Abstract
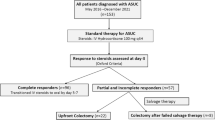
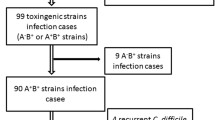
Background The incidence of Clostridium difficile infection is increasing in the United States. The aim of our investigation is to compare short-term and long-term outcomes of patients admitted with an ulcerative colitis (UC) flare and co-existent C. difficile infection to those of non-infected patients. Methods A historical cohort study was undertaken examining admissions at Mount Sinai Hospital between June 2004 and June 2005 using ICD-9 criteria for UC. Charts were abstracted for those patients for whom C. difficile testing was performed. Results Of 288 admissions, 99 charts met the inclusion criteria. Fifty-two patients were C. difficile-negative and 47 were positive. Demographic data and laboratory values upon admission did not differ between the two groups. Patients who were C. difficile-positive had significantly more UC-related hospitalizations and emergency room visits in the year following initial admission (58 visits vs. 27, P = 0.001 and eight visits vs. 1 visit (P = 0.012), respectively). One year following the index admission, C. difficile patients had significantly higher rates of colectomy compared to C. difficile-negative patients (44.6% vs. 25%, P = 0.04). Length of hospitalization (11.7 vs. 11 days), use of cyclosporine therapy during index admission (48% vs. 47% of patients), and percentage requiring colectomy at initial admission (23.4% vs. 13.5%) did not reach statistical significance. Conclusions Our data suggest that patients presenting with a UC flare who are infected with C. difficile have worse long-term clinical outcomes than those that are C. difficile-negative. C. difficile testing should be performed for all patients presenting with UC flare. Further studies are warranted to elucidate how infection can alter the natural history of UC.




Similar content being viewed by others
References
Archibald L, Banerjee S, Jarvis W. Secular trends in hospital-acquired Clostridium difficile disease in the United States, 1987–2001. J Infect Dis. 2004;189:1585–1589. doi:10.1086/383045.
Greenfield C, Aguilar Ramirez JR, Pounder RE, et al. Clostridium difficile and inflammatory bowel disease. Gut. 1983;24(8):713–717. doi:10.1136/gut.24.8.713.
Meyer A, Nizar R, Loftus E, et al. The diagnostic yield of stool pathogen studies during relapses of inflammatory bowel disease. J Clin Gastroenterol. 2004;38(9):772–775. doi:10.1097/01.mcg.0000139057.05297.d6.
Mylonaki M, Langmead L, Pantes A, et al. Enteric infection in relapse of inflammatory bowel disease: importance of microbiological examination of stool. Eur J Gastroenterol Hepatol. 2004;16(8):775–778. doi:10.1097/01.meg.0000131040.38607.09.
Kochhar R, Ayyagari A, Goenka MK, et al. Role of infectious agents in exacerbation of ulcerative colitis in India: a study of Clostridium difficile. J Clin Gastroenterol. 1993;16(1):26–30. doi:10.1097/00004836-199301000-00008.
Trnka YM, LaMont JT. Association of Clostridium difficile toxin with symptomatic relapse of chronic inflammatory bowel disease. Gastroenterology. 1981;80(4):693–696.
Weber P, Koch M, Heizmann WR, et al. Microbic superinfection in relapse of inflammatory bowel disease. J Clin Gastroenterol. 1992;14(4):302–308. doi:10.1097/00004836-199206000-00008.
Rodemann J, Dubberke E, Reske K, et al. Incidence of Clostridium difficile infection in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007;5(3):339–344. doi:10.1016/j.cgh.2006.12.027.
Meyers S, Mayer L, Bottone E, et al. Occurrence of Clostridium difficile toxin during the course of inflammatory bowel disease. Gastroenterology. 1981;80(4):697–700.
LaMont JT, Trnka YM. Therapeutic implications of Clostridium difficile toxin during relapse of chronic inflammatory bowel disease. Lancet. 1980;1(8165):381–383. doi:10.1016/S0140-6736(80)90939-3.
Bolton RP, Sherriff RJ, Read AE. Clostridium difficile associated diarrhea: a role in inflammatory bowel disease? Lancet. 1980;1(8165):383–384. doi:10.1016/S0140-6736(80)90940-X.
Rüssmann H, Panthel K, Bader RC, et al. Evaluation of three rapid assays for detection of Clostridium difficile toxin A and toxin B in stool specimens. Eur J Clin Microbiol Infect Dis. 2007;26(2):115–119. doi:10.1007/s10096-006-0251-7.
Aldeen WE, Bingham M, Aiderzada A, et al. Comparison of the TOX A/B test to a cell culture cytotoxicity assay for the detection of Clostridium difficile in stools. Diagn Microbiol Infect Dis. 2000;36(4):211–213. doi:10.1016/S0732-8893(00)00113-9.
Kelly CP, Pothoulakis C, LaMont JT. Clostridium difficile colitis. N Engl J Med. 1994;330:257–262. doi:10.1056/NEJM199401273300406.
Ananthakrishnan AN, McGinley EL, Binion DG. Excess hospitalization burden associated with Clostridium difficile in patients with Inflammatory Bowel Disease. Gut. 2007 [Epub ahead of print].
Issa M, Vijayapal A, Graham MB, et al. Impact of Clostridium difficile on inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007;5(3):345–351. doi:10.1016/j.cgh.2006.12.028.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jodorkovsky, D., Young, Y. & Abreu, M.T. Clinical Outcomes of Patients with Ulcerative Colitis and Co-existing Clostridium difficile Infection. Dig Dis Sci 55, 415–420 (2010). https://doi.org/10.1007/s10620-009-0749-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0749-9