Abstract
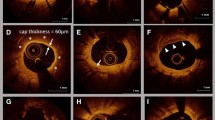
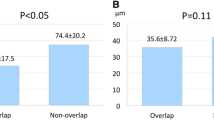
The consequences of acute strut malapposition in everolimus-eluting stents (EES) are unknown. This study investigated the impact of strut–vessel (S–V) distance and plaque type underneath acute strut malapposition on the mid-term vessel response in EES. Twenty-nine patients (35 EES) underwent optical coherence tomography (OCT) immediately after percutaneous coronary intervention and at 8-month follow-up. S–V distance and plaque type (lipid, calcified, or fibrous) underneath acute strut malapposition were evaluated. Follow-up OCT classified acute strut malapposition as persistent or resolved. The S–V cutoff value for predicting resolved strut malapposition and the incidence of intra-stent thrombi were determined. Among 569 cases of acute strut malapposition, involving 29,168 struts, 139 (24.4 %) were persistent. Mean S–V distance was significantly longer in persistent than in resolved strut malapposition (600 ± 294 vs. 231 ± 95 μm; P < 0.0001). S–V distance ≤380 μm was the best cutoff value for predicting resolved strut malapposition (sensitivity 93.5 %, specificity 69.8 %, area under curve 0.878). Acute strut malapposition with S–V distance ≤380 μm remained persistent more frequently over lipid/calcified than over fibrous plaques (lipid: 13.4 %, calcified: 18.2 %, fibrous: 4.2 %; lipid vs. fibrous, P = 0.001; calcified vs. fibrous, P = 0.02). Intra-stent thrombi were more frequent in stents with ≥1 persistent strut malapposition than in those without [4/11 stents (36.3 %) vs. 0/24 (0 %); P = 0.006]. Lipid and calcified plaque, together with S–V distance, affect the resolution of acute strut malapposition in EES. Persistent strut malapposition is associated with the presence of thrombi at follow-up, which could be the substrate for late stent thrombosis.






Similar content being viewed by others
References
Gonzalo N, Serruys PW, Okamura T, Shen ZJ, Onuma Y, Garcia-Garcia HM, Sarno G, Schultz C, van Geuns RJ, Ligthart J, Regar E (2009) Optical coherence tomography assessment of the acute effects of stent implantation on the vessel wall: a systematic quantitative approach. Heart 95(23):1913–1919. doi:10.1136/hrt.2009.172072
Kawamori H, Shite J, Shinke T, Otake H, Sawada T, Kato H, Miyoshi N, Yoshino N, Kozuki A, Hariki H, Inoue T, Hirata K (2010) The ability of optical coherence tomography to monitor percutaneous coronary intervention: detailed comparison with intravascular ultrasound. J Invasive Cardiol 22(11):541–545
Kume T, Okura H, Miyamoto Y, Yamada R, Saito K, Tamada T, Koyama T, Neishi Y, Hayashida A, Kawamoto T, Yoshida K (2012) Natural history of stent edge dissection, tissue protrusion and incomplete stent apposition detectable only on optical coherence tomography after stent implantation–preliminary observation. Circ J 76(3):698–703
Kawamori H, Shite J, Shinke T, Otake H, Matsumoto D, Nakagawa M, Nagoshi R, Kozuki A, Hariki H, Inoue T, Osue T, Taniguchi Y, Nishio R, Hiranuma N, Hirata KI (2013) Natural consequence of post-intervention stent malapposition, thrombus, tissue prolapse, and dissection assessed by optical coherence tomography at mid-term follow-up. Eur Heart J Cardiovasc Imaging. doi:10.1093/ehjci/jes299
Gutierrez-Chico JL, Wykrzykowska J, Nuesch E, van Geuns RJ, Koch KT, Koolen JJ, di Mario C, Windecker S, van Es GA, Gobbens P, Juni P, Regar E, Serruys PW (2012) Vascular tissue reaction to acute malapposition in human coronary arteries: sequential assessment with optical coherence tomography. Circ Cardiovasc Interv 5(1):20–29, S21–28. doi:10.1161/CIRCINTERVENTIONS.111.965301
Gonzalo N, Barlis P, Serruys PW, Garcia-Garcia HM, Onuma Y, Ligthart J, Regar E (2009) Incomplete stent apposition and delayed tissue coverage are more frequent in drug-eluting stents implanted during primary percutaneous coronary intervention for ST-segment elevation myocardial infarction than in drug-eluting stents implanted for stable/unstable angina: insights from optical coherence tomography. JACC Cardiovasc Interv 2(5):445–452. doi:10.1016/j.jcin.2009.01.012
Tu S, Holm NR, Koning G, Huang Z, Reiber JH (2011) Fusion of 3D QCA and IVUS/OCT. Int J Cardiovasc Imaging 27(2):197–207. doi:10.1007/s10554-011-9809-2
Inoue T, Shite J, Yoon J, Shinke T, Otake H, Sawada T, Kawamori H, Katoh H, Miyoshi N, Yoshino N, Kozuki A, Hariki H, Hirata K (2011) Optical coherence evaluation of everolimus-eluting stents 8 months after implantation. Heart 97(17):1379–1384. doi:10.1136/hrt.2010.204339
