Abstract
Background
Limited nationwide data currently exists regarding corticosteroid (CS) use and long-term outcome after CS initiation in ulcerative colitis (UC).
Aims
The purpose of this study was to assess CS use prevalence and long-term outcomes after the index CS exposure. Our outcomes of interest were CS use level (reintroduction, dependency, and refractoriness), thiopurine use, and colectomy.
Methods
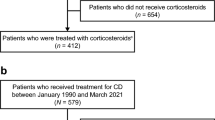
Nationwide data was obtained from the Veterans Affairs (VA) healthcare system for the period 2001–2011. Patients with UC were included if they had been diagnosed in the VA system and if they had filled CS for the first time during the observation period. A retrospective cohort design and time-to-event survival analysis was used to track outcomes of interest.
Results
A total of 1,038 newly-diagnosed patients with UC were identified. The prevalence of CS use over the observation period was 45 %. Four hundred sixty-four CS users with median follow-up of 3.4 years were included. Among the included patients, 65 % required CS reintroduction, 38 % were classified as CS dependent, and 11 % were classified as CS refractory mostly within 2 years after the index CS course. Respectively, 8.6 and 38 % had colectomy and received thiopurine. Colectomy and thiopurine use rates varied significantly according to CS use level.
Conclusions
Approximately half of newly-diagnosed patients with UC required CS. Among CS users, one third of the patients had a sustained response after the initial CS course while two-thirds required further CS therapy. We observed a trend towards higher than previously reported thiopurine use accompanied by marked reduction in colectomy rates.



Similar content being viewed by others
References
Loftus CG, Loftus EV, Harmsen WS, et al. Update on the incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota, 1940–2000. Inflamm Bowel Dis. 2007;13:254–261.
Langholz E, Munkholm P, Nielsen OH, Kreiner S, Binder V. Incidence and prevalence of ulcerative colitis in Copenhagen county from 1962 to 1987. Scand J Gastroenterol. 1991;26:1247–1256.
Kornbluth A, Sachar DB. Gastroenterology PPCotACo. Ulcerative colitis practice guidelines in adults: American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105:501–523 (quiz 524).
Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955;2:1041–1048.
Ford AC, Bernstein CN, Khan KJ, et al. Glucocorticosteroid therapy in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106:590–599 (quiz 600).
Ho GT, Chiam P, Drummond H, Loane J, Arnott ID, Satsangi J. The efficacy of corticosteroid therapy in inflammatory bowel disease: analysis of a 5-year UK inception cohort. Aliment Pharmacol Ther. 2006;24:319–330.
Faubion WA, Loftus EV, Harmsen WS, Zinsmeister AR, Sandborn WJ. The natural history of corticosteroid therapy for inflammatory bowel disease: a population-based study. Gastroenterology. 2001;121:255–260.
The National Center for Veterans Analysis and Statistics (NCVAS). Trends in the Utilization of VA Programs and Services. 2012; www.va.gov/vetdata. Accessed 21 April 2012.
Khan N, Abbas AM, Almukhtar RM, Khan A. Prevalence and predictors of low bone mineral density in males with ulcerative colitis. J Clin Endocrinol Metab. 2013;98:2368–2375.
Garcia-Planella E, Mañosa M, Van Domselaar M, et al. Long-term outcome of ulcerative colitis in patients who achieve clinical remission with a first course of corticosteroids. Dig Liver Dis. 2012;44:206–210.
Targownik LE, Singh H, Nugent Z, Bernstein CN. The epidemiology of colectomy in ulcerative colitis: results from a population-based cohort. Am J Gastroenterol. 2012;107:1228–1235.
Henriksen M, Jahnsen J, Lygren I, et al. Ulcerative colitis and clinical course: results of a 5-year population-based follow-up study (the IBSEN study). Inflamm Bowel Dis. 2006;12:543–550.
Ha CY, Newberry RD, Stone CD, Ciorba MA. Patients with late-adult-onset ulcerative colitis have better outcomes than those with early onset disease. Clin Gastroenterol Hepatol. 2010;8:682–687.
Solberg IC, Lygren I, Jahnsen J, et al. Clinical course during the first 10 years of ulcerative colitis: results from a population-based inception cohort (IBSEN Study). Scand J Gastroenterol. 2009;44:431–440.
Klein RE, Stockford DD. Data on the Socioeconomic Status of Veterans and on VA Program Usage. Office of the Actuary, Veterans Health Administration. 2001; http://www.va.gov/vetdata/docs/SpecialReports/sesprogramnet5-31-01.pdf. Accessed 10 June 2013.
Thirumurthi S, Chowdhury R, Richardson P, Abraham NS. Validation of ICD-9-CM diagnostic codes for inflammatory bowel disease among veterans. Dig Dis Sci. 2010;55:2592–2598.
Morgan RO, Petersen LA, Hasche JC, et al. VHA pharmacy use in veterans with medicare drug coverage. Am J Manag Care. 2009;15:e1–e8.
Wolinsky FD, Miller TR, An H, Brezinski PR, Vaughn TE, Rosenthal GE. Dual use of medicare and the Veterans Health Administration: are there adverse health outcomes? BMC Health Serv Res. 2006;6:131.
U.S. Government Accountability Office Report. Veterans Health Care: Use of VA Services by Medicare-Eligible Veterans. 1994; http://www.gao.gov/products/HEHS-95-13. Accessed 19 February 2013.
Acknowledgments
This study was funded in full by the Department of Veterans Affairs, Veterans Health Administration, Office of Research & Development Health Services, grant number (VA Project No. 425).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khan, N., Abbas, A., Williamson, A. et al. Prevalence of Corticosteroids Use and Disease Course After Initial Steroid Exposure in Ulcerative Colitis. Dig Dis Sci 58, 2963–2969 (2013). https://doi.org/10.1007/s10620-013-2748-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-013-2748-0