Abstract
Background
During inflammation in the gastrointestinal tract, the production of nitric oxide (NO) is mediated by the mucosal conversion of l-arginine. Recently, it was shown that the gut microbiota can also produce NO.
Aims
The effect of gut luminal NO on inflammatory processes of an experimental colitis mice model was investigated by administrating NO directly to the colon, mimicking microbial NO production.
Methods
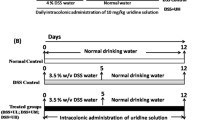
Twenty-four mice received daily intrarectal treatment with a NO donor in 2 doses and 8 mice were treated with placebo. Starting 1 day later, 18 of these mice were fed ad libitum with 4% of dextran sodium sulfate (DSS) in their drinking water to induce colitis. At day 6, histopathology (both the inflammation and damage score), myeloperoxidase (MPO)-activity, colon length and colonic permeability were evaluated.
Results
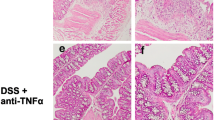
Co-administration of NO during DSS exposure inhibited the induction of an increasing colonic MPO-activity. This protective effect of NO was confirmed by the histological inflammation score showing a similar trend. The colonic permeability was restored when very low levels of NO were administered to the DSS-mice. On the other hand, the colon length of the NO-treated DSS-mice was negatively correlated with the NO dose and the histological damage score was not improved.
Conclusions
Our results indicate that intrarectal administration of NO has clear anti-inflammatory effects in experimental colitis, but does not prevent colonic damage. Therefore, NO-producing microorganisms in the gut lumen should be accounted as a modulating process during colitis.



Similar content being viewed by others
References
Moncada S. Nitric oxide: discovery and impact on clinical medicine. J R Soc Med. 1999;92:164–169.
Herulf M, Ljung T, Hellstrom PM, Weitzberg E, Lundberg JON. Increased luminal nitric oxide in inflammatory bowel disease as shown with a novel minimally invasive method. Scand J Gastroenterol. 1998;33:164–169.
Boughton-Smith NK, Evans SM, Hawkey CJ, et al. Nitric-oxide synthase activity in ulcerative colitis and Crohn’s disease. Lancet. 1993;342:338–340.
Middleton SJ, Shorthouse M, Hunter JO. Increased nitric-oxide synthesis in ulcerative colitis. Lancet. 1993;341:465–466.
Rachmilewitz D, Stamler JS, Bachwich D, Karmeli F, Ackerman Z, Podolsky DK. Enhanced colonic nitric-oxide generation and nitric-oxide synthase activity in ulcerative colitis and Crohn’s disease. Gut. 1995;36:718–723.
Rachmilewitz D, Karmeli F, Okon E, Bursztyn M. Experimental colitis is ameliorated by inhibition of nitric-oxide synthase activity. Gut. 1995;37:247–255.
Zingarelli B, Szabo C, Salzman AL. Reduced oxidative and nitrosative damage in murine experimental colitis in the absence of inducible nitric oxide synthase. Gut. 1999;45:199–209.
Reinders CI, Jonkers D, Jansson EA, et al. Rectal nitric oxide and fecal calprotectin in inflammatory bowel disease. Scand J Gastroenterol. 2007;42:1151–1157.
Sobko T, Reinders CI, Jansson EA, Norin E, Midtvedt T, Lundberg JO. Gastrointestinal bacteria generate nitric oxide from nitrate and nitrite. Nitric Oxide-Biol Chem. 2005;13:272–278.
Vermeiren J, Van de Wiele T, Verstraete W, Boeckx P, Boon N. Nitric oxide production by the human intestinal microbiota by dissimilatory nitrate reduction to ammonium. J Biomed Biotechnol. 2009:10. doi:10.1155/2009/284718.
Roediger WEW. Review article: nitric oxide from dysbiotic bacterial respiration of nitrate in the pathogenesis and as a target for therapy of ulcerative colitis. Aliment Pharmacol Ther. 2008;27:531–541.
Vermeiren J, Van de Wiele T, Van Nieuwenhuyse G, Boeckx P, Verstraete W, Boon N. Sulfide- and nitrite- dependent nitric oxide production in the intestinal tract. Microbial Biotechnol. 2012. doi:10.1111/j.1751-7915.2011.00320.x.
Van der Sluis M, De Koning BAE, De Bruijn A, et al. Muc2-deficient mice spontaneously develop colitis, indicating that muc2 is critical for colonic protection. Gastroenterology. 2006;131:117–129.
Hindryckx P, Waeytens A, Laukens D, et al. Absence of placental growth factor blocks dextran sodium sulfate-induced colonic mucosal angiogenesis, increases mucosal hypoxia and aggravates acute colonic injury. Lab Invest. 2010;90:566–576.
Napolitano LM, Koruda MJ, Meyer AA, Baker CC. The impact of femur fracture with associated soft tissue injury on immune function and intestinal permeability. Shock. 1996;5:202–207.
Lamine F, Eutamene H, Fioramonti J, Bueno L, Theodorou V. Colonic responses to Lactobacillus farciminis treatment in trinitrobenzene sulphonic acid-induced colitis in rats. Scand J Gastroenterol. 2004;39:1250–1258.
Lamine F, Fioramonti J, Bueno L, et al. Nitric oxide released by Lactobacillus farciminis improves TNBS-induced colitis in rats. Scand J Gastroenterol. 2004;39:37–45.
Wallace JL, Vergnolle N, Muscara MN, et al. Enhanced anti-inflammatory effects of a nitric oxide-releasing derivative of mesalamine in rats. Gastroenterology. 1999;117:557–566.
Wolf G, Arendt EK, Pfahler U, Hammes WP. Heme-dependent and heme-independent nitrite reduction by lactic-acid bacteria results in different N-containing products. Int J Food Microbiol. 1990;10:323–329.
Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004;118:229–241.
Salzman AL, Menconi MJ, Unno N, et al. Nitric-oxide dilates tight junctions and depletes ATP in cultured Caco-2bbe intestinal epithelial monolayers. Am J Physiol-Gastroint Liver Physiol. 1995;31:G361–G373.
Yamamoto A, Tatsumi H, Maruyama M, Uchiyama T, Okada N, Fujita T. Modulation of intestinal permeability by nitric oxide donors: Implications in intestinal delivery of poorly absorbable drugs. J Pharmacol Exp Ther. 2001;296:84–90.
Resta-Lenert S, Barrett KE. Live probiotics protect intestinal epithelial cells from the effects of infection with enteroinvasive Escherichia coli (EIEC). Gut. 2003;52:988–997.
Acknowledgments
We like to thank Varvara Tsilia for her help in sacrificing the mice. This work was supported by a Concerted Research Action of the Flemish Community (GOA) (BOF07/GOA/002).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vermeiren, J., Hindryckx, P., Van Nieuwenhuyse, G. et al. Intrarectal Nitric Oxide Administration Prevents Cellular Infiltration but Not Colonic Injury During Dextran Sodium Sulfate Colitis. Dig Dis Sci 57, 1832–1837 (2012). https://doi.org/10.1007/s10620-012-2105-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2105-8