Abstract
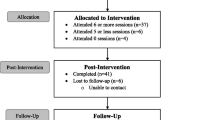
A package of biopsychosocial services for young adults experiencing psychological distress was evaluated and compared to usual outpatient psychiatric care. Young adults (18–25) with moderate-to-severe symptoms of depression and/or anxiety (n = 26) were enrolled in a 13-week intervention consisting of nutritional coaching and multi-vitamin supplements, weekly educational and peer support groups, and a modest financial stipend to engage with physical or expressive activities. A comparison group (n = 13) continued with their usual medication-based outpatient care. Program participants reported significantly improved depression, anxiety, severity of distress, overall quality of life, and empowerment over 4 months, with progress maintained or further improved at 2-month follow-up. No evidence of change on any outcome was observed for comparison group participants. Although long-term impacts on mental health trajectories and reliance on psychotropic medications remain unknown, a holistic self-learning approach is a viable alternative to standard outpatient psychiatric care for young adults.

Similar content being viewed by others
References
Adame, A., & Knudson, R. (2007). Beyond the counter-narrative: Exploring alternative narratives of recovery from the psychiatric survivor movement. Narrative Inquiry, 17(2), 157–178.
Akkasheh, G., Kashani-Poor, Z., Tajabadi-Ebrahimi, M., Jafari, P., & Akbari, H. (2016). Clinical and metabolic response to probiotic administration in patients with major depressive disorder: A randomized, double-blind, placebo-controlled trial. Nutrition, 32(3), 315–320. https://doi.org/10.1016/j.nut.2015.09.003.
Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15-4927, NSDUH Series H-50). (2015). Center for Behavioral Health Statistics and Quality. Retrieved from https://www.samhsa.gov/data/.
Bonomi, A., Patrick, D., Bushnell, D., & Martin, M. (2000). Validation of the United States' version of the World Health Organization Quality of Life (WHOQOL) instrument. Journal of Clinical Epidemiology, 53(1), 13–17.
Chatterjee, H., Camic, P., Lockyer, B., & Thomson, L. (2017). Non-clinical community interventions: A systematised review of social prescribing schemes. Arts & Health, 10, 97–123. https://doi.org/10.1080/17533015.2017.1334002.
Coatsworth, J. D., Palen, L., Sharp, E., & Ferrer-Wreder, L. (2006). Self-defining activities, expressive identity, and adolescent wellness. Applied Developmental Science, 10(3), 157–170. https://doi.org/10.1207/s1532480xads1003_5.
Cruickshank, G., MacGillivray, S., & Bruce, D. (2008). Cross-sectional survey of patients in receipt of long-term repeat prescriptions for antidepressant drugs in primary care. Mental Health in Family Medicine, 5, 105–109.
Davies, J., & Read, J. (2019). A systematic review into the incidence, severity, and duration of antidepressant withdrawal effects: Are guidelines evidence-based? Addictive Behaviors, 97, 111–121.
De Vries, Y., Roest, A., Beijers, L., Turner, E., & de Jonge, P. (2016). Bias in the reporting of harms in clinical trials of second-generation antidepressants for depression and anxiety: A meta-analysis. European Neuropsychopharmacology, 26(11), 1752–1759.
Faulkner, A. (2017). Survivor research and Mad Studies: The role and value of experiential knowledge in mental health research. Disability & Society, 32(4), 500–520. https://doi.org/10.1080/09687599.2017.1302320.
Faulkner, A., & Basset, T. (2010). A helping hand: Consultations with services users about peer support. Retrieved from https://www.together-uk.org/wp-content/uploads/downloads/2011/11/helpinghand.pdf.
Gambrill, E. (2014). The Diagnostic and Statistical Manual of Mental Disorders as a major form of dehumanization in the modern world. Research on Social Work Practice, 24(1), 13–36. https://doi.org/10.1177/1049731513499411.
Hickie, I., Luscombe, G., Davenport, T., Burns, J., & Highet, N. (2007). Perspectives of young people on depression: Awareness, experiences, attitudes, and treatment preferences. Early Intervention in Psychiatry, 1, 333–339. https://doi.org/10.1111/j.1751-7893.2007.00042.x.
Hughes, S., Cohen, D., & Jaggi, R. (2014). Differences in reporting serious adverse events in industry sponsored clinical trial registries and journal articles on antidepressant and antipsychotic drugs: A cross-sectional study. British Medical Journal Open, 4, e005535.
Hughes, S., Colbert, R., & Baugh, A. (2020). Valuing whole complex lives: Young adults’ experiences of recovery-related principles in mental health care in the United States. Health and Social Care in the Community, 28, 357–365. https://doi.org/10.1111/hsc.12867
Hughes, S., Colbert, R., Holloway, M., Klumb, K., Van Sweden, A., & Fiushbein, L. (2018). Consciousness-raising workbook for re-telling the story of ourselves. Learning and Self-development Collaborative. The Nowak Society. Fort Collins, CO. Retrieved from https://www.chhs.colostate.edu/ssw/research/alternatives-for-mental-health-and-healing-lab/learning-and-self-development-collaborative/.
Jacka, F., O'Neil, A., Opie, R., Itsiopoulos, C., Cotton, S., Mohebbi, M., et al. (2017). A randomised controlled trial of dietary improvement for adults with major depression (the 'SMILES' trial). BMC Medicine, 15(1), 23. https://doi.org/10.1186/s12916-017-0791-y.
Khan, A., Faucett, J., Lichtenberg, P., Kirsch, I., & Brown, W. (2012). A systematic review of comparative efficacy of treatments and controls for depression. PLoS ONE, 7(7), e41778.
