Abstract
Introduction
In Vietnam, 60% of men living with HIV smoke tobacco, and 92% of HIV-infected people who inject drugs (PWID) smoke tobacco. Tobacco use increases mortality through increased health risks including tuberculosis and malignancy in HIV-infected smokers. However, tobacco use treatment is not widely available in Vietnam. The objective was to examine current barriers and facilitators of smoking cessation and tobacco use treatment for HIV-infected PWID in Hanoi, Vietnam.
Methods
Native speaking ethnographers conducted semi-structured qualitative interviews about tobacco use and tobacco use treatment with sixteen HIV-infected PWID and eight healthcare providers, recruited from four HIV-Methadone Maintenance Treatment (MMT) clinics in Hanoi, Vietnam. Interviews were recorded, transcribed, and translated for thematic analysis in Dedoose.
Results
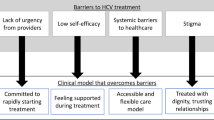
Clients and providers had learned the general health risks of smoking from public awareness campaigns. Half had tried to quit previously, often motivated by advice from family members but not by HIV providers’ advice. Almost all clients did not want to quit, citing the low price of tobacco, prevalence of smoking in Vietnam, and physical cravings. HIV provider’s counseling was brief, inconsistent, and limited by low provider knowledge and competing burdens of HIV and injection drug use. Providers recently trained by NGO-led seminars on tobacco prioritized tobacco use treatment.
Conclusions
Smoking cessation efforts for people living with HIV/AIDS (PLHA) and PWID smokers in Hanoi, Vietnam could benefit from further community public awareness campaigns, and exploring increased tobacco taxation. Tobacco use treatment at HIV clinics could benefit from involving family and friends in cessation, and training providers in treatment methods.
Similar content being viewed by others
References
WHO, Research for International Tobacco Control (2017) WHO report on the global tobacco epidemic (pp. volumes). Geneva: World Health Organization
United States. Department of Health and Human Services (US DHHS) (2000) Tracking healthy people 2010. U.S. Department of Health and Human Services, Washington, DC
Mdege ND, Shah S, Ayo-Yusuf OA, Hakim J, Siddiqi K (2017) Tobacco use among people living with HIV: analysis of data from Demographic and Health Surveys from 28 low-income and middle-income countries. Lancet Glob Health 5(6):e578–e592. https://doi.org/10.1016/S2214-109X(17)30170-5
Humfleet GL, Delucchi K, Kelley K, Hall SM, Dilley J, Harrison G (2009) Characteristics of HIV-positive cigarette smokers: a sample of smokers facing multiple challenges. AIDS Educ Prev 21(3 Suppl):54–64. https://doi.org/10.1521/aeap.2009.21.3_supp.54
Tesoriero JM, Gieryic SM, Carrascal A, Lavigne HE (2010) Smoking among HIV positive New Yorkers: prevalence, frequency, and opportunities for cessation. AIDS Behav 14(4):824–835. https://doi.org/10.1007/s10461-008-9449-2
Cohen MH, French AL, Benning L, Kovacs A, Anastos K, Young M et al (2002) Causes of death among women with human immunodeficiency virus infection in the era of combination antiretroviral therapy. Am J Med 113(2):91–98
Crothers K, Griffith TA, McGinnis KA, Rodriguez-Barradas MC, Leaf DA, Weissman S et al (2005) The impact of cigarette smoking on mortality, quality of life, and co-morbid illness among HIV-positive veterans. J Gen Intern Med 20(12):1142–1145. https://doi.org/10.1111/j.1525-1497.2005.0255.x
Feldman JG, Minkoff H, Schneider MF, Gange SJ, Cohen M, Watts DH et al (2006) Association of cigarette smoking with HIV prognosis among women in the HAART era: a report from the women’s interagency HIV study. Am J Public Health 96(6):1060–1065. https://doi.org/10.2105/AJPH.2005.062745
Fiore M (2008) United States. Tobacco Use and Dependence Guideline Panel. Treating tobacco use and dependence: 2008 update. U.S. Dept. of Health and Human Services, Rockville, MD
Helleberg M, Afzal S, Kronborg G, Larsen CS, Pedersen G, Pedersen C et al (2013) Mortality attributable to smoking among HIV-1-infected individuals: a nationwide, population-based cohort study. Clin Infect Dis 56(5):727–734. https://doi.org/10.1093/cid/cis933
