Abstract
Background
Disruption of epithelial tight junctions (TJ) followed by loss of barrier function is of crucial importance in the pathogenesis of a variety of gastrointestinal disorders. Heme oxygenase-1 (HO-1), which can be induced by curcumin (Cur), provides protection against various forms of oxidative stress.
Aims
The protective effect of Cur on oxidative stress-induced intestinal barrier disruption in human intestinal epithelial cells was elucidated in this study.
Methods
H2O2-induced Caco-2 enterocytic monolayers were incubated in the presence or absence of Cur and/or zinc protoporphyrin (ZnPP). The trans-epithelial electrical resistance (TEER) and the flux of sodium fluorescein in the filter-grown Caco-2 cell monolayers were measured. The expression and localization of the TJ protein occludin and zonula occluden-1 (ZO-1) were evaluated by western blot and immunofluorescence microscopy. The mRNA and protein levels of HO-1 were analyzed by real-time PCR and western blot.
Results
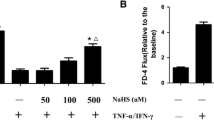
Cur attenuated H2O2-induced disruption of paracellular permeability (TEER 52.02 ± 10.15% vs 22.71 ± 3.11%; sodium fluorescein flux 12.41 ± 2.19% vs 32.00 ± 4.97%, P < 0.05) and induced HO-1 mRNA (6.64 ± 0.48 vs 3.22 ± 0.28, P < 0.05) and protein (291.00 ± 9.17% vs 99.00 ± 10.00%, P < 0.05) expression in Caco-2 cells. After administration of H2O2, occludin and ZO-1 proteins were restored by Cur (occludin 175.67 ± 29.50% vs 53.67 ± 24.19%, P < 0.05; ZO-1 139.67 ± 33.71% vs 36.00 ± 15.88%, P < 0.05) and this effect was blocked by HO-1 inhibitor, ZnPP (occludin 54.67 ± 10.02% vs 168.33 ± 36.47%, P < 0.05; ZO-1 50.00 ± 15.13% vs 117.67 ± 38.81%, P < 0.05).
Conclusion
Cur protects human intestinal epithelial cells against H2O2-induced disruption of TJ and barrier dysfunction via the HO-1 pathway.






Similar content being viewed by others
Abbreviations
- TJ:
-
Tight junction
- OJ:
-
Obstructive jaundice
- IBD:
-
Inflammatory bowel disease
- AP:
-
Acute pancreatitis
- Cur:
-
Curcumin
- AJ:
-
Adhere junctions
- JAM:
-
Junctional adhesion molecule
- ZOs:
-
Zonula occludens
- H2O2 :
-
Hydrogen peroxide
- HO-1:
-
Heme oxygenase-1
- DMEM:
-
Dulbecco’s Vogt modified Eagle’s media
- TEER:
-
Trans-epithelial electrical resistance
- ZnPP:
-
Zinc protoporphyrin
- LDH:
-
Lactate dehydrogenase
- MDA:
-
Malondialdehyde
References
Catalioto RM, Maggi CA, Giuliani S. Intestinal epithelial barrier dysfunction in disease and possible therapeutical interventions. Curr Med Chem. 2011;18:398–426.
Weber CR, Turner JR. Inflammatory bowel disease: is it really just another break in the wall? Gut. 2007;56:6–8.
Tsukita S, Furuse M, Itoh M. Multifunctional strands in tight junctions. Natl Rev Mol Cell Biol. 2001;2:285–293.
Schneeberger EE, Lynch RD. The tight junction: a multifunctional complex. Am J Physiol Cell Physiol. 2004;286:C1213–C1228.
Wang N, Yu H, Ma J, et al. Evidence for tight junction protein disruption in intestinal mucosa of malignant obstructive jaundice patients. Scand J Gastroenterol. 2010;45:191–199.
Besselink MG, van Santvoort HC, Renooij W, et al. Intestinal barrier dysfunction in a randomized trial of a specific probiotic composition in acute pancreatitis. Ann Surg. 2009;250:712–719.
Zhang R, Hu Y, Yuan J, et al. Effects of puerariae radix extract on the increasing intestinal permeability in rat with alcohol-induced liver injury. J Ethnopharmacol. 2009;126:207–214.
Chen ML, Ge Z, Fox JG, Schauer DB. Disruption of tight junctions and induction of proinflammatory cytokine responses in colonic epithelial cells by Campylobacter jejuni. Infect Immun. 2006;74:6581–6589.
Tanida S, Mizoshita T, Mizushima T, et al. Involvement of oxidative stress and mucosal address in cell adhesion molecule-1 (MAdCAM-1) in inflammatory bowel disease. J Clin Biochem Nutr. 2011;48:112–116.
Basuroy S, Seth A, Elias B, Naren AP, Rao R. MAPK interacts with occludin and mediates EGF-induced prevention of tight junction disruption by hydrogen peroxide. Biochem J. 2006;393:69–77.
Audus KL, Bartel RL, Hidalgo IJ, Borchardt RT. The use of cultured epithelial and endothelial cells for drug transport and metabolism studies. Pharm Res. 1990;7:435–451.
Artursson P, Palm K, Luthman K. Caco-2 monolayers in experimental and theoretical predictions of drug transport. Adv Drug Deliv Rev. 2001;46:27–43.
