Abstract
Purpose
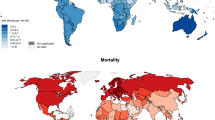
Most melanoma studies have been performed in the white population who exhibits the highest incidence rate due to their skin sensitivity to UV radiation. Previous publications have shown that young women (approximately under the menopausal age) exhibit higher incidence rates than men of the same age, and the causes are mostly attributed to their sun behavior or indoor tanning. In our recent publications, we suggested that higher risk in younger women was due to pathophysiological factors, such as hormonal impact, and thus this higher risk in young women should be shared across ethnicities regardless of their skin color or UV behavior.
Methods
A total of 13,208 non-white melanoma patients from SEER and 15,226 from WHO CI5-Plus were extracted for analysis. Age-specific incidence rates, female-to-male incidence rate ratios, and p values were calculated.
Results
As observed in the white population, younger women and older men showed higher melanoma incidence rates than their peers of the other gender in all ethnic groups. The highest female-to-male incidence rate ratios were observed in the pubescent and reproductive ages. Previously this gender discrepancy in the white population was attributed to the preference of skin tanning in young females. There is no evidence to show that darker-skinned young females adopt a similar tanning preference. Thus the age-dependent gender difference in the risk of melanoma is shared across ethnic groups and is perhaps independent of UV behavior.
Conclusions
Our results highlight the importance of gender as one of the melanoma risk factors beyond traditional UV radiation, which warrants further investigation and may provide a base for an improved prevention strategy.


Similar content being viewed by others
References
Czene K, Lichtenstein P, Hemminki K (2002) Environmental and heritable causes of cancer among 9.6 million individuals in the Swedish family-cancer database. Int J Cancer 99(2):260–266
Thomas NE et al (2010) Associations of cumulative sun exposure and phenotypic characteristics with histologic solar elastosis. Cancer Epidemiol Biomarkers Prev 19(11):2932–2941
Berwick M et al (2014) Sun exposure and melanoma survival: a GEM study. Cancer Epidemiol Biomarkers Prev 23(10):2145–2152
De Bock V et al (2014) Relations between erythemal UV dose, global solar radiation, total ozone column and aerosol optical depth at Uccle, Belgium. Atmos Chem Phys 14(22):12251–12270
Premi S et al (2015) Photochemistry. Chemiexcitation of melanin derivatives induces DNA photoproducts long after UV exposure. Science 347(6224):842–847
Hodi FS et al (2010) Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 363(8):711–723
Fajuyigbe D, Young AR (2016) The impact of skin colour on human photobiological responses. Pigment Cell Melanoma Res 29(6):607–618
Khavari PA (2006) Modelling cancer in human skin tissue. Nat Rev Cancer 6(4):270–280
Liu-Smith F et al (2015) Amyloids, melanins and oxidative stress in melanomagenesis. Exp Dermatol 24(3):171–174
Halliday GM (2010) Common links among the pathways leading to UV-induced immunosuppression. J Investig Dermatol 130(5):1209–1212
Liu-Smith F et al (2017) Sex differences in the association of cutaneous melanoma incidence rates and geographic ultraviolet light exposure. J Am Acad Dermatol 76(3):499–505 e3
CDC. Melanoma Incidence Rates and Death Rates by Race and Ethnicity. 1999–2012; Available from http://www.cdc.gov/cancer/skin/statistics/race.htm
SEER. Compare Statistics by Sex. 2016 September 12, 2016; Available from https://seer.cancer.gov/faststats/selections.php?#Output
Liu F et al (2013) A unique gender difference in early onset melanoma implies that in addition to ultraviolet light exposure other causative factors are important. Pigment Cell Melanoma Res 26(1):128–135
Lim HW et al (2011) Adverse effects of ultraviolet radiation from the use of indoor tanning equipment: time to ban the tan. J Am Acad Dermatol 64(4):e51–60
Vogel RI et al (2014) Exposure to indoor tanning without burning and melanoma risk by sunburn history. J Natl Cancer Inst 106(6):dju112
Wehner MR et al (2014) International prevalence of indoor tanning: a systematic review and meta-analysis. JAMA Dermatol 150(4):390–400
Roh MR et al (2015) Cutaneous melanoma in women. Int J Women Dermatol 1(1):21–25
Flowers JL et al (1987) Absence of estrogen receptor in human melanoma as evaluated by a monoclonal antiestrogen receptor antibody. Arch Dermatol 123(6):764–765
de Giorgi V et al (2011) Estrogens, estrogen receptors and melanoma. Expert Rev Anticancer Ther 11(5):739–747
Gori A et al (2016) Estrogen receptor (ER)beta expression and worse outcome from melanoma in pregnant and perimenopausal women. J Am Acad Dermatol 75(3):e117
Ribeiro MPC, Santos AE, Custodio JBA (2017) The activation of the G protein-coupled estrogen receptor (GPER) inhibits the proliferation of mouse melanoma K1735-M2 cells. Chem Biol Interact 277:176–184
Rajabi P, Bagheri M, Hani M (2017) Expression of Estrogen Receptor Alpha in Malignant Melanoma. Adv Biomed Res 6:14
Liu-Smith F, Ziogas A (2017) An age-dependent interaction between sex and geographical UV index in melanoma risk. J Am Acad Dermatol. https://doi.org/10.1016/j.jaad.2017.11.049
Gold EB (2011) The timing of the age at which natural menopause occurs. Obstet Gynecol Clin North Am 38(3):425–440
Boyle P, Parkin DM, Cancer registration: principles and methods. Statistical methods for registries. IARC Sci Publ 1991(95):126–158
Rothman KJ, Greenland S, Lash TL (2012) Modern Epidemiology. Lippincott Williams & Wilkins, Philadelphia
Altma DG (2015) Practical statistics for medical research, Chapman and Hall/CRC TextsStatistical Science Series, vol 12. Chapman and Hall, London.
