Abstract
Aims
The objective of the present substudy was to examine whether aspirin poor/high responsiveness (APR/AHR) is associated with increased rates of major adverse cardiovascular events (MACE) and serious bleeding after primary percutaneous coronary intervention (PPCI).
Methods
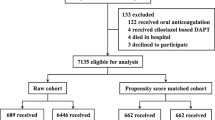
We analyzed 961 consecutive ST-elevation acute myocardial infarction patients who underwent PPCI between February 2008 and June 2011. Multiplate analyser (Dynabite, Munich, Germany) was used for the assessment of platelet reactivity. APR/AHR were defined as the upper/lower quintiles of ASPI values, determined 24 h after aspirin loading. APR patients were tailored using 300 mg maintenance dose for 30 days. The co-primary end points at 30 days were: MACE (death, non-fatal infarction, ischemia-driven target vessel revascularization and ischemic stroke) and serious bleeding according to the BARC classification.
Results
One hundred and 90 patients were classified as APR, and 193 patients as AHR. At admission, compared with aspirin sensitive patients (ASP), patients with APR had more frequently diabetes, anterior infarction and heart failure, while AHR patients had reduced values of creatine kinase, leukocytes, heart rate and systolic blood pressure. Compared with ASP, the rates of 30-day primary end points did not differ neither in APR group including tailored patients (MACE, adjusted OR 1.02, 95%CI 0.47-2.17; serious bleeding, adjusted OR 1.92, 95%CI 0.79-4.63), nor in patients with AHR (MACE, adjusted OR 1.58, 95%CI 0.71-5.51; serious bleeding, adjusted OR 0.69, 95%CI 0.22-2.12).
Conclusions
The majority of APR patients were suitable for tailoring. Neither APR including tailored patients nor AHR were associated with adverse 30-day efficacy or safety clinical outcomes.

Similar content being viewed by others
Abbreviations
- PPCI:
-
Primary percutaneous coronary intervention
- APR:
-
Aspirin poor responsiveness
- AHR:
-
Aspirin high responsiveness
- ASP:
-
Aspirin sensitive patients
- MACE:
-
Major adverse cardiovascular events
- STEMI:
-
ST-elevation myocardial infarction
- ART-PCI:
-
The Antiplatelet Regimen Tailoring after primary PCI trial
References
Tobbia P, Brodie BR, Witzenbichler B, et al. Adverse event rates following primary PCI for STEMI at US and non-US hospitals: three-year analysis from the HORIZONS-AMI trial. EuroIntervention. 2013;8:1134–42.
Menees DS, Peterson ED, Yongfei Wang Y, et al. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369:901–9.
Althoff TF, Fischer M, Langer E, Ziemer S, Baumann G. Sustained enhancement of residual platelet reactivity after coronary stenting in patients with myocardial infarction compared to elective patients. Thromb Res. 2010;125:e190–6.
Hobikoglu GF, Norgaz T, Aksu H, et al. High frequency of aspirin resistance in patients with acute coronary syndrome. Tohoku J Exp Med. 2005;207:59–64.
Poulsen TS, Jorgensen B, Korsholm L, et al. Prevalence of aspirin resistance in patients with an evolving acute myocardial infarction. Thromb Res. 2007;119:555–62.
Eikelboom JW, Hankey GJ, Thom J, et al., for the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization. Management and avoidance (CHARISMA) investigators. Incomplete inhibition of thromboxane biosynthesis by acetylsalicylic acid: determinants and effect on cardiovascular risk. Circulation 2008;118:1705–12.
Rafferty M, Walters MR, Dawson J. Antiplatelet therapy and aspirin resistance - clinically and chemically relevant? Curr Med Chem. 2010;17:4578–86.
Cheng X, Chen WH, Simon DI. Aspirin resistance or variable response or both? Am J Cardiol. 2006;98:11N–7N.
Rao GHR, Jan Jaques Michiels JJM. Aspirin resistance: does it exist? Semin Thromb Hemost. 2007;33:210–4.
