intermediate probability of bile duct stones: a randomized trial comparing two management strategies. Endoscopy. 2007;39:296–303.
Moon JH, Cho YD, Cha SW, et al. The detection of bile duct stones in suspected biliary pancreatitis: comparison of MRCP, ERCP, and intraductal US. Am J Gastroenterol. 2005;100:1051–1057.
Liu CL, Lo CM, Chan JK, et al. Detection of choledocholithiasis by EUS in acute pancreatitis: a prospective evaluation in 100 consecutive patients. Gastrointest Endosc. 2001;54:325–330.
Catanzaro A, Pfau P, Isenberg GA, et al. Clinical utility of intraductal US for evaluation of choledocholithiasis. Gastrointest Endosc. 2003;57:648–652.
Lee YT, Chan FK, Leung WK, et al. Comparison of EUS and ERCP in the investigation with suspected biliary obstruction caused by choledocholithiasis: a randomized study. Gastrointest Endosc. 2008;67:660–668.
Maple JT, Ben-Menachem T, Anderson MA, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71:1–9.
Katz D, Nikfarjam M, Sfakiotaki A, et al. Selective endoscopic cholangiography for the detection of common bile duct stones in patients with cholelithiasis. Endoscopy. 2004;36:1045–1049.
Amouyal P, Amouyal G, Levy P, et al. Diagnosis of choledocholithiasis by endoscopic ultrasonography. Gastroenterology. 1994;106:1062–1067.
Prat F, Amouyal G, Amouyal P, et al. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common-bileduct lithiasis. Lancet. 1996;347:75–79.
Soto JA, Barish MA, Yucel EK, et al. Magnetic resonance cholangiography: comparison with endoscopic retrograde cholangiopancreatography. Gastroenterology. 1996;110:589–597.
Ohashi A, Ueno N, Tamada K, et al. Assessment of residual bile duct stones with use of intraductal US during endoscopic balloon sphincteroplasty: comparison with balloon cholangiography. Gastrointest Endosc. 1999;49:328–333.
Tseng LJ, Jao YT, Mo LR, et al. Over-the-wire US catheter probe as an adjunct to ERCP in the detection of choledocholithiasis. Gastrointest Endosc. 2001;54:720–723.
Gregg JA, De Girolami P, Carr-Locke DL. Effects of sphincteroplasty and endoscopic sphincterotomy on the bacteriologic characteristics of the common bile duct. Am J Surg. 1985;149:668–671.
Sand J, Airo I, Hiltunen KM, et al. Changes in biliary bacteria after endoscopic cholangiography and sphincterotomy. Am Surg. 1992;58:324–328.
Doi S, Yasuda I, Mukai T, et al. Comparison of long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation: a propensity score-based cohort analysis. J Gastroenterol. 2012;48:1090–1096.
Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol. 2002;97:2763–2767.
Kubota Y, Takaoka M, Yamamoto S, et al. Diagnosis of common bile duct calculi with intraductal ultrasonography during endoscopic biliary cannulation. J Gastroenterol Hepatol. 2002;17:708–712.
Tamada K, Ohashi A, Tomiyama T, et al. Comparison of intraductal ultrasonography with percutaneous transhepatic cholangioscopy for the identification of residual bile duct stones during lithotripsy. J Gastroenterol Hepatol. 2001;16:100–103.
Fritz E, Kirchgatterer A, Hubner D, et al. ERCP is safe and effective in patients 80 years of age and older compared with younger patients. Gastrointest Endosc. 2006;64:899–905.
Mitchell RMS, O’Connor F, Dickey W. Endoscopic retrograde cholangiopancreatography is safe and effective in patients 90 years of age and older. J Clin Gastroenterol. 2003;36:72–74.
Gangi S, Saidi F, Patel K, et al. Cardiovascular complications after GI endoscopy: occurrence and risks in a large hospital system. Gastrointest Endosc. 2004;60:679–685.
Kerker A, Hardt C, Schlief HE, et al. Combined sedation with midazolam/propofol for gastrointestinal endoscopy in elderly patients. BMC Gastroenterol. 2010;10:11.
Acknowledgments
This work was supported by the SoonChunHyang University Research Fund. We thank A Ri Song, RN; Song Ah Jeong, RN; Sun Yeong Moon, RN; and the entire nursing staff for their support and assistance with the procedures.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, D.C., Moon, J.H., Choi, H.J. et al. Usefulness of Intraductal Ultrasonography in Icteric Patients with Highly Suspected Choledocholithiasis Showing Normal Endoscopic Retrograde Cholangiopancreatography. Dig Dis Sci 59, 1902–1908 (2014). https://doi.org/10.1007/s10620-014-3127-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3127-1