Abstract
Purpose
Current practice guidelines support the use of angiotensin-converting enzyme inhibitors (ACEi) and angiotensin-receptor blockers (ARBs) in patients with coronary artery disease (CAD) without heart failure (HF). However, a number of cited trials were performed prior to the era of prevalent statin use. Our objective was to evaluate the effectiveness of ACEi and ARBs in reducing cardiovascular events as well as the impact of statin therapy.
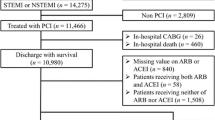
Methods
We searched the MEDLINE and EMBASE databases for randomized-controlled trials (1/1/1980 – 8/31/2015) with ACEi or ARBs as the single intervention for patients with CAD without HF. We assessed the outcomes of non-fatal myocardial infarction (MI), stroke, cardiovascular mortality and all-cause mortality. The relationship between these outcomes and the percentages of patients on statin therapy was evaluated using meta-regression analysis.
Results
A total of ten ACEi trials and five ARB trials were included for analysis, with 78,761 patients followed for a mean of 36 months. Treatment with ACEi was associated with decreased non-fatal MI (RR 0.83; 95 % CI 0.75–0.91), stroke (RR 0.76; 95 % CI 0.68–0.86), cardiovascular mortality (RR 0.83; 95 % CI 0.72–0.95), and all-cause mortality (RR 0.86; 95 % CI 0.80–0.93). Treatment with ARBs was associated only with a decreased incidence of stroke (RR 0.92; 95 % CI 0.87–0.98). When adjusted for statin use, there was a trend towards an attenuated effect of ACEi in reducing cardiovascular mortality with increased use of statins (p-value = 0.063).
Conclusion
In CAD patients without HF, ACEi, but not ARBs decreases the risk of non-fatal MI, cardiovascular mortality and all-cause mortality, while both ACEi and ARBs decrease the risk of stroke.



Similar content being viewed by others
References
American Heart Association Heart Disease, Stroke Statistics Writing Group. Heart disease and stroke statistics—2013 update. Circulation. 2013;127:e6–e245.
Fourth International Study of Infarct Survival Collaborative Group. A randomized factorial trial assessing oral captopril, oral mononitrate, and intravenous magnesium sulphate in 58,050 patients with suspected acute myocardial infarction. ISIS-4. Lancet. 1995;345:669–85.
GISSI-3 Investigators, Gruppo Italiano per lo Studio della Sopravvivenza nell’infarto Miocardico. Effects of lisinopril and transdermal glyceryl trinitrate singly and together on 6-week mortality and ventricular function after acute myocardial infarction. Lancet. 1994;343:1115.
The Acute Infarction Ramipril Efficacy (AIRE) Study Investigators. Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet. 1993;342:821–8.
Ambrosioni E, Borghi C, Magnani B, The Survival of Myocardial Infarction Long-Term Evaluation (SMILE) Study Investigators. The effect of the angiotensin-converting enzyme inhibitor zofenopril on mortality and morbidity after anterior myocardial infarction. N Engl J Med. 1995;332:80–5.
Pfeffer MA, Greaves SC, Arnold JM, The Healing and Early Afterload Reducing Therapy (HEART) Trial Investigators, et al. Early versus delayed angiotensin-converting enzyme inhibition therapy in acute myocardial infarction. The Healing and Early Afterload Reducing Therapy Trial. Circulation. 1997;95:2643–51.
Staessen J, Wang J, Thijs L. Cardiovascular protection and blood pressure reduction: a meta-analysis. Lancet. 2001;358:1305–15.
Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively designed overviews of randomized trials. Lancet. 2003;362:1527–35.
Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure lowering drugs: results of prospectively designed overviews of randomized trials. Lancet. 2000;356:1955–64.
Kjoller-Hansen L, Steffensen R, Grande P. The Angiotensin-converting Enzyme Inhibition Post Revascularization Study (APRES). J Am Coll Cardiol. 2000;35:881–8.
Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342:145–53.
MacMahon S, Sharpe N, Gamble G, PART-2 Collaborative Research Group, et al. Randomized, placebo-controlled trial of the angiotensin-converting enzyme inhibitor, ramipril, in patients with coronary or other occlusive arterial disease. J Am Coll Cardiol. 2000;36:438–43.
Pitt B, O’Neill B, Feldman R, et al. The Quinapril Ischemic Event Trial (QUIET): evaluation of chronic ACE inhibitor therapy in patients with ischemic heart disease and preserved left ventricular. Am J Cardiol. 2001;87:1058–63.
Lewis EJ, Hunsicker LG, Clarke WR, Collaborative Study Group, et al. Renoprotective effect of the -receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes (IDNT). N Engl J Med. 2001;345:851–60.
Brenner BM, Cooper ME, de Zeeuw D, RENAAL Study Investigators, et al. Effects of losartan, on renal and cardiovascular outcomes in patients with type 2 diabetes, and nephropathy. N Engl J Med. 2001;345:861–9.
European Trial on Reduction of Cardiac Events with Perindopril in Stable Coronary Artery Disease Investigators. Efficacy on perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: randomized, double-blind, placebo-controlled, multicentre trial (the EUROPA study). Lancet. 2003;362:782–8.
The PEACE Trial Investigators. Angiotensin-converting enzyme inhibition in stable coronary artery disease. N Engl J Med. 2004;351:2058–68.
