Abstract
Purpose
In patients with acute decompensated heart failure (ADHF) and left ventricular systolic dysfunction (LVSD), the role of initial vasodilator therapy remains uncertain. The present study aimed to evaluate the acute efficacy of initial carperitide therapy and to predict its response in ADHF patients with LVSD.
Methods
Twenty-four consecutive patients with ADHF and LVSD were enrolled. Inclusion criteria were a left ventricular ejection fraction < 40%, systolic blood pressure (BP) > 90 mm Hg, and pulmonary capillary wedge pressure ≥18 mm Hg at baseline. Hemodynamic parameters were evaluated by right heart catheterization before and after carperitide infusion. Responders were defined as a ≥30% reduction of pulmonary capillary wedge pressure (PCWP) or a decrease to < 16 mm Hg within 6 h after carperitide infusion.
Results
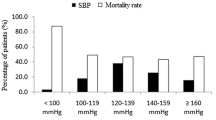
Seventeen (71%) of the 24 patients were responders for initial carperitide therapy. The responders had significantly higher systolic BP and cardiac index at baseline compared with nonresponders. The area under the curve (AUC) for systolic BP was 0.93 and a cut-off value of 120 mm Hg had a sensitivity of 94% and specificity of 86% for predicting the efficacy of carperitide. The AUC for the cardiac index was 0.88 and a cut-off value of 2.30 L/min/m2 had a sensitivity of 65% and a specificity of 100% for predicting the response to carperitide.
Conclusions
The initial use of carperitide therapy safely reduces PCWP in ADHF patients with LVSD and baseline systolic BP may be useful for predicting the response to initial carperitide therapy for ADHF with LVSD.



Similar content being viewed by others
References
Gheorghiade M, Zannad F, Sopko G, International Working Group on Acute Heart Failure Syndromes, et al. Acute heart failure syndromes: current state and framework for future research. Circulation. 2005;112:3958–68.
De Luca L, Mebazaa A, Filippatos G, et al. Overview of emerging pharmacological agents for acute heart failure syndromes. Eur J Heart Fail. 2008;10:201–13.
Nieminen MS, Harjola VP. Definition and epidemiology of acute heart failure syndromes. Am J Cardiol. 2005;96:5G–10G.
Mebazaa A, Gheorghiade M, Piña IL, et al. Practical recommendations for prehospital and early in-hospital management of patients presenting with acute heart failure syndromes. Crit Care Med. 2008;36:S129–S39.
Gheorghiade M, De Luca L, Fonarow GC, Filippatos G, Metra M, Francis GS. Pathophysiologic targets in the early phase of acute heart failure syndromes. Am J Cardiol. 2005;96:11G–7G.
Metra M, Teerlink JR, Voors AA, et al. Vasodilators in the treatment of acute heart failure: what we know, what we don’t. Heart Fail Rev 2008. Published online ahead of print 19 December 2008
Lee CYW, Burnett JC Jr. Natriuretic peptides and therapeutic applications. Heart Fail Rev. 2007;12:131–42.
Saito Y, Nakao K, Nishimura K, et al. Clinical application of atrial polypeptide in patients with congestive heart failure: beneficial effects on left ventricular function. Circulation. 1987;76:115–24.
Colucci WS, Elkayam U, Horton DP, et al. Intravenous nesiritide, a natriuretic peptide, in the treatment of decompensated congestive heart failure. N Eng J Med. 2000;343:246–53.
Publication Committee for the VMAC (Vasodilation in the management of acute CHF) Investigators. Intravenous nesiritide vs. nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA. 2002;287:1531–40.
Elkayam U, Akhter MW, Singh H, Khan S, Usman A. Comparison of effects on left ventricular filling pressure of intravenous nesiritide and high-dose nitroglycerin in patients with decompensated heart failure. Am J Cardiol. 2004;93:237–40.
Suwa M, Seino Y, Nomachi Y, Matsuki S, Funahashi K. Multicenter prospective investigation on efficacy and safety of carperitide for acute heart failure in the ‘real world’ of therapy. Circ J. 2005;69:283–90.