NCI. Number of Persons by Race and Hispanic Ethnicity for SEER Participants. Available from https://seer.cancer.gov/registries/data.html
Coelho SG, Hearing VJ (2009) UVA tanning is involved in the increased incidence of skin cancers in fair-skinned young women. Pigment Cell Melanoma Res 23(1):57–63
Hausauer AK et al (2011) Increases in melanoma among adolescent girls and young women in California: trends by socioeconomic status and UV radiation exposure. Arch Dermatol 147(7):783–789
Coelho SG, Hearing VJ (2010) UVA tanning is involved in the increased incidence of skin cancers in fair-skinned young women. Pigment Cell Melanoma Res 23(1):57–63
Doll R, Peto R (1981) The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. Oxford University Press, Oxford, pp 1197–1312
Sambandan DR, Ratner D (2011) Sunscreens: an overview and update. J Am Acad Dermatol 64(4):748–758
Holman DM et al (2015) Patterns of sunscreen use on the face and other exposed skin among US adults. J Am Acad Dermatol 73(1):83–92 e1
Aviles-Izquierdo JA et al (2016) Who detects melanoma? Impact of detection patterns on characteristics and prognosis of patients with melanoma. J Am Acad Dermatol. https://doi.org/10.1016/j.jaad.2016.07.009
Chen J et al (2016) Gender-based differences and barriers in skin protection behaviors in melanoma survivors. J Skin Cancer 2016:3874572
Cheung MR (2013) Using SEER data to quantify effects of low income neighborhoods on cause specific survival of skin melanoma. Asian Pac J Cancer Prev 14(5):3219–3221
Stensheim H et al (2009) Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: a registry-based cohort study. J Clin Oncol 27(1):45–51
Costin GE, Hearing VJ (2007) Human skin pigmentation: melanocytes modulate skin color in response to stress. FASEB J 21(4):976–994
Scoggins CR et al (2006) Gender-related differences in outcome for melanoma patients. Ann Surg 243(5):693–698 (discussion 698–700)
Buller DB et al (2011) Prevalence of sunburn, sun protection, and indoor tanning behaviors among Americans: review from national surveys and case studies of 3 states. J Am Acad Dermatol 65(5 Suppl 1):S114–S123
Sondak VK, Swetter SM, Berwick MA (2012) Gender disparities in patients with melanoma: breaking the glass ceiling. J Clin Oncol 30(18):2177–2178
Dika E et al (2017) Oestrogen and progesterone receptors in melanoma and nevi: an immunohistochemical study. Eur J Dermatol 27(3):254–259
Elling SV, Powell FC (1997) Physiological changes in the skin during pregnancy. Clin Dermatol 15(1):35–43
Glatthaar H et al (2016) Estrogen receptor alpha (ESR1) single-nucleotide polymorphisms (SNPs) affect malignant melanoma susceptibility and disease course. Genet Epigenet 8:1–6
Merrill RM, Pace ND, Elison AN (2010) Cutaneous malignant melanoma among White Hispanics and Non-Hispanics in the United States. Ethn Dis 20(4):353–358
Gonzalez Burchard E et al (2005) Latino populations: a unique opportunity for the study of race, genetics, and social environment in epidemiological research. Am J Public Health 95(12):2161–2168
Ziegler RG et al (1993) Migration patterns and breast cancer risk in Asian-American women. J Natl Cancer Inst 85(22):1819–1827
Acknowledgments
This study is supported by a collaborative Grant to FLS, jointly by MRA(#509278), UCI Melanoma Center (Dr. James Jakowatz), UCI Chao Family Comprehensive Cancer Center (Dr. Richard Van Etten, NCI P30 CA062203), and by a NCI/NIH K07 Grant to FLS (CA 160756). TAY is supported by the UCI Public Health Graduate Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflicts of interest.
Rights and permissions
About this article
Cite this article
Yuan, TA., Meyskens, F. & Liu-Smith, F. A cancer registry-based analysis on the non-white populations reveals a critical role of the female sex in early-onset melanoma. Cancer Causes Control 29, 405–415 (2018). https://doi.org/10.1007/s10552-018-1022-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-018-1022-3