Abstract
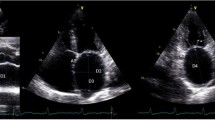
We sought to determine and prospectively validate, with concomitantly performed transthoracic (TTE) and transesophageal echocardiograms (TEE), a TTE-assessed E/e′ threshold that can be useful in predicting left atrial appendage (LAA) thrombus in patients with nonvalvular atrial fibrillation (NVAF). The retrospective derivation cohort was comprised of 297 patients with NVAF with TTE performed within 1 year of TEE. The validation cohort was comprised of 266 prospectively enrolled patients with TTE performed immediately prior to TEE. LAA thrombus was detected by TEE in 6.4 % of patients in both cohorts. Receiver operating characteristic (ROC) analyses demonstrated a good discriminatory capacity of lateral E/e′ in predicting LAA thrombus in the derivation cohort (AUC 0.72; CI 0.63–0.82; P = 0.001) which was confirmed in the validation cohort (AUC 0.83; CI 0.75–0.91; P < 0.001). In the derivation cohort, ROC curve point-coordinates identified E/e′ thresholds of both 9.0 and 8.0 to be associated with 100 % sensitivity, with specificities of 36 and 30 %, respectively. An E/e′ threshold of ≥8 was selected a priori for prospective validation, and was associated with 100 % sensitivity and 41 % specificity for LAA thrombus, with positive and negative predictive values of 10 and 100 %, respectively, and positive and negative likelihood ratios of 1.69 and 0, respectively. We determined and validated an E/e′ threshold of 8 as a highly sensitive and useful parameter that can aid in identifying patients at very low risk for LAA thrombus and potentially obviate the need for a TEE prior to electrophysiology procedures and restoration of sinus rhythm.

Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- CI:
-
95 % confidence intervals
- LA:
-
Left atrial
- LAA:
-
Left atrial appendage
- LV:
-
Left ventricular
- NVAF:
-
Nonvalvular atrial fibrillation
- ROC:
-
Receiver operating characteristic
- SEC:
-
Spontaneous echo contrast
- TEE:
-
Transesophageal echocardiogram
- TTE:
-
Transthoracic echocardiogram
References
Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S et al (2010) Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J 31(19):2369–2429
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, Jr et al (2014) AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 64(21):e1–e76
Archer SL, James KE, Kvernen LR, Cohen IS, Ezekowitz MD, Gornick CC (1995) Role of transesophageal echocardiography in the detection of left atrial thrombus in patients with chronic nonrheumatic atrial fibrillation. Am Heart J 130(2):287–295
Caplan LR, D’Cruz I, Hier DB, Reddy H, Shah S (1986) Atrial size, atrial fibrillation, and stroke. Ann Neurol 19(2):158–161
Bernhardt P, Schmidt H, Hammerstingl C, Luderitz B, Omran H. (2005) Patients with atrial fibrillation and dense spontaneous echo contrast at high risk a prospective and serial follow-up over 12 months with transesophageal echocardiography and cerebral magnetic resonance imaging. J Am Coll Cardiol 45(11):1807–1812
Leung DY, Black IW, Cranney GB, Hopkins AP, Walsh WF (1994) Prognostic implications of left atrial spontaneous echo contrast in nonvalvular atrial fibrillation. J Am Coll Cardiol 24(3):755–762
Zabalgoitia M, Halperin JL, Pearce LA, Blackshear JL, Asinger RW, Hart RG (1998) Transesophageal echocardiographic correlates of clinical risk of thromboembolism in nonvalvular atrial fibrillation. Stroke Prevention in Atrial Fibrillation III Investigators. J Am Coll Cardiol 31(7):1622–1626
Saric M, Armour AC, Arnaout MS, Chaudhry FA, Grimm RA, Kronzon I et al (2016) Guidelines for the use of echocardiography in the evaluation of a cardiac source of embolism. J Am Soc Echocardiogr 29(1):1–42
Chen R, Wu X, Jin H, Wang B, Ma M, Zhao B. (2016) Assessment of left atrial appendage morphology and function in patients with non-valvular paroxysmal atrial fibrillation with different rhythms using real-time 3D transesophageal echocardiography. Ultrasound Med Biol 42(1):118–124
Klein AL, Grimm RA, Murray RD, Apperson-Hansen C, Asinger RW, Black IW et al (2001) Use of transesophageal echocardiography to guide cardioversion in patients with atrial fibrillation. N Engl J Med 344(19):1411–1420
Min JK, Spencer KT, Furlong KT, DeCara JM, Sugeng L, Ward RP et al (2005) Clinical features of complications from transesophageal echocardiography: a single-center case series of 10,000 consecutive examinations. J Am Soc Echocardiogr 18(9):925–929
