Abstract
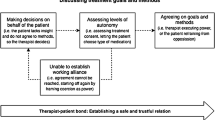
The emphasis on care in the community in current mental health policy poses challenges for community mental health professionals with responsibility for patients who do not wish to receive services. Previous studies report that professionals employ a range of behaviors to influence reluctant patients. We investigated professionals’ own conceptualizations of such influencing behaviors through focus groups with community teams in England. Participants perceived that good, trusting relationships are a prerequisite to the negotiation of reciprocal agreements that, in turn, lead to patient-centred care. They described that although asserting professional authority sometimes is necessary, it can be a potential threat to relationships. Balancing potentially conflicting processes—one based on reciprocity and the other on authority—represents a challenge in clinical practice. By providing descriptive accounts of micro-level dynamics of clinical encounters, our analysis shows how the authoritative aspect of the professional role has the potential to undermine therapeutic interactions with reluctant patients. We argue that such micro-level analyses are necessary to enhance our understanding of how patient-centered mental health policy may be implemented through clinical practice.
Similar content being viewed by others
Notes
For simplicity, we use ‘mental health professionals’ in this article to refer to all those working thereputically with patients in community teams whether or not they are clinicians or have received specific professional training. Where relevant, we refer to specific professions.
References
Anderson, E., Levine, M., Sharma, A., Ferretti, L., Steinberg, K., & Wallach, L. (1993). Coercive use of mandatory reporting in therapeutic relationships. Behavioral Sciences and the Law, 11, 335–345. doi:10.1002/bsl.2370110310.
Angell, B. (2006). Measuring strategies used by mental health providers to encourage medication adherence. Journal of Behaviour Health Services and Research, 33(1), 53–72. doi:10.1007/s11414-005-9000-4.
Angell, B., & Mahoney, C. (2007). Reconceptualizing the case management relationship in intensive treatment: A study of staff perceptions and experiences. Administration and Policy in Mental Health and Mental Health Services Research, 34(2), 172–188. doi:10.1007/s10488-006-0094-7.
Angell, B., Mahoney, C. A., & Martinez, N. I. (2006). Promoting treatment adherence in assertive outreach treatment. Social Service Review, 80(3), 486–526. doi:10.1086/505447.
Anthony, W. A. (1993). Recovery from mental illness: The guiding vision of the mental health system in the 1990s. Psychosocial Rehabilitation Journal, 16(4), 11–23.
Appelbaum, P., & Le Melle, S. (2007). Techniques used by assertive community treatment (ACT) teams to encourage adherence: Patient and staff perspectives. Community Mental Health Journal, 44, 49–464. doi:10.1007/s10598-008-9149-4.
Appelbaum, P. S., & Redlich, A. (2006). Use of leverage over patients’ money to promote adherence to psychiatric treatment. The Journal of Nervous and Mental Disease, 194(4), 294–302. doi:10.1097/01.nmd.0000207368.14133.0c.
Atlas.ti. (1999). ATLAS.ti 6.2. Berlin: Scientific Software Development.
Burns, T. (2004). Community mental health teams. Oxford: Oxford University Press.
Burns, T., & Firn, M. (2002). Assertive outreach in mental health: A manual for practitioners. Oxford: Oxford University Press.
Burns, T., Yeeles, K., Molodynski, A., Nightingale, H., Vazquez-Montes, M., Sheehan, K., et al. (2011). Pressure to adhere to treatment (‘leverage’) in English mental healthcare. British Journal of Psychiatry, 199, 145–150. doi:10.1192/bjp.bp.110.086827.
Canvin, C., Rugkåsa, J., Sinclair, J., & Burns, T. (2013). Leverage and other informal pressures in community psychiatry in England. International Journal of Law and Psychiatry, 36, 100–106. doi:10.1016/j.ijlp.2013.01.002.
Classen, D., Fakhoury, W., Ford, R., & Priebe, S. (2007). Money for medication: Financial incentives to improve medication adherence in assertive outreach. Psychiatric Bulletin, 31, 4–7. doi:10.1192/pb.31.1.4.
