Abstract
Few studies have explored the importance of worry-related metacognitions and thought control strategies in major depressive disorder. The present study explored how metacognitions and thought control strategies differentiated currently depressed (n = 37), previously depressed (n = 81) and never-depressed individuals (n = 50). Discriminant function analysis was performed to investigate group differences on the Metacognitions Questionnaire-30, Thought Control Questionnaire, and Ruminative Response Scale. The analysis revealed that currently depressed participants scored significantly higher than previously depressed participants and that previously depressed participants scored higher than never-depressed participants on negative metacognitive beliefs, rumination, worry and the use of punishment as a thought control strategy. The discriminant function analysis further showed that previously depressed participants had a higher use of the thought control strategy reappraisal, along with lower dysfunctional metacognitions concerning the need to control their thoughts, higher confidence in their cognitive function and lower levels about the need to worry, compared to both the currently and never-depressed groups. The results indicate that metacognitions and thought control strategies could be promising vulnerability markers for depression.

Similar content being viewed by others
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
Andrade, L., Caraveo-Anduaga, J. J., Berglund, P., Bijl, R. V., De Graaf, R., Vollebergh, W., et al. (2003). The epidemiology of major depressive episodes: Results from the international consortium of psychiatric epidemiology (ICPE) surveys. International Journal of Methods in Psychiatric Research, 12, 3–21.
Beck, A. T. (1987). Cognitive models of depression. Journal of Cognitive Psychotherapy, 1, 5–37.
Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression. New York: Guilford Press.
Beck, A. T., & Steer, R. A. (1990). Manual for the Beck Anxiety Inventory. San Antonio, TX: The Psychological Corporation.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). BDI-II: Beck Depression Inventory (2nd ed.). San Antonio, TX: The Psychological Corporation.
Beevers, C. G., Rohde, P., Stice, E., & Nolen-Hoeksema, S. (2007). Recovery from major depressive disorder among female adolescents: A prospective test of scar hypothesis. Journal of Consulting and Clinical Psychology, 75, 888–900.
DeRubeis, R. K., Hollon, S. D., Amsterdam, J. D., Shelton, R. C., Young, P. R., Salamon, R. M., et al. (2005). Cognitive therapy vs medications in the treatment of moderate to severe depression. Archives of General Psychiatry, 62, 409–416.
Dimidjian, S., Hollon, S. D., Dobson, K. S., Schmaling, K. B., Kohlenberg, R. J., Addis, M. E., et al. (2006). Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology, 74, 658–670.
Fehm, L., & Hoyer, J. (2004). Measuring thought control strategies: The Thought Control Questionnaire and a look beyond. Cognitive Therapy and Research, 28, 105–117.
Fergus, T. A., Bardeen, J. R., & Orcutt, H. K. (2012). Attentional control moderates the relationship between activation of the cognitive attentional syndrome and symptoms of psychopathology. Personality and Individual Differences, 53, 213–217.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (1997). The structured clinical interview for DSM-IV, axis I disorders-clinician version (SCID-CV). Washington, DC: American Psychiatric Press.
Halvorsen, M., Høifødt, R. S., Myrbakk, I. N., Wang, C. E. A., Sundet, K., Eisemann, M., et al. (2012). Cognitive function in unipolar major depression: A comparison of clinically depressed, previously depressed and never depressed individuals. Journal of Clinical and Experimental Neuropsychology, 34, 782–790.
Halvorsen, M., Wang, C. E., Eisemann, M., & Waterloo, K. (2010). Dysfunctional attitudes and early maladaptive schemas as predictors of depression: A 9-year follow-up study. Cognitive Therapy and Research, 34, 368–379.
Halvorsen, M., Wang, C. E., Richter, J., Myrland, I., Pedersen, S. K., Eisemann, M., et al. (2009). Early maladaptive schemas, temperament and character traits in clinically depressed and previously depressed subjects. Clinical Psychology & Psychotherapy, 16, 394–407.