Nissen SE, Tuzcu EM, Libby P, et al. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure. The CAMELOT study: a randomized controlled trial. JAMA. 2004;292:2217–26.
Ferrari R, Perindopril and Remodeling in Elderly with Acute Myocardial Infarction Investigators. Effects of angiotensin-converting enzyme inhibition with perindopril on left ventricular remodeling and clinical outcome: results of the randomized Perindopril and Remodeling in Elderly with Acute Myocardial Infarction (PREAMI) Study. Arch Intern Med. 2006;166:659–66.
Borghi C, Ambrosioni E. On behalf of the Survival of Myocardial Infarction Long-term Evaluation (SMILE) Study Group Effects of zofenopril on myocardial ischemia in post–myocardial infarction patients with preserved left ventricular function: The Survival of Myocardial Infarction Long-term Evaluation (SMILE)–ISCHEMIA study. Am Heart J. 2007;153:445e7–14.
Bosch J, Yusuf S, Gerstein HC, DREAM Trial Investigators, et al. Effect of ramipril on the incidence of diabetes. N Engl J Med. 2006;355:1551–62.
The Telmisartan Randomized Assessment Study in ACE Intolerant Subjects with Cardiovascular Disease (TRANSCEND) Investigators. Effects of the angiotensin-receptor blocker telmisartan on cardiovascular events in high-risk patients intolerant to angiotensin-converting enzyme inhibitors: a randomized controlled trial. Lancet. 2008;372:1174–83.
Yusuf S, Diener HC, Sacco RL, PROFESS Study Group, et al. Telmisartan to prevent recurrent stroke and cardiovascular events. N Engl J Med. 2008;359:1225–37.
The NAVIGATOR Study Group. Effect of Valsartan on the incidence of diabetes and cardiovascular events. N Engl J Med. 2010;362:1477–90.
Al-Mallah MH, Tleyjeh IM, Abdel-Latif AA, Weaver WD. Angiotensin-converting enzyme inhibitors in coronary artery disease and preserved left ventricular systolic function. A systematic review and meta-analysis of randomized controlled trials. J Am Coll Cardiol. 2006;47:1576–83.
Dagenais GR, Pogue J, Fox K, Simoons ML, Yusuf S. Angiotensin-converting-enzyme inhibitors in stable vascular disease without left ventricular systolic dysfunction or heart failure: a combined analysis of three trials. Lancet. 2006;368:581–8.
Danchin N, Cucherat M, Thuillez C, Durand E, Kadri Z, Steq PG. Angiotensin-converting enzyme inhibitors in patients with coronary artery disease and absence of heart failure or left ventricular systolic dysfunction: an overview of long-term randomized controlled trials. Arch Intern Med. 2006;166:787–96.
Van Vark LC, Bertrand M, Akkerhius KM, et al. Angiotensin-converting-enzyme inhibitors reduce mortality in hypertension: a meta-analysis of randomized clinical trials of rennin-angiotensin-aldosterone system inhibitors involving 158,998 patients. Eur Heart J. 2012;33:2088–97.
Baker WL, Coleman CI, Kluger J, et al. Systematic review: comparative effectiveness of angiotensin-converting enzyme inhibitors or angiotensin II-receptor blockers for ischemic heart disease. Ann Intern Med. 2009;12:861–71.
Fihn SD, Gardin JM, Abrams J, et al. ACCF/AHA/ACP/AATS/PCNA/SCAI/STS 2012 guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary. Circulation. 2012;126:3097–137.
Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/ non-ST-elevation myocardial infarction: a report of the American College of Cardiology/ American Heart Association Task Force on practice guidelines. Circulation. 2007;116:148–304.
O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:362–425.
Montalescot G, Sechtem U, Achenbach S, et al. ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949–3003.
Hamm CW, Bassand JP, Agewall S, et al. ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011;32:2999–3054.
Steg PG, James SK, Atar D, et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569–619.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100.
Review Manager (RevMan) [Computer program], Version 5.0. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration, 2008.
Yusef S, Pogue J. ACE inhibition in stable coronary artery disease. N Engl J Med. 2005;352:937–9.
Mancini GB, Henry GC, Macaya C, et al. Angiotensin-converting enzyme inhibition with quinapril improves endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation. 1996;94:258–65.
Bonetti PO, Lerman LO, Napoli C, Lerman A. Statin effects beyond lipid lowering—are they clinically relevant? Eur Heart J. 2003;24:225–48.
Zhang X, Xie YW, Nasjletti A, Xu X, Wolin MS, Hintze TH. ACE inhibitors promote nitric oxide accumulation to modulate myocardial oxygen consumption. Circulation. 1997;95:176–82.
Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker Valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–75.
Yancy CW, Jessup M, Bozkurt B, et al. ACCF/AHA guideline for the management of heart failure. Circulation. 2013;128:e240–327.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors report no relationships that could be construed as a conflict of interest.
Rights and permissions
About this article
Cite this article
Hoang, V., Alam, M., Addison, D. et al. Efficacy of Angiotensin-Converting Enzyme Inhibitors and Angiotensin-Receptor Blockers in Coronary Artery Disease without Heart Failure in the Modern Statin Era: a Meta-Analysis of Randomized-Controlled Trials. Cardiovasc Drugs Ther 30, 189–198 (2016). https://doi.org/10.1007/s10557-016-6652-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-016-6652-7