Lee, R., Draper, M., & Lee, S. (2001). Social connectedness, dysfunctional interpersonal behaviors, and psychological distress: Testing a mediator model. Journal of Counseling Psychology, 48(3), 310–318.
Lipson, S., Lattie, E., & Eisenberg, D. (2019). Increased rates of mental health service utilization by U.S. college students: 10-year population-level trends (2007–2017). Psychiatric Services, 70, 60–63. https://doi.org/10.1176/appi.ps.201800332.
Mallett, C. (2014). Child and adolescent behaviorally based disorders: A critical review of reliability and validity. Research on Social Work Practice, 24, 96–113. https://doi.org/10.1177/1049731512464275.
Marcus, M., Westra, H., Eastwood, J., & Barnes, K. (2012). What are young adults saying about mental health? An analysis of internet blogs. Journal of Medical Internet Research, 14(1), e17. https://doi.org/10.2196/jmir.1868.
McCann, T., & Lubman, D. (2012). Young people with depression and their satisfaction with the quality of care they receive from a primary care youth mental health service: A qualitative study. Journal of Clinical Nursing, 21, 2179–2187. https://doi.org/10.1111/j.1365-2702.2012.04086.x.
Meade, S., & Hilton, D. (2003). Crisis and connection. Psychiatric Rehabilitation Journal, 27(1), 87–94.
Mojtabai, R., & Olfson, M. (2014). National trends in long-term use of antidepressant medications: Results from the USA National Health and Nutrition Examination Study. Journal of Clinical Psychiatry, 75(2), 169–177.
Opie, R., O'Neil, A., Jacka, F., Pizzinga, J., & Itsiopoulos, C. (2017). A modified Mediterranean dietary intervention for adults with major depression: Dietary protocol and feasibility data from the SMILES trial. Nutritional Neuroscience, 19, 1–15.
Pinheiro, J. (2016). R Core Team (2016) nlme: Linear and nonlinear mixed effects models. R package version 3.1-128. Bioinformatics, 26, 1463–1464.
Pratt, L., Brody, D., & Gu, Q. (2017). Antidepressant use among persons aged 12 and over: United States, 2011–2014. Hyattsville, MD: National Center for Health Statistics.
Raue, P., Schulberg, H., Heo, M., Klimstra, S., & Bruce, M. (2009). Patients' depression treatment preferences and initiation, adherence, and outcome: A randomized primary care study. Psychiatric Services, 60, 337–343. https://doi.org/10.1176/appi.ps.60.3.337.
Read, J., Cartwright, C., & Gibson, K. (2014). Adverse emotional and interpersonal effects reported by 1829 New Zealanders while taking antidepressants. Psychiatry and Research, 216(1), 67–73.
Rogers, E., Ralph, R., & Salzer, M. (2010). Validating the empowerment scale with a multisite sample of consumers of mental health services. Psychiatric Services, 61(9), 933–936.
Rucklidge, J., Kaplan, B., & Mulder, R. (2015). What if nutrients could treat mental illness? Australian and New Zealand Journal of Psychiatry, 49(5), 407–408. https://doi.org/10.1177/0004867414565482.
Seebohm, P., Chaudhary, S., Boyce, M., Elkan, R., Avis, M., & Mucc-Giddings, C. (2013). The contribution of self-help/mutual aid groups to mental well-being. Health and Social Care in the Community, 21(4), 391–401. https://doi.org/10.1111/hsc.12021.
Semahegn, A., Torpey, K., Manu, A., Assefa, N., Tesfaye, G., & Ankomah, A. (2020). Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: A systematic review and meta-analysis. Systematic Reviews, 9, 17.
Stratford, A., Halpin, M., Phillips, K., Skerritt, F., Beales, A., Cheng, V., et al. (2017). The growth of peer support: An intentional charter. Journal of Mental Health. https://doi.org/10.1080/09638237.2017.1340593.
Tew, J., Ramon, S., Slade, M., Bird, V., Melton, J., & Le Boutillier, C. (2012). Social factors and recovery from mental health difficulties: A review of the evidence. British Journal of Social Work, 42, 443–460. https://doi.org/10.1093/bjsw/bcr076.
Thomas, D. (2006). A general inductive approach for analyzing qualitative evaluation data. American Journal of Evaluation, 27(2), 237–246.
Treatment, C. F. S. A. (1994). Simple Screening Instruments for Outreach for Alcohol and Other Drug Abuse and Infectious Diseases (DHHS Publication No. SMA 94-2094, Treatment Improvement Protocol Series 11). Rockville, MD: Substance Abuse and Mental Health Services Administration.
Twenge, J., Cooper, A., Joiner, T., Duffy, M., & Binau, S. (2019). Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. Journal of Abnormal Psychology, 128(3), 158–199.
Valles-Colomer, M., Falony, G., Darzi, Y., Tigchelaar, E., Wang, J., Tito, R., et al. (2019). The neuroactive potential of the human gut microbiota in quality of life and depression. Nature Microbiology, 4, 623–632.
Warden, D., Trivedi, M., Wisniewski, S., Davis, L., Nierenberg, A., et al. (2007). Predictors of attrition during initial (citalopram) treatment for depression: A STAR*D report. American Journal of Psychiatry, 164(8), 1189–1197.
Funding
This study was funded by the Foundation for Excellence in Mental Health Care. Vitamin supplements used in this study were donated by Hardy Nutritionals. Fish oil used in this study was donated by Vital Nutrients.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hughes, S., Rondeau, M., Shannon, S. et al. A Holistic Self-learning Approach for Young Adult Depression and Anxiety Compared to Medication-Based Treatment-As-Usual. Community Ment Health J 57, 392–402 (2021). https://doi.org/10.1007/s10597-020-00666-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-020-00666-9