ABSTRACT
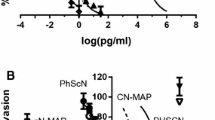
Primary tumors often give rise to disseminated tumor cells (DTC’s), which acquire full malignancy after invading distant site(s). Thus, DTC’s may be a productive target for preventing prostate cancer metastasis progression. Our prior research showed that PHSCN peptide (Ac-PHSCN-NH2) targets activated α5β1 integrin to prevent invasion and metastasis in preclinical adenocarcinoma models, and disease progression in Phase I clinical trial. Here, we report that d-stereoisomer replacement of histidine and cysteine in PHSCN produces a highly potent derivative, Ac-PhScN-NH2 (PhScN). PhScN was 27,000- to 150,000-fold more potent as an inhibitor of basement membrane invasion by DU 145 and PC-3 prostate cancer cells. A large increase in invasion–inhibitory potency occurred after covalent modification of the sulfhydryl group in PHSCN to prevent disulfide bond formation; while the potency of covalently modified PhScN was not significantly increased. Thus PhScN and PHSCN invasion inhibition occurs by a noncovalent mechanism. These peptides also displayed similar cell surface binding dissociation constants (Kd), and competed for the same site. Consistent with its increased invasion–inhibitory potency, PhScN was also a highly potent inhibitor of lung extravasation and colonization in athymic nude mice: it was several hundred- or several thousand-fold more potent than PHSCN at blocking extravasation by PC-3 or DU 145 cells, and 111,000- or 379,000-fold more potent at inhibiting lung colonization, respectively. Furthermore, systemic 5 mg/kg PhScN monotherapy was sufficient to cause complete regression of established, intramuscular DU 145 tumors. PhScN thus represents a potent new family of therapeutic agents targeting metastasis by DTC’s to prevent parallel progression in prostate cancer.








Similar content being viewed by others
Abbreviations
- SF:
-
Serum–free
- FBS:
-
Fetal bovine serum
- Bio:
-
Biotin
- CI:
-
Combination index
- IC50:
-
Concentration for 50 % inhibition
- DRI:
-
Dose reduction index
- HBSS:
-
Hanks buffered salt solution
- DTC:
-
Disseminated tumor cells
- ELISA:
-
Enzyme–linked immunoabsorbant assay
- DiI:
-
1,1′-dilinoleyl-3,3,3′3′-tetramethylindocarbocyanine perchlorate
- MAP:
-
Multiantigenic peptide
- MAb:
-
Monoclonal antibody
- SEM:
-
Standard error of mean
- O.C.T.:
-
Optimal cutting temperature
- FITC:
-
Fluorescein isothiocyanate
- Me:
-
Methyl
- OAc:
-
Acetyl
- acm:
-
Acetamidomethyl
- μg:
-
Microgram
- ng:
-
Nanogram
- pg:
-
Picogram
- fg:
-
Femtogram
- ag:
-
Attogram
References
Bubendorf L et al (2000) Metastatic patterns of prostate cancer: an autopsy study of 1,589 patients. Hum Pathol 31(5):578–583
Saitoh H et al (1984) Metastatic patterns of prostatic cancer. Correlation between sites and number of organs involved. Cancer 54(12):3078–3084
Livant DL et al (2000) Anti-invasive, antitumorigenic, and antimetastatic activities of the PHSCN sequence in prostate carcinoma. Cancer Res 60(2):309–320
Zeng Z-Z et al (2006) Role of focal adhesion kinase and phosphatidylinositol 3′-kinase in integrin fibronectin receptor-mediated, matrix metalloproteinase-1 dependent invasion by metastatic prostate cancer cells. Cancer Res 66(16):8091–8099
Zeng Z–Z et al (2009) (alpha)5(beta)1 integrin ligand PHSRN induces invasion and (alpha)5 mRNA in endothelial cells to stimulate angiogenesis. Transl Oncol 2:8–20
Donate F et al (2008) Pharmacology of the novel antiangiogenic peptide ATN-161 (Ac-PHSCN-NH2): observation of a U-shaped dose-response curve in several preclinical models of angiogenesis and tumor growth. Clin Cancer Res 14:2137–2144