Curtis, L., & Hodge, M. (1995). Ethics and boundaries in community support services: New challenges. New Directions for Mental Health Services, 66, 43–59.
Davies, S. (2002). Autonomy versus coercion: Reconciling competing perspectives in community mental health. Community Mental Health Journal, 38(3), 239–250.
Denzin, N. K., & Lincoln, Y. S. (Eds.). (1993). Handbook of qualitative research. Thousands Oaks: Sage.
Department of Health. (2009). New horizons: A shared vision for mental health. London: Department of Health.
Department of Health. (2011). No health without mental health: A cross-government mental health outcomes strategy for people of all ages. London: Department of Health.
Elbogen, E. B., Swanson, J. W., & Swartz, M. S. (2003). Psychiatric disability, the use of financial leverage and perceived coercion in mental health services. International Journal of Forensic Mental Health, 2(2), 119–127. doi:10.1080/14999013.2003.10471183.
Gardener, W., & Lidz, C. (2001). Gratitude and coercion between physicians and patients. Psychiatric Annuals, 31(2), 125–129.
Gillard, S., Simons, L., Lucock, M., & Edwards, C. (2012). Patient and public involvement in the coproduction of knowledge: Reflection on the analysis of qualitative data in a mental health study. Qualitative Health Research, 22(8), 1126–1137. doi:10.1177/1049732312448541.
Glaser, B. G. (1965). The constant comparative method of qualitative analysis. Social Problems, 12(4), 436–445. doi:10.2307/798843.
Gray, R., Wykes, T., & Gournay, K. (2002). From compliance to concordance: A review of the literature on interventions to enhance compliance with antipsychotic medication. Journal of Psychiatric and Mental Health Nursing, 9, 277–284. doi:10.1046/j.1365-2850.2002.00474.x.
Jaeger, M., & Rossler, W. (2010). Enhancement of outpatient treatment adherence: Patient’s perception of coercion, fairness and effectiveness. Psychiatry Research, 180, 48–53. doi:10.1016/j.psychres.2009.09.011.
Kirsh, B., & Tate, E. (2006). Developing a comprehensive understanding of the working alliance in community mental health. Qualitative Health Research, 16(8), 1054–1074. doi:10.1177/1049732306292100.
Kitzinger, J. (2005). Focus group research: Using group dynamics to explore perceptions, experiences and understandings. In I. Holloway (Ed.), Qualitative research in health care (pp. 56–69). Maidenhead: Open University Press.
Korman, H., Engster, D., & Milstein, B. M. (1996). Housing as a tool of coercion. In D. L. Dennis & J. Monahan (Eds.), Coercion and aggressive community treatment: A new frontier in mental health law (pp. 95–113). New York: Plenum.
Laugharne, R., Priebe, S., McCabe, R., Garland, N., & Clifford, D. (2012). Trust, choice and power in mental health care: Experiences of patients with psychosis. International Journal of Social Psychiatry, 58(5), 496–504. doi:10.1177/0020764011408658.
Lingam, R., & Scott, J. (2002). Treatment and non-adherence in affective disorders. Acta Psychiatrica Scandinavica, 105, 164–172. doi:10.1034/j.1600-0447.2002.1r084.x.
Lopez, M. (1996). The perils of outreach work: Overreaching the limits of persuasive tactics. In D. L. Dennis & J. Monahan (Eds.), Coercion and aggressive community treatment: A new frontier in mental health law (pp. 85–92). New York: Plenum.
Lützén, K. (1998). Subtle coercion in psychiatric practice. Journal of Psychiatric and Mental Health Nursing, 5, 101–107. doi:10.1046/j.1365-2850.1998.00104.x.
Magnusson, A., & Severinsson, E. (2004). Swedish mental health nurses’ responsibility in supervised community care of persons with long-term mental illness. Nursing and Health Sciences, 6, 19–27. doi:10.1111/j.1442-2018.2003.00171.x.
