Abstract
Background
The psychometric hepatic encephalopathy score (PHES) is a battery of neuropsychological tests used in the diagnosis of minimal hepatic encephalopathy (MHE).
Aim
The aim of this study was to construct and validate a dataset of normal values for the PHES.
Methods
Volunteers and patients with cirrhosis with and without low-grade overt hepatic encephalopathy (OHE) were enrolled. All subjects completed the PHES battery, and possible modifying factors were assessed. Formulas to predict expected scores in cirrhotics were constructed, and MHE was diagnosed whenever a deviation of <−4 SDs occurred across the five tests.
Results
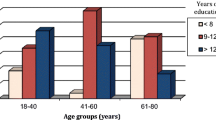
Among the 743 volunteers, age and years of education influenced the scores of all tests. Eighty-four patients with cirrhosis lacked evidence of OHE, whereas 20 had OHE: median PHES were −1 [0 to −3] and −9 [−6.5 to −11.8] (P < 0.001), respectively. Thirteen of the 84 patients (15%) with cirrhosis but without OHE had MHE. Patients with MHE were older and less educated than those without MHE (61 ± 8 and 52 ± 10 years old, P = 0.003; 7 ± 4 and 12 ± 5 years education, P = 0.002), whereas liver function was not different (MELD, 8 ± 5 and 8 ± 5). A very strong correlation between these norms and those derived from Spain was observed (r = 0.964, P < 0.001).
Conclusions
PHES performance was mostly influenced by age and education, and expected results in cirrhotics need to be adjusted for these factors. Our validation of Mexican norms for PHES (PHES-Mex) establishes a practical method for assessing MHE and contributes to international attempts to standardize diagnostic protocols for MHE.


Similar content being viewed by others
References
Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT. Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th world congresses of gastroenterology, Vienna, 1998. Hepatology. 2002;35:716–721.
Córdoba J, Mínguez B. Hepatic encephalopathy. Semin Liver Dis. 2008;28:70–80.
Torre-Delgadillo A, Cisneros-Garza L, Méndez-Sánchez N, Jacobo-Karam J, Duarte-Rojo A, Solís-Galindo F. Gastroenterology diagnosis and treatment guidelines of hepatic encephalopathy. General approach. Rev Gastroenterol Mex. 2009;74:161–163.
Bajaj JS, Wade JB, Sanyal AJ. Spectrum of neurocognitive impairment in cirrhosis: implications for the assessment of hepatic encephalopathy. Hepatology. 2009;50:2014–2021.
Bajaj JS, Saeian K, Verber MD, et al. Inhibitory control test is a simple method to diagnose minimal hepatic encephalopathy and predict development of overt hepatic encephalopathy. Am J Gastroenterol. 2007;102:754–760.
Baskin-Bey ES, Stewart CA, Mitchell MM, Bida JP, Rosenthal TJ, Nyberg SL. Preliminary report of the hepatic encephalopathy assessment driving simulator (HEADS) score. Ethn Dis. 2008;18:357–364.
Prasad S, Dhiman RK, Duseja A, Chawla YK, Sharma A, Agarwal R. Lactulose improves cognitive functions and health-related quality of life in patients with cirrhosis who have minimal hepatic encephalopathy. Hepatology. 2007;45:549–559.
Liu Q, Duan ZP, Ha DK, Bengmark S, Kurtovic J, Riordan SM. Synbiotic modulation of gut flora: effect on minimal hepatic encephalopathy in patients with cirrhosis. Hepatology. 2004;39:1441–1449.
Malaguarnera M, Gargante MP, Cristaldi E, et al. Acetyl-L-carnitine treatment in minimal hepatic encephalopathy. Dig Dis Sci. 2008;53:3018–3025.
Randolph C, Hilsabeck R, Kato A, et al. Neuropsychological assessment of hepatic encephalopathy: ISHEN practice guidelines. Liver Int. 2009;29:629–635.
Weissenborn K. PHES: one label, different goods?! J Hepatol. 2008;49:308–312.
Weissenborn K, Ennen JC, Schomerus H, Rückert N, Hecker H. Neuropsychological characterization of hepatic encephalopathy. J Hepatol. 2001;34:768–773.
Romero Gómez M, Córdoba J, Jover R, et al. Normality tables in the Spanish population for psychometric tests used in the diagnosis of minimal hepatic encephalopathy. Med Clin (Barc). 2006;127:246–249.
Amodio P, Campagna F, Olianas S, et al. Detection of minimal hepatic encephalopathy: normalization and optimization of the psychometric hepatic encephalopathy score. A neuropsychological and quantified EEG study. J Hepatol. 2008;49:346–353.
Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–470.
Virtanen A, Kairisto V, Uusipaikka E. Regression-based reference limits: determination of sufficient sample size. Clin Chem. 1998;44:2353–2358.
Bravo G, Hébert R. Age- and education-specific reference values for the mini-mental and modified mini-mental state examinations derived from a non-demented elderly population. Int J Geriatr Psychiatry. 1997;12:1008–1018.
Romero-Gómez M, Córdoba J, Jover R, et al. Value of the critical flicker frequency in patients with minimal hepatic encephalopathy. Hepatology. 2007;45:879–885.
Lockwood AH, Weissenborn K, Bokemeyer M, Tietge U, Burchert W. Correlations between cerebral glucose metabolism and neuropsychological test performance in nonalcoholic cirrhotics. Metab Brain Dis. 2002;17:29–40.
Weissenborn K, Ahl B, Fischer-Wasels D, et al. Correlations between magnetic resonance spectroscopy alterations and cerebral ammonia and glucose metabolism in cirrhotic patients with and without hepatic encephalopathy. Gut. 2007;56:1736–1742.
Amodio P, Ridola L, Schiff A, et al. Improving the inhibitory control task to detect minimal hepatic encephalpathy. Gastroenterology. 2010;139:510–518.
Bajaj JS, Schubert CM, Heuman DM, et al. Persistence of cognitive impairment after resolution of overt hepatic encephalopathy. Gastroenterology. 2010;138:2332–2340.
Jover R, Compañy L, Gutiérrez A, et al. Minimal hepatic encephalopathy and extrapyramidal signs in patients with cirrhosis. Am J Gastroenterol. 2003;98:1599–1604.
Ortiz M, Córdoba J, Doval E, et al. Development of a clinical hepatic encephalopathy staging scale. Aliment Pharmacol Ther. 2007;26:859–867.
Ortiz M, Córdoba J, Jacas C, Flavià M, Esteban R, Guardia J. Neuropsychological abnormalities in cirrhosis include learning impairment. J Hepatol. 2006;44:104–110.
Riggio O, Ridola L, Pasquale C, et al. Evidence of persistent cognitive impairment after resolution of overt hepatic encephalopathy. Clin Gastroenterol Hepatol. 2011;9:181–183.
Acknowledgments
We thank Hugo Villamil-Ramírez, Daniel Bernal-Serrano, Ricardo Macías-Rodríguez, and Marina Green-Gómez for their technical assistance, and Fundación Mexicana para la Salud Hepática (Fundhepa - FUNSALUD, México) for their invaluable support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Duarte-Rojo, A., Estradas, J., Hernández-Ramos, R. et al. Validation of the Psychometric Hepatic Encephalopathy Score (PHES) for Identifying Patients with Minimal Hepatic Encephalopathy. Dig Dis Sci 56, 3014–3023 (2011). https://doi.org/10.1007/s10620-011-1684-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1684-0