Lewden C, Salmon D, Morlat P, Bevilacqua S, Jougla E, Bonnet F et al (2005) Causes of death among human immunodeficiency virus (HIV)-infected adults in the era of potent antiretroviral therapy: emerging role of hepatitis and cancers, persistent role of AIDS. Int J Epidemiol 34(1):121–130. https://doi.org/10.1093/ije/dyh307
Nguyen NP, Tran BX, Hwang LY, Markham CM, Swartz MD, Phan HT et al (2015) Prevalence of cigarette smoking and associated factors in a large sample of HIV-positive patients receiving antiretroviral therapy in Vietnam. PLoS ONE 10(2):e0118185. https://doi.org/10.1371/journal.pone.0118185
Nguyen NT, Tran BX, Hwang LY, Markham CM, Swartz MD, Vidrine JI et al (2016) Effects of cigarette smoking and nicotine dependence on adherence to antiretroviral therapy among HIV-positive patients in Vietnam. AIDS Care 28(3):359–364. https://doi.org/10.1080/09540121.2015.1090535
WHO (2016) Global Adult Tobacco Fact Sheet Vietnam 2015 [Internet]
VAAC (2017) Report of the first half 2017. Retrieved from Hanoi, Vietnam
Pool ERM, Dogar O, Lindsay RP, Weatherburn P, Siddiqi K (2016) Interventions for tobacco use cessation in people living with HIV and AIDS. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD011120.pub2
Hartmann-Boyce J, Lancaster T, Stead LF (2014) Print-based self-help interventions for smoking cessation. Cochrane Database Syst Rev 6:CD001118. https://doi.org/10.1002/14651858.CD001118.pub3
Bhuiyan J, Jonkman L, Connor S, Giannetti V (2017) Qualitative evaluation of perceptions of smoking cessation among clients at an alcohol and other drug treatment program. Res Soc Adm Pharm 13(6):1082–1089
Garner L, Ratschen E (2013) Tobacco smoking, associated risk behaviours, and experience with quitting: a qualitative study with homeless smokers addicted to drugs and alcohol. BMC Public Health 13:951
Twyman L, Bonevski B, Paul C, Bryant J (2014) Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open 4(12):e006414
McMaster C, Lee C (1991) Cognitive dissonance in tobacco smokers. Addict Behav 16(5):349–353
Oakes W, Chapman S, Borland R, Balmford J, Trotter L (2004) “Bulletproof skeptics in life’s jungle”: which self-exempting beliefs about smoking most predict lack of progression towards quitting? Prev Med 39(4):776–782. https://doi.org/10.1016/j.ypmed.2004.03.001
Saunders B, Sim J, Kingstone T et al (2018) Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 52(4):1893–1907
UN Office of Drugs and Crime (UNODC) (2017) Vietnam Country Programme, 2012–2017. Retrieved from Geneva
Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO (1991) The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom tolerance questionnaire. Br J Addict 86(9):1119–1127
Uppal N, Shahab L, Britton J, Ratschen E (2013) The forgotten smoker: a qualitative study of attitudes towards smoking, quitting, and tobacco control policies among continuing smokers. BMC Public Health 13:432. https://doi.org/10.1186/1471-2458-13-432
SocioCultural Research Consultants, LLC (2018) Dedoose Version 8.0.35, web application for managing, analyzing, and presenting qualitative and mixed method research data. www.dedoose.com
Hsieh HF, Shannon SE (2005) Three approaches to qualitative content analysis. Qual Health Res 15(9):1277–1288. https://doi.org/10.1177/1049732305276687
Minh HV, Ngan TT, Mai VQ, My NT, le Chung H, Kien VD et al (2016) Tobacco control policies in Vietnam: review on MPOWER implementation progress and challenges. Asian Pac J Cancer Prev 17(S1):1–9
Borland R, Balmford J (2003) Understanding how mass media campaigns impact on smokers. Tob Control 12(Suppl 2):45–52
Goldman LK, Glantz SA (1998) Evaluation of antismoking advertising campaigns. JAMA 279(10):772–777
Hohman ZP, Crano WD, Niedbala EM (2016) Attitude ambivalence, social norms, and behavioral intentions: developing effective anti-tobacco persuasive communications. Psychol Addict Behav 30(2):209–219. https://doi.org/10.1037/adb0000126
McVey D, Stapleton J (2000) Can anti-smoking television advertising affect smoking behaviour? Controlled trial of the Health Education Authority for England’s anti-smoking TV campaign. Tob Control 9(3):273–282