Marcucci R, Gori AM, Paniccia R, et al. Cardiovascular death and nonfatal myocardial infarction in acute coronary syndrome patients receiving coronary stenting are predicted by residual platelet reactivity to ADP detected by a point-of-care assay. A 12-month follow-up. Circulation. 2009;119:237–42.
Parodi G, Marcucci R, Valenti R, et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011;306:1215–23.
Wenaweser P, Dörffler-Melly J, Imboden K, et al. Stent thrombosis is associated with an impaired response to antiplatelet therapy. J Am Coll Cardiol. 2005;45:1748–52.
Chiu FC, Wang TD, Jen-Kuang Lee JK, et al. Residual platelet reactivity after aspirin and clopidogrel treatment predicts 2-year major cardiovascular events in patients undergoing percutaneous coronary intervention. Europ J Int Med. 2011;22:471–7.
Eikelboom JW, Hirsh J, Weitz JI, et al. Aspirin-resistant thromboxane biosynthesis and the risk of myocardial infarction, stroke, or cardiovascular death in patients at high risk for cardiovascular events. Circulation. 2002;105:1650–5.
Mehta SR, Tanguay JF, Eikelboom JW, et al, on behalf of the CURRENT-OASIS 7 trial investigators. Double-dose versus standard-dose clopidogrel and high-dose versus low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomised factorial trial. Lancet 2010; 376: 1233–43.
Campo G, Fileti L, de Cesare N, et al, on behalf of the 3 T/2R Investigators. Long-term clinical outcome based on aspirin and clopidogrel responsiveness status after elective percutaneous coronary intervention. A 3 T/2R (tailoring treatment with tirofiban in patients showing resistance to aspirin and/or resistance to clopidogrel) trial substudy. J Am Coll Cardiol 2010; 56:1447–55.
Pamukcu B, Oflaz H, Oncul A, Umman B, et al. The role of aspirin resistance on outcome in patients with acute coronary syndrome and the effect of clopidogrel therapy in the prevention of major cardiovascular events. J Thromb Thrombolysis. 2006;22:103–10.
Grotemeyer KH, Scharafinski HW, Husstedt IW. Two-year follow-up of aspirin responder and aspirin non responder. A pilot-study including 180 post-stroke patients. Thromb Res. 1993;71:397–403.
Fuchs I, Frossard M, Spiel A, et al. Platelet function in patients with acute coronary syndrome (ACS) predicts recurrent ACS. J Thromb Haemost. 2006;4:2547–52.
Grundmann K, Jaschonek K, Kleine B, et al. Aspirin non-responder status in patients with recurrent cerebral ischemic attacks. J Neurol. 2003;250:63–6.
Marcucci R, Paniccia R, Antonucci E, et al. Usefulness of aspirin resistance after percutaneous coronary intervention for acute myocardial infarction in predicting one-year major adverse coronary events. Am J Cardiol. 2006;98:1156–9.
Pettersen AR, Seljeflot I, Abdelnoor M, et al. High on-aspirin platelet reactivity and clinical outcome in patients with stable coronary artery disease: results from ASCET (Aspirin Nonresponsiveness and Clopidogrel Endpoint Trial). J Am Heart Assoc. 2012;1:e000703.
Gurbel PA, Bliden KP, DiChiara J, et al. Evaluation of dose-related effects of aspirin on platelet function results from the aspirin-induced platelet effect (ASPECT) study. Circulation. 2007;115:3156–64.
Neubauer H, Kaiser AF, Endres HG, et al. Tailored antiplatelet therapy can overcome clopidogrel and aspirin resistance - the Bochum CLopidogrel and aspirin plan (BOCLAPlan) to improve antiplatelet therapy. BMC Medicine. 2011;9:3.
Mrdovic I, Savic L, Krljanac G, et al. Impact of high post-loading platelet aggregation on 30-day clinical outcomes after primary percutaneous coronary intervention. The antiplatelet regimen tailoring after primary PCI (ART-PCI) trial. Intern J Cardiol. 2013;167(4):1632–7.
Sibbing D, Braun S, Morath T, et al. Platelet reactivity after clopidogrel treatment assessed with point-of-care analysis and early drug-eluting stent thrombosis. J Am Coll Cardiol. 2009;53:849–56.