Malinowski, B. (1978 [1922]). Argonauts of the Western Pacific. London: Routledge.
Mauss, M. (1990[1922]). The gift: Forms and functions of exchange in archaic societies. London: Routledge.
Mind. (2008). Life and times of a supermodel. The recovery paradigm for mental health. London: Mind.
Monahan, J., Redlich, A. D., Swanson, J., Robbins, P. C., Appelbaum, P. S., Petrila, J., et al. (2005). Use of leverage to improve adherence to psychiatric treatment in the community. Psychiatric Services, 56(1), 37–44. doi:10.1176/appi.ps.56.1.37.
Moser, L. (2007). Coercion in assertive community treatment: Examining client, staff, and program predictors. PhD Thesis. Purdue University, Indiana. http://search.proquest.com/docview/304834899?accountid=31375. Accessed October 3, 2012.
Moser, L., & Bond, G. (2009). Scope of agency control: Assertive community treatment teams’ supervision of consumers. Psychiatric Services, 60(7), 922–928.
Nath, S. B., Alexander, L. B., & Solomon, P. L. (2012). Case managers’ perspectives on the therapeutic alliance: A qualitative study. Social Psychiatry and Psychiatric Epidemiology,. doi:10.1007/s00127-012-0483-z.
Neale, M., & Rosenheck, R. A. (2000). Therapeutic limit setting in an assertive outreach treatment programme. Psychiatric Services, 51(4), 499–505.
Nicholson, J. (2005). Use of child custody as leverage to improve treatment adherence. Psychiatric Services, 56, 357–358. doi:10.1176/appi.ps.56.3.357-a.
Olofson, B., & Norberg, A. (2001). Experiences of coercion in psychiatric care as narrated by patients, nurses and physicians. Journal of Advanced Nursing, 33(1), 89–97. doi:10.1046/j.1365-2648.2001.01641.x.
Olofsson, B., Norberg, A., & Jacobsson, L. (1995). Nurses’ experience of using force in institutional care of psychiatric patients. Nordic Journal of Psychiatry, 49, 325–330.
Øye, C. (2010). Omsorgens vilkår: Om gaver og tjenester som del av relasjonsdannelsen in institusjonspsykiatrien når brukermedvirkning skal vektlegges (The conditions of care: On the use of gifts and services as part of relationship building in inpatient psychiatry when user involvement is emphasised). Michael, 2, 218–233.
Redlich, A. D., Steadman, H. J., Robbins, P. C., & Swanson, J. (2006). Use of the criminal justice system to leverage mental health treatment: Effects of treatment adherence and satisfaction. Journal of the American Academy of Psychiatry Law, 34, 292–299.
Robbins, P., Petrila, J., Le Melle, S., & Monahan, J. (2006). The use of housing as leverage to increase adherence to psychiatric treatment in the community. Administration and Policy in Mental Health and Mental Health Services Research, 33(2), 226–236. doi:10.1007/s10488-006-0037-3.
Rugkåsa, J., & Burns, T. (2009). Community treatment orders. Psychiatry, 8(2), 493–495. doi:10.1016/j.mppsy.2009.09.009.
Seale, C., Chaplin, R., Lelleiott, P., & Quirk, A. (2005). Sharing decisions in consultations involving anti-psychotic medication: A qualitative study of psychiatrist’ experiences. Social Science and Medicine, 62(11), 2861–2873. doi:10.1016/j.socscimed.2005.11.002.
Shepherd, G., Boardman, J., & Slade, M. (2009). Making recovery a reality. Briefing Paper. London: Sainsbury Centre for Mental Health.
Simmel, G. (1950 [1908]). In K. H. Wolff (Transl. and Ed.), The Sociology of Georg Simmel. New York: The Free Press.
Sjöström, S. (2005). Invocation of coercion in compliance communication—Power dynamics in psychiatric care. International Journal of Law and Psychiatry, 29, 36–47. doi:10.1016/j.ijlp.2005.06.001.