Tanigawa J, Barlis P, Di Mario C (2007) Intravascular optical coherence tomography: optimisation of image acquisition and quantitative assessment of stent strut apposition. EuroIntervention 3(1):128–136
Yabushita H, Bouma BE, Houser SL, Aretz HT, Jang IK, Schlendorf KH, Kauffman CR, Shishkov M, Kang DH, Halpern EF, Tearney GJ (2002) Characterization of human atherosclerosis by optical coherence tomography. Circulation 106(13):1640–1645
Guo N, Maehara A, Mintz GS, He Y, Xu K, Wu X, Lansky AJ, Witzenbichler B, Guagliumi G, Brodie B, Kellett MA Jr, Dressler O, Parise H, Mehran R, Stone GW (2010) Incidence, mechanisms, predictors, and clinical impact of acute and late stent malapposition after primary intervention in patients with acute myocardial infarction: an intravascular ultrasound substudy of the harmonizing outcomes with revascularization and stents in acute myocardial infarction (HORIZONS-AMI) trial. Circulation 122(11):1077–1084. doi:10.1161/CIRCULATIONAHA.109.906040
Jang IK, Tearney GJ, MacNeill B, Takano M, Moselewski F, Iftima N, Shishkov M, Houser S, Aretz HT, Halpern EF, Bouma BE (2005) In vivo characterization of coronary atherosclerotic plaque by use of optical coherence tomography. Circulation 111(12):1551–1555. doi:10.1161/01.CIR.0000159354.43778.69
Shimohama T, Ako J, Yamasaki M, Otake H, Tsujino I, Hasegawa T, Nakatani D, Sakurai R, Chang H, Kusano H, Waseda K, Honda Y, Stone GW, Saito S, Fitzgerald PJ, Sudhir K (2010) SPIRIT III JAPAN versus SPIRIT III USA: a comparative intravascular ultrasound analysis of the everolimus-eluting stent. Am J Cardiol 106(1):13–17. doi:10.1016/j.amjcard.2010.02.008
Ozaki Y, Okumura M, Ismail TF, Naruse H, Hattori K, Kan S, Ishikawa M, Kawai T, Takagi Y, Ishii J, Prati F, Serruys PW (2010) The fate of incomplete stent apposition with drug-eluting stents: an optical coherence tomography-based natural history study. Eur Heart J 31(12):1470–1476. doi:10.1093/eurheartj/ehq066
Jang IK, Bouma BE, Kang DH, Park SJ, Park SW, Seung KB, Choi KB, Shishkov M, Schlendorf K, Pomerantsev E, Houser SL, Aretz HT, Tearney GJ (2002) Visualization of coronary atherosclerotic plaques in patients using optical coherence tomography: comparison with intravascular ultrasound. J Am Coll Cardiol 39(4):604–609
Nakazawa G, Finn AV, Joner M, Ladich E, Kutys R, Mont EK, Gold HK, Burke AP, Kolodgie FD, Virmani R (2008) Delayed arterial healing and increased late stent thrombosis at culprit sites after drug-eluting stent placement for acute myocardial infarction patients: an autopsy study. Circulation 118(11):1138–1145. doi:10.1161/CIRCULATIONAHA.107.762047
Kubo T, Imanishi T, Kitabata H, Kuroi A, Ueno S, Yamano T, Tanimoto T, Matsuo Y, Masho T, Takarada S, Tanaka A, Nakamura N, Mizukoshi M, Tomobuchi Y, Akasaka T (2008) Comparison of vascular response after sirolimus-eluting stent implantation between patients with unstable and stable angina pectoris: a serial optical coherence tomography study. JACC Cardiovasc Imaging 1(4):475–484. doi:10.1016/j.jcmg.2008.03.012
Otake H, Shite J, Ako J, Shinke T, Tanino Y, Ogasawara D, Sawada T, Miyoshi N, Kato H, Koo BK, Honda Y, Fitzgerald PJ, Hirata K (2009) Local determinants of thrombus formation following sirolimus-eluting stent implantation assessed by optical coherence tomography. JACC Cardiovasc Interv 2(5):459–466. doi:10.1016/j.jcin.2009.03.003
Levin AD, Vukmirovic N, Hwang CW, Edelman ER (2004) Specific binding to intracellular proteins determines arterial transport properties for rapamycin and paclitaxel. Proc Natl Acad Sci U S A 101(25):9463–9467. doi:10.1073/pnas.0400918101
Kimura M, Mintz GS, Carlier S, Takebayashi H, Fujii K, Sano K, Yasuda T, Costa RA, Costa JR Jr, Quen J, Tanaka K, Lui J, Weisz G, Moussa I, Dangas G, Mehran R, Lansky AJ, Kreps EM, Collins M, Stone GW, Moses JW, Leon MB (2006) Outcome after acute incomplete sirolimus-eluting stent apposition as assessed by serial intravascular ultrasound. Am J Cardiol 98(4):436–442. doi:10.1016/j.amjcard.2006.02.050
Conflict of interest
No conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inoue, T., Shinke, T., Otake, H. et al. Impact of strut–vessel distance and underlying plaque type on the resolution of acute strut malapposition: serial optimal coherence tomography analysis after everolimus-eluting stent implantation. Int J Cardiovasc Imaging 30, 857–865 (2014). https://doi.org/10.1007/s10554-014-0422-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-014-0422-z