Abstract
Background
Globus sensation is common, but its pathogenesis is not yet clear.
Aims
Our purpose was to investigate subjective perception of swallowing and esophageal motility by combined multichannel intraluminal impedance and manometry (MII-EM) for patients with globus sensation.
Methods
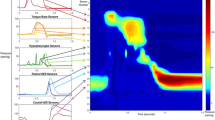
Combined MII-EM was performed for 25 globus patients and 15 healthy controls. Swallows were abnormal if hypocontractivity or simultaneous contractions occurred. Esophageal bolus transit was incomplete if bolus exit was not found at one or more of all measurement sites. Perception of each swallow was assessed by use of a standardized scoring system, and was enhanced if the score was >1.
Results
Few globus patients reported enhanced perception during viscous or solid swallows. Incomplete bolus transit and enhanced perception occurred similarly between viscous and solid boluses. Agreement between enhanced perception and proximal bolus clearance was greater during solid swallows (κ = 0.45, 95 % CI: 0.32–0.58) than during viscous swallows (κ = 0.13, 95 % CI: 0–0.25) (P < 0.05). Similarly, agreement between enhanced perception and total bolus clearance was greater during solid swallows (κ = 0.46, 95 % CI: 0.34–0.58) than during viscous swallows (κ = 0.11, 95 % CI: 0–0.22) (P < 0.05).
Conclusions
Enhanced swallow perception is uncommon in patients with globus sensation, although there is a significant association between enhanced esophageal perception and solid bolus clearance. Application of a solid bolus may help better delineation of the interrelationship between the subjective perception of bolus passage and the objective measurement of bolus clearance.

Similar content being viewed by others
References
Moloy PJ, Charter R. The globus symptom. Incidence, therapeutic response, and age and sex relationships. Arch Otolaryngol. 1982;108:740–744.
Watson WC, Sullivan SN. Hypertonicity of the cricopharyngeal sphincter: a cause of globus sensation. Lancet. 1974;2:1417–1419.
Wilson JA, Pryde A, Piris J, et al. Pharyngoesophageal dysmotility in globus sensation. Arch Otolaryngol Head Neck Surg. 1989;115:1086–1090.
Batch AJ. Globus pharyngeus (Part I). J Laryngol Otol. 1988;102:152–158.
Harris MB, Deary IJ, Wilson JA. Life events and difficulties in relation to the onset of globus pharyngis. J Psychosom Res. 1996;40:603–615.
Wilson JA, Deary IJ, Maran AG. The persistence of symptoms in patients with globus pharyngis. Clin Otolaryngol Allied Sci. 1991;16:202–205.
Silny J. Intraluminal multiple electric impedance procedure for measurement of gastrointestinal motility. Neurogastroenterol Motil. 1991;3:151–162.
Simren M, Silny J, Holloway R, Tack J, Janssens J, Sifrim D. Relevance of ineffective oesophageal motility during oesophageal acid clearance. Gut. 2003;52:784–790.
Chen CL, Yi CH. Clinical correlates of dysphagia to oesophageal dysmotility: studies using combined manometry and impedance. Neurogastroenterol Motil. 2008;20:611–617.
Tutuian R, Vela MF, Balaji NS, et al. Esophageal function testing with combined multichannel intraluminal impedance and manometry: multicenter study in healthy volunteers. Clin Gastroenterol Hepatol. 2003;1:174–182.
Spechler SJ, Castell DO. Classification of oesophageal motility abnormalities. Gut. 2001;49:145–151.
Chen CL, Yi CH. Assessment of esophageal motor function using combined multichannel intraluminal impedance and manometry in healthy volunteers: a single-center study in Taiwan. J Gastroenterol Hepatol. 2007;22:1039–1043.
Byrt T, Bishop J, Carlin JB. Bias, prevalence and kappa. J Clin Epidemiol. 1993;46:423–429.
Lin HM, Williamson JM, Lipsitz SR. Calculating power for the comparison of dependent κ-coefficients. Appl Stat. 2003;52:391–404.
Farkkila MA, Ertama L, Katila H, Kuusi K, Paavolainen M, Varis K. Globus pharyngis, commonly associated with esophageal motility disorders. Am J Gastroenterol. 1994;89:503–508.
Wilson JA, Hawkins RA, Sangster K, et al. Estimation of oestrogen and progesterone receptors in chronic rhinitis. Clin Otolaryngol Allied Sci. 1986;11:213–218.
Adachi J, Ohmae Y, Karaho T, et al. Relationship between globus sensation and esophageal clearance. Acta Otolaryngol. 2010;130:138–144.
Chen CL, Szczesniak MM, Cook IJ. Evidence for oesophageal visceral hypersensitivity and aberrant symptom referral in patients with globus. Neurogastroenterol Motil. 2009;21:e1142–e1196.
Allen ML, Orr WC, Mellow MH, Robinson MG. Water swallows versus food ingestion as manometric tests for esophageal dysfunction. Gastroenterology. 1988;95:831–833.
Anand P, Aziz Q, Willert R, van Oudenhove L. Peripheral and central mechanisms of visceral sensitization in man. Neurogastroenterol Motil. 2007;19:29–46.
Cook IJ, Dent J, Collins SM. Upper esophageal sphincter tone and reactivity to stress in patients with a history of globus sensation. Dig Dis Sci. 1989;34:672–676.
Galmiche JP, Clouse RE, Balint A, et al. Functional esophageal disorders. Gastroenterology. 2006;130:1459–1465.
Bradley LA, Richter JE, Scarinci IC, Halle JM, Schan CA. Mechanisms of altered pain perception in non-cardiac chest pain patients. Gastroenterology. 1993;104:A482.
Whitehead WE, Croweil MD, Davidoff A, Cheskin L, Schuster MM. Is sexual abuse associated with lower thresholds for pain due to balloon distension of the rectum? Gastroenterology. 1994;106:A588.
Acknowledgments
This study was supported by a grant, NSC 99-2314-B-303-005, from the National Science Council, Taiwan. Part of this study was presented as a poster presentation at DDW 2012 in San Diego and was published in abstract form in Gastroenterology (2012) 142 (5 Suppl. 1):S282.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, CL., Yi, CH. & Liu, TT. Association Between Swallow Perception and Esophageal Bolus Clearance in Patients with Globus Sensation. Dig Dis Sci 58, 1042–1048 (2013). https://doi.org/10.1007/s10620-012-2463-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2463-2