Sjöström, S., Zetterberg, L., & Markström, U. (2011). Why community compulsion became the solution—Reforming mental health law in Sweden. International Journal of Law and Psychiatry, 34(6), 419–428. doi:10.1016/j.ijlp.2011.10.007.
Smart, C. (2007). Personal life. New directions in sociological thinking. London: Polity Press.
Solomon, P. (1996). Research on the coercion of persons with severe mental illness. In D. L. Dennis & J. Monahan (Eds.), Coercion and aggressive community treatment: A new frontier in mental health law (pp. 129–145). New York: Plenum.
Stanhope, V., Marcus, S., & Solomon, P. (2009). The impact of coercion on service from the perspective of mental health care consumers with co-occurring disorders. Psychiatric Services, 60(2), 183–188.
Stanhope, V., & Matejkowski, J. (2010). Understanding the role of individual consumer–provider relationships within assertive community treatment. Community Mental Health Journal, 46, 309–318. doi:10.1007/s10597-099-9219-2.
Steadman, H. J., Gounis, K., Dennis, D., Hopper, K., Roche, B., Swartz, M., et al. (2001). Assessing the New York involuntary outpatient commitment pilot programme. Psychiatric Services, 52, 330–336. doi:10.1176/appi.ps.52.3.330.
Susser, E., & Roche, B. (1996). “Coercion” and leverage in clinical outreach. In D. L. Dennis & J. Monahan (Eds.), Coercion and aggressive community treatment: A new frontier in mental health law (pp. 73–84). New York: Plenum.
Swartz, M. S., & Swanson, J. (2008). Outpatient commitment: When it improves patient outcomes. Current Psychology, 7(4), 25–35.
Swartz, M. S., Swanson, J. W., & Hannon, M. J. (2003). Does fear of coercion keep people away from mental health treatment? Evidence from a survey of persons with schizophrenia and mental health professionals. Behavioral Sciences and the Law, 21, 459–472. doi:10.1002/bsl.539.
Swartz, M. S., Swanson, J. W., Wagner, H. R., Burns, B. J., Hiday, V. A., & Borum, R. (1999). Can involuntary outpatient commitment reduce hospital recidivism? Findings from a randomized trial with severely mentally ill individuals. American Journal of Psychiatry, 156, 1968–1975.
Swartz, M. S., Wagner, H. J., Swanson, J. W., Hiday, V. A., & Burns, B. J. (2002). The perceived coerciveness of involuntary outpatient commitment: Findings from an experimental study. Journal of the American Academy of Psychiatry Law, 30, 207–217.
Szmukler, G., & Appelbaum, P. (2008). Treatment pressures, leverage, coercion, and compulsion in mental health care. Journal of Mental Health, 17(3), 233–244. doi:10.1080/09638230802052203.
Van Dorn, R. A., Elbogen, E. B., Redlich, A. D., Swanson, J. W., Swartz, M. S., & Mustillo, S. (2006). The relationship between mandated community treatment and perceived barriers to care in persons with severe mental illness. International Journal of Law and Psychiatry, 29(6), 495–506. doi:10.1016/j.ijlp.2006.08.002.
Zygmunt, A., Olofson, M., Boyer, C. A., & Mechanic, D. (2002). Interventions to improve medication adherence in schizophrenia. American Journal of Psychiatry, 159, 1653–1664. doi:10.1176/appi.ajp.159.10.1653.
Acknowledgments
We thank our focus group participants for making this study possible. This article presents independent research funded by the National Institute of Health Research (Program Grant for Applied Research, Grant Number RP-PG-0606-1006). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rugkåsa, J., Canvin, K., Sinclair, J. et al. Trust, Deals and Authority: Community Mental Health Professionals’ Experiences of Influencing Reluctant Patients. Community Ment Health J 50, 886–895 (2014). https://doi.org/10.1007/s10597-014-9720-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-014-9720-0