Abstract
Purpose
This study aimed to evaluate the cost-effectiveness of statins for primary prevention of stroke and myocardial infarction (MI) in the elderly in Singapore.
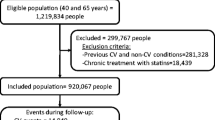
Methods
A Markov model was developed to investigate the lifetime costs, quality-adjusted life years (QALYs) and incremental cost-effectiveness ratios (ICERs) of statin treatment in those aged 65 years and older without a history of stroke or MI from the perspective of Singapore’s healthcare system, using elderly-specific clinical data and local costs from hospital databases. A lifetime horizon was used and all costs and health outcomes were discounted at 3 % annually.
Results
In the base-case analysis, statin treatment prevented an additional four strokes and eight MIs among 1,000 “healthy” elderly individuals compared with no treatment. Statin treatment resulted in a QALY gain of 0.26 and additional costs of SGD 11,314 per person, yielding an ICER of SGD 43,925 (USD 33,495) per QALY gained. The results were sensitive to statin effectiveness, particularly statins’ effect on all-cause mortality, and cost of statin medication. Probabilistic sensitivity analysis demonstrated that the probability of statin treatment being cost-effective was 72 % at a willingness-to-pay threshold of SGD 65,000 (USD 49,546) per QALY gained. Shortening the time horizon from lifetime to 10 years (simulating limited life expectancy) considerably increased the ICER to SGD 291,313 (USD 167,171) per QALY. Female gender and younger age were also associated with higher ICERs owing to a lower baseline risk of cardiovascular disease (CVD) and higher costs to manage events in these subgroups.
Conclusions
Statin treatment for the primary prevention of CVD in the elderly was cost-effective. However, treatment warrants re-evaluation when the prognosis of the individual is considered less than ten years; other goals may take precedence over CVD prevention.




Similar content being viewed by others
References
Yusuf S, Reddy S, Ounpuu S, et al. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–53.
Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81.
Taylor F, Ward K, Moore TH, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2011; CD004816.
Brugts JJ, Yetgin T, Hoeks SE, et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trials. BMJ (Clin Res ed). 2009;338:b2376.
Mihaylova B, Emberson J, Blackwell L, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–90.
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American college of cardiology/american heart association task force on practice guidelines. J Am Coll Cardiol. 2014;63:2889–934.
Ioannidis JA. More than a billion people taking statins? Potential implications of the new cardiovascular guidelines. JAMA: J Am Med Assoc. 2014;311:463–4.
Lazar LD, Pletcher MJ, Coxson PG, et al. Cost-effectiveness of statin therapy for primary prevention in a low-cost statin era. Circulation. 2011;124:146–53.
Greving JP, Visseren FL, de Wit GA, et al. Statin treatment for primary prevention of vascular disease: whom to treat? Cost-effectiveness analysis. BMJ (Clin Res ed). 2011;342:d1672.
Ward S, Lloyd Jones M, Pandor A, et al. A systematic review and economic evaluation of statins for the prevention of coronary events. Health Technol Assess. 2007;11:178.
The State of Aging and Health in America 2013. In: Centers for Disease Control and Prevention UDoHaHS, ed. Atlanta, GA, 2013.
Health at a Glance 2013. OECD Indicators. OECD Publishing, 2013.
Department of Statistics, Singapore. Complete life tables 2008–2013 for Singapore Resident Population. Available at: http://www.singstat.gov.sg/publications/publications_and_papers/births_and_deaths/lifetable08-13.pdf. Last accessed 1 December 2014.
Office for National Statistics, United Kingdom. National life tables 2011–2013. Available at: http://www.ons.gov.uk/ons/taxonomy/index.html?nscl=Life+Tables#tab-data-tables. Last accessed 1 December 2014.
Arias E. United States life tables, 2010, National vital statistics reports, vol. 7. 63rd ed. Hyattsville: National Center for Health Statistics; 2014.
Brønnum-Hansen H, Davidsen M, Thorvaldsen P, et al. Long-term survival and causes of death after stroke. Stroke. 2001;32(9):2131–6. September 1, 2001.
Smolina K, Wright FL, Rayner M, et al. Long-term survival and recurrence after acute myocardial infarction in England, 2004 to 2010. Circ: Cardiovasc Qual Outcomes. 2012;5(4):532–40. July 1, 2012.
Ellis JJ, Erickson SR, Stevenson JG, et al. Suboptimal statin adherence and discontinuation in primary and secondary prevention populations. J Gen Intern Med. 2004;19(6):638–45.
Bhardwaj S, Selvarajah S, Schneider EB. Muscular effects of statins in the elderly female: a review. Clin Interv Aging. 2013;8:47–59.
