Abstract
Background
Liver disease is associated with increased bleeding risk. The efficacy and safety of direct oral anticoagulants (DOACs) is a subject of contention in atrial fibrillation (AF) patients with liver disease.
Methods
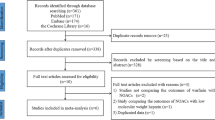
Electronic databases (PubMed, Embase, and Cochrane Library) were searched to retrieve studies on the efficacy and safety of DOACs versus warfarin in AF patients with liver disease from January 1980 to April 2020. A meta-analysis was conducted using a random-effects model.
Results
Six studies involving 41,859 patients were included. Compared with warfarin, DOACs demonstrated significant reduction in ischemic stroke (HR, 0.68; 95% CI (0.54–0.86)), major bleeding (0.74 (0.59–0.92)), and intracranial hemorrhage (ICH) (0.48 (0.40–0.58)), with no significant effect on gastrointestinal bleeding (P = 0.893) in AF patients with liver disease. Similar results were observed in regular-dose, reduced-dose, and active liver disease subgroups, albeit Asian patients had a slight reduction in major bleeding (P = 0.055). Furthermore, the pooled estimates of individual DOAC subgroups indicated that dabigatran and apixaban led to greater safety in major bleeding (P < 0.001), ICH (P < 0.001), and gastrointestinal bleeding (P < 0.005) in these patients. The same trends were observed in AF patients with cirrhosis.
Conclusions
Our findings suggest that DOACs significantly reduce the risk of ischemic stroke, major bleeding, and ICH, with no significant effect on the risk of gastrointestinal bleeding in AF patients with liver disease compared with warfarin.






Similar content being viewed by others
References
Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98(10):946–52.
Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. Jama. 2001;285(18):2370–5.
Fauchier L, Lecoq C, Clementy N, Bernard A, Angoulvant D, Ivanes F, et al. Oral anticoagulation and the risk of stroke or death in patients with atrial fibrillation and one additional stroke risk factor: the Loire Valley Atrial Fibrillation Project. Chest. 2016;149(4):960–8.
Joundi RA, Cipriano LE, Sposato LA, Saposnik G. Ischemic stroke risk in patients with atrial fibrillation and CHA2DS2-VASc score of 1: systematic review and meta-analysis. Stroke. 2016;47(5):1364–7.
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–100.
Gage BF, Yan Y, Milligan PE, Waterman AD, Culverhouse R, Rich MW, et al. Clinical classification schemes for predicting hemorrhage: results from the National Registry of Atrial Fibrillation (NRAF). Am Heart J. 2006;151(3):713–9.
Dhar A, Mullish BH, Thursz MR. Anticoagulation in chronic liver disease. J Hepatol. 2017;66(6):1313–26.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–962.
Lip GYH, Banerjee A, Boriani G, Ce C, Fargo R, Freedman B, et al. Antithrombotic therapy for atrial fibrillation. Chest. 2018;154(5):1121–201.
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2019;16(8):e66–93.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Demets DL. Methods for combining randomized clinical trials: strengths and limitations. Stat Med. 1987;6(3):341–50.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Grant RL. Converting an odds ratio to a range of plausible relative risks for better communication of research findings. BMJ. 2014;348:f7450.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Lee SR, Lee HJ, Choi EK, Han KD, Jung JH, Cha MJ, et al. Direct oral anticoagulants in patients with atrial fibrillation and liver disease. J Am Coll Cardiol. 2019;73(25):3295–308.
Pastori D, GYH L, Farcomeni A, Del Sole F, Sciacqua A, Perticone F, et al. Incidence of bleeding in patients with atrial fibrillation and advanced liver fibrosis on treatment with vitamin K or non-vitamin K antagonist oral anticoagulants. Int J Cardiol. 2018;264((Pastori D.; Del Sole F.; Pignatelli P.; Violi F., francesco.violi@uniroma1.it) I Clinica Medica, Atherothrombosis Centre, Department of Internal Medicine and Medical Specialties of Sapienza University of Rome, Rome, Italy:58–63.
Goriacko P, Veltri KT. Safety of direct oral anticoagulants vs warfarin in patients with chronic liver disease and atrial fibrillation. Eur J Haematol. 2018;100(5):488–93.
Lee HF, Chan YH, Chang SH, Tu HT, Chen SW, Yeh YH, et al. Effectiveness and safety of non-vitamin K antagonist Oral anticoagulant and warfarin in cirrhotic patients with nonvalvular atrial fibrillation. J Am Heart Assoc. 2019;8(5):e011112.
Wang CL, Wu VC, Kuo CF, Chu PH, Tseng HJ, Wen MS, et al. Efficacy and safety of non-vitamin K antagonist oral anticoagulants in atrial fibrillation patients with impaired liver function: a retrospective cohort study. J Am Heart Assoc. 2018;7(15):e009263.
Qamar A, Antman EM, Ruff CT, Nordio F, Murphy SA, Grip LT, et al. Edoxaban versus warfarin in patients with atrial fibrillation and history of liver disease. J Am Coll Cardiol. 2019;74(2):179–89.
Davis KA, Joseph J, Nisly SA. Direct oral anticoagulants and warfarin in patients with cirrhosis: a comparison of outcomes. J Thromb Thrombolysis. 2020;50:457–61.
Cisak KI, Asante D, Grill DE, Ashrani AA. Efficacy and safety of direct oral anticoagulants in patients with cirrhosis-single institution experience. Blood. 2018;132 (Supplement 1): 2525.