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ (2001) Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. J Am Med Assoc 285(22):2864–2870
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 137(2):263–272
Watson T, Shantsila E, Lip GY (2009) Mechanisms of thrombogenesis in atrial fibrillation: Virchow’s triad revisited. Lancet 373(9658):155–166
Doukky R, Gage H, Nagarajan V, Demopoulos A, Cena M, Garcia-Sayan E et al (2013) B-type natriuretic Peptide predicts left atrial appendage thrombus in patients with nonvalvular atrial fibrillation. Echocardiography 30(8):889–895
Pant R, Patel M, Garcia-Sayan E, Wassouf M, D’Silva O, Kehoe RF et al (2016) Impact of B-type natriuretic peptide level on the risk of left atrial appendage thrombus in patients with nonvalvular atrial fibrillation: a prospective study. Cardiovasc Ultrasound 14(1):4
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22(2):107–133
Doukky R, Garcia-Sayan E, Gage H, Nagarajan V, Demopoulos A, Cena M et al (2014) The value of diastolic function parameters in the prediction of left atrial appendage thrombus in patients with nonvalvular atrial fibrillation. Cardiovasc ultrasound 12(1):10
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA. (1997) Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30(6):1527–1533
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29(4):277–314
Iwakura K, Okamura A, Koyama Y, Date M, Higuchi Y, Inoue K et al (2011) Effect of elevated left ventricular diastolic filling pressure on the frequency of left atrial appendage thrombus in patients with nonvalvular atrial fibrillation. Am J Cardiol 107(3):417–422
Doukky R, Garcia-Sayan E, Patel M, Pant R, Wassouf M, Shah S et al (2016) Impact of diastolic function parameters on the risk of left atrial appendage thrombus in patients with nonvalvular atrial fibrillation: a prospective study. J Am Soc Echocardiogr (in press)
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I et al (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57(6):450–458
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1):1–39.e14
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18(12):1440–1463
Aschenberg W, Schluter M, Kremer P, Schroder E, Siglow V, Bleifeld W (1986) Transesophageal two-dimensional echocardiography for the detection of left atrial appendage thrombus. J Am Coll Cardiol 7(1):163–166
Fatkin D, Herbert E, Feneley MP. (1994) Hematologic correlates of spontaneous echo contrast in patients with atrial fibrillation and implications for thromboembolic risk. Am J Cardiol 73(9):672–676
Puwanant S, Varr BC, Shrestha K, Hussain SK, Tang WH, Gabriel RS et al (2009) Role of the CHADS2 score in the evaluation of thromboembolic risk in patients with atrial fibrillation undergoing transesophageal echocardiography before pulmonary vein isolation. J Am Coll Cardiol 54(22):2032–2039
Wazni OM, Tsao HM, Chen SA, Chuang HH, Saliba W, Natale A et al (2006) Cardiovascular imaging in the management of atrial fibrillation. J Am Coll Cardiol 48(10):2077–2084
Lowe BS, Kusunose K, Motoki H, Varr B, Shrestha K, Whitman C et al (2014) Prognostic significance of left atrial appendage “sludge” in patients with atrial fibrillation: a new transesophageal echocardiographic thromboembolic risk factor. J Am Soc Echocardiogr 27(11):1176–1183
Hoyt H, Nazarian S, Alhumaid F, Dalal D, Chilukuri K, Spragg D et al (2011) Demographic profile of patients undergoing catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 22(9):994–998
Acknowledgments
The study was funded by a Rush-County collaborative research grant. The grant fiduciary was Rush University Medical Center; the principal investigator was Dr. Doukky. The funding source had no input into the study design, execution, data analysis and interpretation, or manuscript preparation and approval.
Disclosures
Dr. Doukky receives research funding from Astellas Pharma US and serves on the Advisory Board of Astellas Pharma US; none of these conflicts are relevant to the present work. Other authors report no conflicts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Garcia-Sayan, E., Patel, M., Wassouf, M. et al. Derivation and validation of E/e′ ratio as a parameter in the evaluation of left atrial appendage thrombus formation in patients with nonvalvular atrial fibrillation. Int J Cardiovasc Imaging 32, 1349–1356 (2016). https://doi.org/10.1007/s10554-016-0916-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-016-0916-y