Mehran R, Rao S, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials. A consensus report from the bleeding academic research consortium Circulation 2011; 123:2736–47.
Frelinger 3rd AL, Furman MI, Linden MD, et al. Residual arachidonic acid-induced platelet activation via an adenosine diphosphate-dependent but cyclooxygenase-1 and cyclooxygenase 2-independent pathway. A 700-patient study of aspirin resistance. Circulation. 2006;113:2888–96.
Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR. Aspirin “resistance” and risk of cardiovascular morbidity: systematic review and meta-analysis. BMJ. 2008;336:195–8.
Sane DC, McKee SA, Malinin AI, Serebruany VL. Frequency of aspirin resistance in patients with congestive heart failure treated with antecedent aspirin. Am J Cardiol. 2002;90:893–5.
Patrignani P, Filabozzi P, Patrono C. Selective cumulative inhibition of platelet thromboxane production by low-dose aspirin in healthy subjects. J Clin Invest. 1982;69:1366–72.
Frossard M, Fuchs I, Leitner J, et al. Platelet function predicts myocardial damage in patients with acute myocardial infarction. Circulation. 2004;110:1392–7.
Macchi L, Christiaens L, Brabant S, et al. Resistance to aspirin in vitro is associated with increased platelet sensitivity to adenosine diphosphate. Thromb Res. 2002;107:45–9.
Price MJ, Berger PB, Teirstein PS, et al, for the GRAVITAS Investigators. Standard- versus high-dose clopidogrel based on platelet function testing after percutaneous coronary intervention The GRAVITAS Randomized Trial JAMA 2011; 305:1097–1105.
Chen WH, Cheng X, Lee PY, et al. Aspirin resistance and adverse clinical events in patients with coronary artery disease. Am J Med. 2007;120:631–5.
Chiu FC, Wang TD, Lee JK, et al. Residual platelet reactivity after aspirin and clopidogrel treatment predicts 2-year major cardiovascular events in patients undergoing percutaneous coronary intervention. Eur J Int Med. 2011;22:471–7.
Snoep JD, Hovens MMC, Eikenboom JCJ, van der Bom JG, Huisman MV. Association of laboratory defined aspirin resistance with a higher risk of recurrent cardiovascular events: a systematic review and meta-analysis. Arch Int Med. 2007;167:1593–9.
Barent R, Auer J, Franklin B, et al. Platelet response to aspirin 50 and 100 mg in patients with coronary heart disease over a five year period. Am J Cardiol. 2011;108:644–50.
Campbell CL, Smyth S, Montalescot G, Steinhubl SR. Aspirin dose for the prevention of cardiovascular disease: a systematic review. JAMA. 2007;297:2018–24.
Patrono C, Baigent C, Hirsh J, Roth G, American College of Chest Physicians. Antiplatelet drugs: evidence-based clinical practice guidelines (8th Edition). Chest. 2008;133:199S–233S.
Mehran R, Lansky AJ, Witzenbichler B, et al. Bivalirudin in patients undergoing primary angioplasty for acute myocardial infarction (HORIZONS-AMI): 1-year results of a randomized controlled trial. Lancet. 2009;374:1149–59.
Paniccia R, Antonucci E, Maggini N, et al. Assessment of platelet function on whole blood by multiple electrode aggregometry in high-risk patients with coronary artery disease receiving antiplatelet therapy. Am J Clin Pathol. 2009;131:834–42.
Acknowledgments
This work was supported by the Ministry of Science and Technological Development of the Republic of Serbia, Contract No. 172033. The authors express their gratitude to all physicians and nurses of the Clinical Center’s of Serbia Coronary Unit and Catheterization Laboratory who took part in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None declared.
Rights and permissions
About this article
Cite this article
Mrdovic, I., Čolić, M., Savic, L. et al. Clinical Significance of Laboratory-determined Aspirin Poor Responsiveness After Primary Percutaneous Coronary Intervention. Cardiovasc Drugs Ther 30, 151–158 (2016). https://doi.org/10.1007/s10557-016-6643-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-016-6643-8