van Golen KL et al (2002) Suppression of tumor recurrence and metastasis by a combination of the PHSCN sequence and the antiangiogenic compound tetrathiomolybdate in prostate carcinoma. Neoplasia 4(5):373–379
Khalili P et al (2006) A non-RGD-based integrin binding peptide (ATN-161) blocks breast cancer growth and metastasis in vivo. Mol Can Ther 5:2271–2280
Stoeltzing O et al (2003) Inhibition of integrin alpha5beta1 function with a small peptide (ATN-161) plus continuous 5-FU infusion reduces colorectal liver metastases and improves survival in mice. Int J Cancer 104:496–503
Nam JM et al (2010) Breast cancer cells in three-dimensional culture display an enhanced radioresponse after coordinate targeting of integrin alpha5beta1 and fibronectin. Cancer Res 70(13):5238–5248
Cianfrocca ME et al (2006) Phase 1 trial of the antiangiogenic peptide ATN-161 (Ac-PHSCN-NH(2)), a beta integrin antagonist, in patients with solid tumours. Br J Cancer 94(11):1621–1626
Klein CA (2009) Parallel progression of primary tumours and metastases. Nat Rev Cancer 9(4):302–312
Stone KR et al (1978) Isolation of a human prostate carcinoma cell line (DU 145). Int J Cancer 21(3):274–281
Kaighn ME et al (1979) Establishment and characterization of a human prostatic carcinoma cell line (PC-3). Invest Urol 17(1):16–23
Yao H et al (2010) Increased potency of the PHSCN dendrimer as an inhibitor of human prostate cancer cell invasion, extravasation, and lung colony formation. Clin Exp Metastasis 27(3):173–184
Yao H et al (2011) The PHSCN dendrimer as a more potent inhibitor of human breast cancer cell invasion, extravasation, and lung colony formation. Breast Cancer Res Treat 125:363–375
Livant DL et al (2000) The PHSRN sequence induces extracellular matrix invasion and accelerates wound healing in obese diabetic mice. J Clin Invest 105(11):1537–1545
Jia Y et al (2004) Integrin fibronectin receptors in matrix metalloproteinase-1-dependent invasion by breast cancer and mammary epithelial cells. Cancer Res 64(23):8674–8681
Yao H et al (2011) Role of alpha5beta1 integrin upregulation in radiation-induced invasion by human pancreatic cancer cells. Transl Oncol 4(5):282–292
Peled A et al (2000) The chemokine SDF-1 activates the integrins LFA-1, VLA-4, and VLA-5 on immature human CD34(+) cells: role in transendothelial/stromal migration and engraftment of NOD/SCID mice. Blood 95(11):3289–3296
Hulme EC (1992) Centrifugation binding assays. In: Hulme EC (ed) Receptor-Ligand Interactions: A Practical Approach. Oxford University Press, Oxford, pp 235–246
Mould AP et al (1998) Regulation of integrin function: evidence that bivalent-cation-induced conformational changes lead to the unmasking of ligand-binding sites within integrin alpha5 beta1. Biochem J 331(Pt 3):821–828
Motulsky HJ, Neubig RR (2010) Analyzing binding data. Curr Protoc Neurosci Chapter 7: Unit 7.5
Godement P et al (1987) A study in developing visual systems with a new method of staining neurones and their processes in fixed tissue. Development 101(4):697–713
Molnar Z, Blakey D, Bystron I (2006) Tract-tracing in developing systems and in postmortem human material using carbocyanine dyes. In: Záborszky L, Lanciego JL, Wouterlood FG (eds) Neuroanatomical tract-tracing 3: molecules, neurons, and systems, 3rd edn. Springer Science + Business Media Inc, Boston
Collazo A, Bronner-Fraser M, Fraser SE (1993) Vital dye labelling of Xenopus laevis trunk neural crest reveals multipotency and novel pathways of migration. Development 118(2):363–376