Intagliata NM, Henry ZH, Maitland H, Shah NL, Argo CK, Northup PG, et al. Direct oral anticoagulants in cirrhosis patients pose similar risks of bleeding when compared to traditional anticoagulation. Dig Dis Sci. 2016;61(6):1721–7.
Alonso A, MacLehose RF, Chen LY, Bengtson LG, Chamberlain AM, Norby FL, et al. Prospective study of oral anticoagulants and risk of liver injury in patients with atrial fibrillation. Heart. 2017;103(11):834–9.
Alonso A, MacLehose RF, Chen LY, Bengtson LG, Chamberlain AM, Norby FL, et al. Abstract 13824: Oral anticoagulants and risk of liver injury in patients with atrial fibrillation: A prospective study. Circulation 2016;134:A13824-A.
Chokesuwattanaskul R, Thongprayoon C, Bathini T, Torres-Ortiz A, O’Corragain OA, Watthanasuntorn K, et al. Efficacy and safety of anticoagulation for atrial fibrillation in patients with cirrhosis: a systematic review and meta-analysis. Dig Liver Dis. 2019;51(4):489–95.
Fu Y, Zhu W, Zhou Y, Chen H, Yan L, He W. Non-vitamin K antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and liver disease: a meta-analysis and systematic review. Am J Cardiovasc Drugs. 2019;19:37–47.
Ioannou GN, Beste LA, Green PK, Singal AG, Tapper EB, Waljee AK, et al. Increased risk for hepatocellular carcinoma persists up to 10 years after HCV eradication in patients with baseline cirrhosis or high FIB-4 scores. Gastroenterology. 2019;157(5):1264–78 e4.
Efird LM, Mishkin DS, Berlowitz DR, Ash AS, Hylek EM, Ozonoff A, et al. Stratifying the risks of oral anticoagulation in patients with liver disease. Circ Cardiovasc Qual Outcomes. 2014;7(3):461–7.
Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39(16):1330–93.
De Gottardi A, Trebicka J, Klinger C, Plessier A, Seijo S, Terziroli B, et al. Antithrombotic treatment with direct-acting oral anticoagulants in patients with splanchnic vein thrombosis and cirrhosis. Liver Int. 2017;37(5):694–9.
Gallagher C, Sanders P, Wong CX. Anticoagulation for atrial fibrillation in cirrhosis of the liver: are low-dose non-vitamin k oral anticoagulants a reasonable alternative to warfarin?. J Am Heart Assoc. 2019;8(5):e012102.
Goto S, Ikeda Y, Chan JC, Wilson PW, Yeo TC, Liau CS, et al. Risk-factor profile, drug usage and cardiovascular events within a year in patients with and at high risk of atherothrombosis recruited from Asia as compared with those recruited from non-Asian regions: a substudy of the REduction of Atherothrombosis for Continued Health (REACH) registry. Heart Asia. 2011;3(1):93–8.
Rieder MJ, Reiner AP, Gage BF, Nickerson DA, Eby CS, McLeod HL, et al. Effect of VKORC1 haplotypes on transcriptional regulation and warfarin dose. N Engl J Med. 2005;352(22):2285–93.
Shen AY, Yao JF, Brar SS, Jorgensen MB, Chen W. Racial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillation. J Am Coll Cardiol. 2007;50(4):309–15.
Gue YX, Inoue N, Spinthakis N, Takei A, Takahara H, Otsui K, et al. Thrombotic profile and Oral anticoagulation in Asian and non-Asian patients with nonvalvular atrial fibrillation. J Am Coll Cardiol. 2019;74(22):2822–4.
Chao TF, Chen SA, Ruff CT, Hamershock RA, Mercuri MF, Antman EM, et al. Clinical outcomes, edoxaban concentration, and anti-factor Xa activity of Asian patients with atrial fibrillation compared with non-Asians in the ENGAGE AF-TIMI 48 trial. Eur Heart J. 2019;40(19):1518–27.
Elhosseiny S, Al Moussawi H, Chalhoub JM, Lafferty J, Deeb L. Direct oral anticoagulants in cirrhotic patients: current evidence and clinical observations. Can J Gastroenterol Hepatol. 2019;2019:4383269.
Stangier J, Stahle H, Rathgen K, Roth W, Shakeri-Nejad K. Pharmacokinetics and pharmacodynamics of dabigatran etexilate, an oral direct thrombin inhibitor, are not affected by moderate hepatic impairment. J Clin Pharmacol. 2008;48(12):1411–9.
Steuber TD, Howard ML, Nisly SA. Direct oral anticoagulants in chronic liver disease. Ann Pharmacother. 2019;53(10):1042–9.
Kubitza D, Roth A, Becka M, Alatrach A, Halabi A, Hinrichsen H, et al. Effect of hepatic impairment on the pharmacokinetics and pharmacodynamics of a single dose of rivaroxaban, an oral, direct factor Xa inhibitor. Br J Clin Pharmacol. 2013;76(1):89–98.
Funding
This study was supported by grants from the Natural Science Foundation (No. 81960770 and No. 81960048) of PR China, the Natural Science Foundation (No. 2018MS08099 and No. 2018LH08034) of Inner Mongolia province, Project of Inner Mongolia Science & Technology Program (No. 201802112), Science technology millions of projects of Inner Mongolia Medical University and doctoral Sustentation Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, ZC., Li, CQ., Liu, XY. et al. Efficacy and Safety of Direct Oral Anticoagulants in Patients with Atrial Fibrillation and Liver Disease: a Meta-Analysis and Systematic Review. Cardiovasc Drugs Ther 35, 1205–1215 (2021). https://doi.org/10.1007/s10557-020-07065-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-020-07065-y