Burkhalter JE, Springer CM, Chhabra R, Ostroff JS, Rapkin BD (2005) Tobacco use and readiness to quit smoking in low-income HIV-infected persons. Nicotine Tob Res 7(4):511–522. https://doi.org/10.1080/14622200500186064
Reynolds NR, Neidig JL, Wewers ME (2004) Illness representation and smoking behavior: a focus group study of HIV-positive men. J Assoc Nurses AIDS Care 15(4):37–47. https://doi.org/10.1177/1055329003261969
Shiffman S, Pillitteri JL, Burton SL, Rohay JM, Gitchell JG (2001) Smokers’ beliefs about “Light” and “Ultra Light” cigarettes. Tob Control 10(Suppl 1):i17–i23. https://doi.org/10.1136/tc.10.suppl_1.i17
Borland R, Segan C, Velicer WF (2000) Testing the transtheoretical model for smoking change: victorian data. Aust J Psychol 52(2):83–88
DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS (1991) The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. J Consult Clin Psychol 59(2):295–304
Etter JF, Perneger TV (1999) Associations between the stages of change and the pros and cons of smoking in a longitudinal study of Swiss smokers. Addict Behav 24(3):419–424
Christakis NA, Fowler JH (2008) The collective dynamics of smoking in a large social network. N Engl J Med 358(21):2249–2258. https://doi.org/10.1056/NEJMsa0706154
Morrow M, Ngoc DH, Hoang TT, Trinh TH (2002) Smoking and young women in Vietnam: the influence of normative gender roles. Soc Sci Med 55(4):681–690
Tran DT, Kosik RO, Mandell GA, Chen YA, Su TP, Chiu AW, Fan AP (2013) Tobacco control in Vietnam. Public Health 127(2):109–118. https://doi.org/10.1016/j.puhe.2012.11.012
Tauras JA, Chaloupka FJ, Quah AC, Fong GT (2014) The economics of tobacco control: evidence from the International Tobacco Control (ITC) Policy Evaluation Project. Tob Control 23(Suppl 1):i1-3. https://doi.org/10.1136/tobaccocontrol-2014-051547
Carson KV, Verbiest ME, Crone MR et al. Training health professionals in smoking cessation. Cochrane Database Syst Rev 2012(5):CD000214
Gorin SS, Heck JE (2004) Meta-analysis of the efficacy of tobacco counseling by health care providers. Cancer Epidemiol Biomarkers Prev 13(12):2012–2022
Nguyen N, Nguyen T, Chapman J, Nguyen L, Kumar P, VanDevanter N, Shelley D (2017) Tobacco cessation in Vietnam: exploring the role of village health workers. Glob Public Health. https://doi.org/10.1080/17441692.2017.1360376
Burkhalter JE, Springer CM, Chhabra R, Ostroff JS, Rapkin BD (2005) Tobacco use and readiness to quit smoking in low-income HIV-infected persons. Nicotine Tob Res 7(4):511–522. https://doi.org/10.1080/14622200500186064
Mamary EM, Bahrs D, Martinez S (2002) Cigarette smoking and the desire to quit among individuals living with HIV. AIDS Patient Care STDS 16(1):39–42. https://doi.org/10.1089/108729102753429389
Webb MS, Vanable PA, Carey MP, Blair DC (2007) Cigarette smoking among HIV+ men and women: examining health, substance use, and psychosocial correlates across the smoking spectrum. J Behav Med 30(5):371–383. https://doi.org/10.1007/s10865-007-9112-9
Hser YI, McCarthy WJ, Anglin MD (1994) Tobacco use as a distal predictor of mortality among long-term narcotics addicts. Prev Med 23(1):61–69. https://doi.org/10.1006/pmed.1994.1009
Hurt RD, Offord KP, Croghan IT, Gomez-Dahl L, Kottke TE, Morse RM, Melton LJ III (1996) Mortality following inpatient addictions treatment. Role of tobacco use in a community-based cohort. JAMA 275(14):1097–1103
Funding
This work was supported by the Doris Duke Charitable Foundation through a grant supporting the Doris Duke International Clinical Research Fellows Program at The University of North Carolina at Chapel Hill. The Doris Duke Charitable Foundation did not have any role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chockalingam, L., Ha, T.V., Bui, Q. et al. Barriers and facilitators to smoking cessation among HIV-infected people who inject drugs (PWID) in Hanoi, Vietnam: a qualitative study. Cancer Causes Control 32, 391–399 (2021). https://doi.org/10.1007/s10552-021-01396-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-021-01396-3