Chou TC, Talalay P (1984) Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv Enzyme Regul 22:27–55
Ren H et al (2009) Differential effect of imatinib and synergism of combination treatment with chemotherapeutic agents in malignant glioma cells. Basic Clin Pharmacol Toxicol 104(3):241–252
Cheng Y, Prusoff WH (1973) Relationship between the inhibition constant (K1) and the concentration of inhibitor which causes 50 per cent inhibition (I50) of an enzymatic reaction. Biochem Pharmacol 22(23):3099–3108
Matthews JC (1993) Fundamentals of receptor. Enzyme and transport kinetics. CRC Press Inc, Boca Raton, pp 64–94
Gupta GP, Massague J (2006) Cancer metastasis: building a framework. Cell 127(4):679–695
Pound CR et al (1999) Natural history of progression after PSA elevation following radical prostatectomy. JAMA 281(17):1591–1597
Amling CL et al (2000) Long-term hazard of progression after radical prostatectomy for clinically localized prostate cancer: continued risk of biochemical failure after 5 years. J Urol 164(1):101–105
Thalgott M et al (2013) Detection of circulating tumor cells in different stages of prostate cancer. J Cancer Res Clin Oncol 139(5):755–763
Morgan TM et al (2009) Disseminated tumor cells in prostate cancer patients after radical prostatectomy and without evidence of disease predicts biochemical recurrence. Clin Cancer Res 15(2):677–683
Yamada R, Kera Y (1998) d-amino acid hydrolysing enzymes. EXS 85:145–155
Clevers H (2004) At the crossroads of inflammation and cancer. Cell 118(6):671–674
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420(6917):860–867
Scherer RL, McIntyre JO, Matrisian LM (2008) Imaging matrix metalloproteinases in cancer. Cancer Metastasis Rev 27(4):679–690
Annedi SC et al (2006) Engineering d-amino acid containing novel protease inhibitors using catalytic site architecture. Bioorg Med Chem 14(1):214–236
Friedrich R et al (2008) Structure of a novel thrombin inhibitor with an uncharged D-amino acid as P1 residue. Eur J Med Chem 43(6):1330–1335
Wang J, Rabenstein DL (2006) Interaction of heparin with two synthetic peptides that neutralize the anticoagulant activity of heparin. Biochemistry 45(51):15740–15747
Welch BD et al (2007) Potent D-peptide inhibitors of HIV-1 entry. Proc Natl Acad Sci USA 104(43):16828–16833
Sroka TC, Pennington ME, Cress AE (2006) Synthetic d-amino acid peptide inhibits tumor cell motility on laminin-5. Carcinogenesis 27(9):1748–1757
Acknowledgments
The authors wish to thank Dr. David Ballou and Dr. Eric Carter in the Department of Biological Chemistry, University of Michigan for helpful suggestions in the development and analysis of the binding assays and data. We also wish to thank Dr. Ted Lawrence, Dr. Daniel Hamstra and Dr. Yi Sun in the Department of Radiation Oncology, University of Michigan for providing thoughtful insight to the preparation of this manuscript. This research was supported by the National Institutes of Health, R01 CA119007, “PHSCN Therapies to Prevent Prostate Cancer Progression”, with fiscal assistance from the Office of Technology Transfer, University of Michigan Medical School Office of Research, Ann Arbor, Michigan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Veine, D.M., Yao, H., Stafford, D.R. et al. A d-amino acid containing peptide as a potent, noncovalent inhibitor of α5β1 integrin in human prostate cancer invasion and lung colonization. Clin Exp Metastasis 31, 379–393 (2014). https://doi.org/10.1007/s10585-013-9634-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-013-9634-1