Nomura F, Kurobe N, Mori Y, et al. Multicenter prospective investigation on efficacy and safety of carperitide as a first-line drug for acute heart failure syndrome with preserved blood pressure-COMPASS: Carperitide effects observed through monitoring dyspnea in acute decompensated heart failure study. Circ J. 2008;72:1777–86.
Nieminen MS, Böhm M, Cowie MR, et al. ESC Committe for Practice Guideline. Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the Task Force on Acute heart Failure of the European Society of Cardiology. Eur Heart J. 2005;26:384–416.
Heart Failure Society of America. Executive summary: HFSA 2006 comprehensive heart failure practice guideline. J Card Fail. 2006;12:10–38.
Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur J Heart Fail. 2008;10:933–89.
Sackner-Bernstein JD, Skopicke HA, Aaronson KD. Risk of worsening renal function with nesiritide in patients with acutely decompensated heart failure. Circulation. 2005;111:1487–91.
Sackner-Bernstein JD, Kawalski M, Fox M, Aaronson KD. Short-term risk of death after treatment with nesiritide for decompensated heart failure. JAMA. 2005;293:1900–5.
Drazner MH, Hamilton MA, Fonarow G, Creaser J, Flavell C, Stevenson LW. Relationship between right and left-sided filling pressures in 1000 patients with advanced heart failure. J Heart Lung Transplant. 1999;18:1126–32.
Larsen AI, Gøransson L, Aarsland T, Tamby JF, Dickstein K. Comparison of the degree of hemodynamic tolerance during intravenous infusion of nitroglycerin versus nicorandil in patients with congestive heart failure. Am Heart J. 1997;134:435–41.
Witteles RM, Kao D, Christopherson D, et al. Impact of nesiritide on renal function in patients with acute decompensated heart failure and pre-existing renal dysfunction. J Am Coll Cardiol. 2007;50:1835–40.
Serizawa T, Hirata Y, Kohmoto O, et al. Acute hemodynamic effects of alpha human atrial natriuretic polypeptide in patients with congestive heart failure. Jpn Heart J. 1988;29:143–9.
Mizuno O, Onishi K, Dohi K, et al. Effects of therapeutic doses of human atrial natriuretic peptide on load and myocardial performance in patients with congestive heart failure. Am J Cardiol. 2001;88:863–6.
Cotter G, Williams SG, Vered Z, Tan LB. Role of cardiac power in heart failure. Curr Opin Cardiol. 2003;18:215–22.
Gheorghiade M, Abraham WT, Albert NM, et al. OPTIMIZE-HF Investigators and Coordinators. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296:2217–26.
Milo-Cotter O, Adams KF, O’Connor CM, et al. Acute heart failure associated with high admission blood pressure: a distinct vascular disorder? Eur J Heart Fail. 2007;9:178–83.
Mukoyama M, Nakao K, Hosoda K, et al. Brain natriuretic peptide as a novel cardiac hormone in humans. Evidence for an exquisite dual natriuretic peptide system, atrial natriuretic peptide and brain natriuretic peptide. J Clin Invest. 1991;87:1402–12.
Florkowski CM, Richards AM, Espiner EA, Yandle TG, Frampton C. Renal, endocrine, and hemodynamic interactions of atrial and brain natriuretic peptides in normal men. Am J Physiol. 1994;266:R1244–50.
Hunt PJ, Espiner EA, Richards AM, Yandle TG, Frampton C, Nicholls MG. Interactions of atrial and brain natriuretic peptides at pathophysiological levels in normal men. Am J Physiol. 1995;269:R1397–R403.
Kimura K, Yamaguchi Y, Horii M, et al. ANP is cleared much faster than BNP in patients with congestive heart failure. Eur J Clin Pharmacol. 2007;63:699–702.
Acknowledgement
We express our appreciation to Katsunori Shimada, PhD (STATZ Institute, Inc., Tokyo, Japan) for expert statistical assistance.
Funding Source and Conflict of Interest Disclosures
There were no funding sources and no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kajimoto, K., Sashida, Y., Minami, Y. et al. Systolic Blood Pressure at Admission as a Predictor of the Response to Initial Carperitide Therapy in Patients Hospitalized for Acute Decompensated Heart Failure with Left Ventricular Systolic Dysfunction. Cardiovasc Drugs Ther 23, 481–488 (2009). https://doi.org/10.1007/s10557-009-6207-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-009-6207-2