Oshima T, Sasaki M, Kataoka H, Miwa H, Takeuchi T, Joh T. Wip1 protects hydrogen peroxide-induced colonic epithelial barrier dysfunction. Cell Mol Life Sci. 2007;64:3139–3147.
Jepson MA. Disruption of epithelial barrier function by H2O2: distinct responses of Caco-2 and Madin–Darby canine kidney (MDCK) strains. Cell Mol Biol. 2003;49:101–112.
Seth A, Yan F, Polk DB, Rao RK. Probiotics ameliorate the hydrogen peroxide-induced epithelial barrier disruption by a PKC- and MAP kinase-dependent mechanism. Am J Physiol Gastrointest Liver Physiol. 2008;294:G1060–G1069.
Rao RK, Baker RD, Baker SS, Gupta A, Holycross M. Oxidant-induced disruption of intestinal epithelial barrier function: role of protein tyrosine phosphorylation. Am J Physiol. 1997;273:G812–G823.
Pedersen CB, Gregersen N. Stress response profiles in human fibroblasts exposed to heat shock or oxidative stress. Methods Mol Biol. 2010;648:161–173.
Motterlini R, Foresti R, Bassi R, Green CJ. Curcumin, an antioxidant and anti-inflammatory agent, induces heme oxygenase-1 and protects endothelial cells against oxidative stress. Free Radic Biol Med. 2000;28:1303–1312.
Prawan A, Keum YS, Khor TO, et al. Structural influence of isothiocyanates on the antioxidant response element (ARE)-mediated heme oxygenase-1 (HO-1) expression. Pharm Res. 2008;25:836–844.
Srinivasan A, Menon VP, Periaswamy V, Rajasekaran KN. Protection of pancreatich beta-cell by the potential antioxidant bis-o-hydroxycinnamoyl methane, analogue of natural curcuminoid in experimental diabetes. J Pharm Pharm Sci. 2003;6:327–333.
McNally SJ, Harrison EM, Ross JA, Garden OJ, Wigmore SJ. Curcumin induces heme oxygenase 1 through generation of reactive oxygen species, p38 activation and phosphatase inhibition. Int J Mol Med. 2007;19:165–172.
Banan A, Fields JZ, Decker H, Zhang Y, Keshavarzian A. Nitric oxide and its metabolites mediate ethanol-induced microtubule disruption and intestinal barrier dysfunction. J Pharmacol Exp Ther. 2000;294:997–1008.
Ma J, Li F, Liu L, et al. Raf kinase inhibitor protein inhibits cell proliferation but promotes cell migration in rat hepatic stellate cells. Liver Int. 2009;29:567–574.
Wijeratne SS, Cuppett SL, Schlegel V. Hydrogen peroxide induced oxidative stress damage and antioxidant enzyme response in Caco-2 human colon cells. J Agric Food Chem. 2005;53:8768–8774.
Guo X, Rao JN, Liu L, et al. Polyamines are necessary for synthesis and stability of occludin protein in intestinal epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2005;288:G1159–G1169.
Jiang H, Deng CS, Zhang M, Xia J. Curcumin-attenuated trinitrobenzene sulphonic acid induces chronic colitis by inhibiting expression of cyclooxygenase-2. World J Gastroenterol. 2006;12:3848–3853.
Bao W, Li K, Rong S, et al. Curcumin alleviates ethanol-induced hepatocytes oxidative damage involving heme oxygenase-1 induction. J Ethnopharmacol. 2010;128:549–553.
Ma TY, Iwamoto GK, Hoa NT, et al. TNF-alpha-induced increase in intestinal epithelial tight junction permeability requires NF-kappa B activation. Am J Physiol Gastrointest Liver Physiol. 2004;286:G367–G376.
Tullius SG, Nieminen-Kelhä M, Buelow R, et al. Inhibition of ischemia/reperfusion injury and chronic graft deterioration by a single-donor treatment with cobalt-protoporphyrin for the induction of heme oxygenase-1. Transplantation. 2002;74:591–598.
Balogun E, Hoque M, Gong P, et al. Curcumin activates the haem oxygenase-1 gene via regulation of Nrf2 and the antioxidant-responsive element. Biochem J. 2003;371:887–895.
Huang MT, Newmark HL, Frenkel K. Inhibitory effects of curcumin on tumorigenesis in mice. J Cell Biochem Suppl. 1997;27:26–34.
La P, Fernando AP, Wang Z, et al. Zinc protoporphyrin regulates cyclin D1 expression independent of heme oxygenase inhibition. J Biol Chem. 2009;284:36302–36311.
Acknowledgments
This work was supported in part by a grant to Huiqing Jiang from the National Natural Science Foundation of China (no. 81170411), the Natural Science Foundation of Hebei Province, China (no. C2010000530), and the Health Department Foundation of Hebei Province, China (no. 20090377).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Na Wang and Gai Wang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, N., Wang, G., Hao, J. et al. Curcumin Ameliorates Hydrogen Peroxide-Induced Epithelial Barrier Disruption by Upregulating Heme Oxygenase-1 Expression in Human Intestinal Epithelial Cells. Dig Dis Sci 57, 1792–1801 (2012). https://doi.org/10.1007/s10620-012-2094-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2094-7