Halvorsen, M., Waterloo, K., Sundet, K. S., Eisemann, M., & Wang, C. E. A. (2011). Verbal learning and memory in depression: A 9-year follow-up study. Psychiatry Research, 188, 350–354.
Hjemdal, O., Stiles, T. C., & Wells, A. (2013). Automatic thoughts and meta-cognition as predictors of depressive and anxious symptoms: A prospective study of two trajectories. Scandinavian Journal of Psychology, 54, 59–65.
IBM Corp. (2012). IBM SPSS statistics for Windows, version 21.0. Armonk, NY: IBM Corp.
Ingram, R., Miranda, J., & Segal, Z. V. (1998). Cognitive vulnerability to depression. New York: Guilford Press.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Koretz, D., Merikangas, K. R., et al. (2003). The epidemiology of major depressive disorder: Results from the national comorbidity survey replication (NCS-R). Journal of the American Medical Association, 289, 3095–3105.
Lam, D., Smith, S., Checkley, S., Rijsdijk, F., & Sham, P. (2003). Effect of neuroticism, response style and information processing on depression severity in a clinically depressed sample. Psychological Medicine, 33, 469–479.
Lewinsohn, P. M., Steinmetz, J. L., Larson, D. W., & Franklin, J. (1981). Depression-related cognitions: Antecedent or consequence? Journal of Abnormal Psychology, 90, 213–219.
Luciano, J. V., Belloch, A., Algarabel, S., Tomas, J. M., Morillo, C., & Lucero, M. (2006). Confirmatory factor analysis of the White Bear Suppression Inventory and the Thought Control Questionnaire: A comparison of alternative model. European Journal of Psychological Assessment, 22, 250–258.
Luminet, O. (2004). Measurement of depressive rumination and associated constructs. In C. Papageorgiou & A. Wells (Eds.), Depressive rumination: Nature, theory and treatment (pp. 187–215). West Sussex: Wiley.
Nolen-Hoeksema, S., & Morrow, J. (1991). A prospective study of depression and posttraumatic stress symptoms after a natural disaster. The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology, 61, 115–121.
Nolen-Hoeksema, S., Parker, L. E., & Larson, J. (1994). Ruminative coping with depressed mood following loss. Journal of Personality and Social Psychology, 67, 92–104.
Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking Rumination. Perspectives of Psychological Science, 5, 400–424.
Papageorgiou, C., & Wells, A. (2001). Metacognitive beliefs about rumination in recurrent major depression. Cognitive and Behavioral Practice, 8, 160–164.
Papageorgiou, C., & Wells, A. (2003). An empirical test of a clinical metacognitive model of rumination and depression. Cognitive Therapy and Research, 27, 261–273.
Papageorgiou, C., & Wells, A. (2009). A prospective test of the clinical metacognitive model of rumination and depression. International Journal of Cognitive Therapy, 2, 123–131.
Rassin, E., & Diepstraten, P. (2003). How to suppress obsessive thoughts. Behaviour Research and Therapy, 41, 97–103.
Reynolds, M., & Wells, A. (1999). The Thought Control Questionnaire: Psychometric properties in a clinical sample, and relationships with PTSD and depression. Psychological Medicine, 29, 1089–1099.
Roth, A., & Fonagy, P. (2005). What works for whom: A critical review of psychotherapy research (2nd ed.). New York, NY: Guilford Publication.
Sarisoy, G., Pazvantoglu, O., Ozturan, D. D., Ay, N. D., Yilman, T., Mor, S., et al. (2013). Metacognitive beliefs in unipolar and bipolar depression: A comparative study. Nordic Journal of Psychiatry. Published online August 1, 2013. doi:10.3109/08039488.2013.814710.
Smith, J. M., & Alloy, L. B. (2009). A roadmap to rumination: A review of the definition, assessment, and conceptualization of this multifaceted construct. Clinical Psychology Review, 29, 116–128.
Spada, M. M., Mohiyeddini, C., & Wells, A. (2008). Measuring metacognitions associated with emotional distress: Factor structure and predictive validity of the Metacognitions Questionnaire 30. Personality and Individual Differences, 45, 238–242.