Law M, Rudnicka AR. Statin safety: a systematic review. Am J Cardiol. 2006;97:52C–60C.
Luengo-Fernandez R, Gray AM, Bull L, et al. Quality of life after TIA and stroke: ten-year results of the Oxford vascular study. Neurology. 2013;81:1588–95.
Xie J, Wu EQ, Zheng Z-J, et al. Patient-reported health status in coronary heart disease in the United States: age, sex, racial, and ethnic differences. Circulation. 2008;118:491–7.
Pignone M, Earnshaw S, Tice JA, et al. Aspirin, statins, or both drugs for the primary prevention of coronary heart disease events in men: a cost-utility analysis. Ann Intern Med. 2006;144:326–36.
Pletcher MJ, Lazar L, Bibbins-Domingo K, et al. Comparing impact and cost-effectiveness of primary prevention strategies for lipid-lowering. Ann Intern Med. 2009;150:243–54.
Schreiber DH, Anderson TR. Statin-induced rhabdomyolysis. J Emerg Med. 2006;31:177–80.
Skrabal MZ, Stading JA, Cannella CA, et al. Two cases of rhabdomyolysis associated with high-dose simvastatin. Am J Health Syst Pharm: AJHP: Off J Am Soc Health Syst Pharm. 2003;60:578–81.
Tan WS, Heng BH, Chua KS, et al. Factors predicting inpatient rehabilitation length of stay of acute stroke patients in Singapore. Arch Phys Med Rehabil. 2009;90:1202–7.
Department of Statistics, Singapore. Latest data on GDP per capita. Available at: http://www.singstat.gov.sg/statistics/latest_data.html#1. Last accessed 1 September 2014.
Sachs JD. Macroeconomics and Health: Investing in Health for Economic Development. Report of the Commision on Macroeconomics and Health. Geneva, Switzerland: World Health Organisation, 2011. Available at: http://whqlibdoc.who.int/publications/2001/924154550x.pdf. Accessed on 1 September 2014.
Kostis WJ, Cheng JQ, Dobrzynski JM, et al. Meta-analysis of statin effects in women versus men. J Am Coll Cardiol. 2012;59:572–82.
Bushnell CD, Reeves MJ, Zhao X, et al. Sex differences in quality of life after ischemic stroke. Neurology. 2014;82:922–31.
Alexander KP, Newby LK, Armstrong PW, et al. Acute coronary care in the elderly, part II: ST-segment–elevation myocardial infarction: a scientific statement for healthcare professionals from the American heart association council on clinical cardiology: in collaboration with the society of geriatric cardiology. Circulation. 2007;115:2570–89.
Mehta RH, Rathore SS, Radford MJ, et al. Acute myocardial infarction in the elderly: differences by age. J Am Coll Cardiol. 2001;38:736–41.
Collier DJ, Poulter NR, Dahlof B, et al. Impact of atorvastatin among older and younger patients in the Anglo-Scandinavian cardiac outcomes trial lipid-lowering arm. J Hypertens. 2011;29:592–9.
Bruckert E, Lievre M, Giral P, et al. Short-term efficacy and safety of extended-release fluvastatin in a large cohort of elderly patients. Am J Geriatr Cardiol. 2003;12:225–31.
Neil HA, DeMicco DA, Luo D, et al. Analysis of efficacy and safety in patients aged 65–75 years at randomization: collaborative atorvastatin diabetes study (CARDS). Diabetes Care. 2006;29:2378–84.
Collins R, Armitage J, Parish S, et al. MRC/BHF heart protection study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet. 2003;361:2005–16.
Glynn RJ, Koenig W, Nordestgaard BG, et al. Rosuvastatin for primary prevention in older persons with elevated C-reactive protein and low to average low-density lipoprotein cholesterol levels: exploratory analysis of a randomized trial. Ann Intern Med. 2010;152:488–96. W174.
Nakaya N, Mizuno K, Ohashi Y, et al. Low-dose pravastatin and age-related differences in risk factors for cardiovascular disease in hypercholesterolaemic Japanese: analysis of the management of elevated cholesterol in the primary prevention group of adult Japanese (MEGA study). Drugs Aging. 2011;28:681–92.
Shepherd J, Blauw GJ, Murphy MB, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–30.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Relationships with Industry: None
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 27 kb)
Rights and permissions
About this article
Cite this article
Lin, L., Teng, M., Zhao, Y.J. et al. Long-term Cost-effectiveness of Statin Treatment for Primary Prevention of Cardiovascular Disease in the Elderly. Cardiovasc Drugs Ther 29, 187–197 (2015). https://doi.org/10.1007/s10557-015-6584-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-015-6584-7