Steer, R. A., Ball, R., Ranieri, W. F., & Beck, A. T. (1999). Dimensions of the Beck Depression Inventory-II in clinically depressed outpatients. Journal of Clinical Psychology, 55, 117–128.
Steer, R. A., & Ranieri, W. F. (1993). Further evidence for the validity of the Beck Anxiety Inventory with psychiatric outpatients. Journal of Anxiety Disorders, 7, 195–205.
Tabachnick, B. G., & Fidell, L. S. (2007). Using multivariate statistics (5th ed.). Upper Saddle River: Pearson Education.
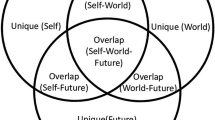
Wang, C. E., Brennen, T., & Holte, A. (2005). Mechanisms of recurrent depression: a cognitive battle model and some preliminary results. Clinical Psychology & Psychotherapy, 12, 427–442.
Wang, C. E., Halvorsen, M., Sundet, K., Steffensen, A. L., Holte, A., & Waterloo, K. (2006). Verbal memory performance of mildly to moderately depressed outpatient younger adults. Journal of Affective Disorders, 92, 283–286.
Wells, A. (2000). Emotional disorders and metacognition. West Sussex: Wiley.
Wells, A. (2009). Metacognitive therapy for anxiety and depression. New York: Guilford Press.
Wells, A., & Carter, K. (2001). Further tests of a cognitive model of generalized anxiety disorder: Metacognitions and worry in GAD, panic disorder, social phobia, depression, and nonpatients. Behavior Therapy, 32, 85–102.
Wells, A., & Cartwright-Hatton, S. (2004). A short form of the metacognitions questionnaire: properties of the MCQ-30. Behaviour Research and Therapy, 42, 385–396.
Wells, A., & Davies, M. I. (1994). The Thought Control Questionnaire: A measure of individual differences in the control of unwanted thoughts. Behaviour Research and Therapy, 32, 871–878.
Wells, A., & Matthews, G. (1994). Attention and emotion: A clinical perspective. Hove: Erlbaum.
Wells, A., & Matthews, G. (1996). Modeling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy, 32, 867–870.
Wells, A., & Pagageorgiou, C. (2004). Metacognitive therapy for depressive rumination. In C. Papageorgiou & A. Wells (Eds.), Depressive rumination: Nature, theory and treatment (pp. 259–273). West Sussex: Wiley.
Acknowledgments
This study was supported by “The National Program for Integrated Clinical Specialist and PhD-training for Psychologists” in Norway. This program is a joint cooperation between the Universities of Bergen, Oslo, Tromsø, the Norwegian University of Science and Technology (Trondheim), the Regional Health Authorities, and the Norwegian Psychological Association. The program is funded jointly by The Ministry of Education and Research and The Ministry of Health and Care Services. The study was also supported in part by the Psychiatric Research Centre of Northern Norway. The authors would like to thank the participants and the research assistants who contributed to the data collection. We would also like to thank Professor Adrian Wells for commenting on an early draft of the manuscript. Last but not least, we would like to thank the anonymous reviewers for helpful suggestions, which contributed to the improvement of this paper.
Conflict of Interest
Marianne Halvorsen, Roger Hagen, Odin Hjemdal, Marianne S. Eriksen, Åse J. Sørli, Knut Waterloo, Martin Eisemann and Catharina E. A. Wang do not have any commercial association that might pose a conflict of interest in connection with the manuscript.
Informed Consent
All of the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients before entering the study.
Animal Rights
No animal studies were carried out by the authors for this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Halvorsen, M., Hagen, R., Hjemdal, O. et al. Metacognitions and Thought Control Strategies in Unipolar Major Depression: A Comparison of Currently Depressed, Previously Depressed, and Never-Depressed Individuals. Cogn Ther Res 39, 31–40 (2015). https://doi.org/10.1007/s10608-014-9638-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-014-9638-4