Abstract
Purpose
Breast cancer surgical techniques are evolving. Few studies have analyzed national trends for the multitude of surgical options that include partial mastectomy (PM), mastectomy without reconstruction (M), mastectomy with reconstruction (M+R), and PM with oncoplastic reconstruction (OS). We hypothesize that the use of M is declining and likely correlates with the rise of surgery with reconstructive options (M+R, OS).
Methods
A retrospective cohort analysis was conducted using the ACS-NSQIP database from 2005 to 2016 and ICD codes for IBC and DCIS. Patients were then grouped together based on current procedural terminology (CPT) codes for PM, M, M+R, and OS. In each group, categories were sorted again based on additional reconstructive procedures. Data analysis was conducted via Pearson’s chi-squared test for demographics, linear regression, and a non-parametric Mann- Kendall test to assess a temporal trend.
Results
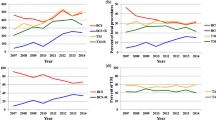
The patient cohort consisted of 256,398 patients from the NSQIP data base; 197,387 meet inclusion criteria diagnosed with IBC or DCIS. Annual breast surgery trends changed as follows: PM 46.3–46.1% (p = 0.21), M 35.8–26.4% (p = 0.001), M+R 15.9–23.0% (p = 0.03), and OS 1.8–4.42% (p = 0.001). Analyzing the patient cohort who underwent breast conservation, categorical analysis showed a decreased use of PM alone (96–91%) with an increased use of OS (4–9%). For the patient cohort undergoing mastectomy, M alone decreased (69–53%); M+R with muscular flap decreased (9–2%); and M+R with implant placement increased (20–40%)—all three trends p < 0.0001.
Conclusion
The modern era of breast surgery is identified by the increasing use of reconstruction for patients undergoing breast conservation (in the form of OS) and mastectomy (in the form of M+R). Our study provides data showing significant trends that will impact the future of both breast cancer surgery and breast training programs.


Similar content being viewed by others
Abbreviations
- BCT:
-
Breast conservative therapy
- IBC:
-
Invasive breast cancer
- DCIS:
-
Ductal carcinoma in situ
- PM:
-
Partial mastectomy
- M:
-
Mastectomy
- M+R:
-
Mastectomy with reconstruction
- OS:
-
Oncoplastic surgery
- M+I:
-
Mastectomy with breast prosthesis, delayed- insertion or tissue expander for implant placement
- M+MF:
-
Mastectomy with muscular flap
- SLNB:
-
Sentinel lymph node biopsy
- ALND:
-
Axillary lymph node dissection
- SS:
-
Sen’s slope
- R 2 :
-
Linear regression
- ACS:
-
American College of Surgeons
- NSQIP:
-
National Surgical Quality Improvement Program
- CPT:
-
Current procedural terminology
- ICD-9:
-
International classification of diseases ninth revision
- CG:
-
Categories
References
Research AIfC. https://www.wcrf.org/dietandcancer/cancer-trends/worldwide-cancer-data
The L (2018) GLOBOCAN 2018: counting the toll of cancer. Lancet 392(10152):985. https://doi.org/10.1016/S0140-6736(18)32252-9
Registries NAAoCC (2018) Online cancer database. NAACCR partners and sponsors. https://www.naaccr.org/interactive-data-on-line/. Accessed 8/15/2018 2018
Kelsall JE, McCulley SJ, Brock L, Akerlund MTE, Macmillan RD Comparing oncoplastic breast conserving surgery with mastectomy and immediate breast reconstruction: Case-matched patient reported outcomes. J Plast Reconstr Aesthet Surg. https://doi.org/10.1016/j.bjps.2017.05.009
De Lorenzi F, Loschi P, Bagnardi V, Rotmensz N, Hubner G, Mazzarol G, Orecchia R, Galimberti V, Veronesi P, Colleoni MA, Toesca A, Peradze N, Mario R Oncoplastic breast-conserving surgery for tumors larger than 2 centimeters: Is it oncologically safe? A matched-cohort analysis. Ann Surg Oncol 23 (6):1852–1859. https://doi.org/10.1245/s10434-016-5124-4
Kimball CC, Nichols CI, Vose JG, Peled AW (2018) Trends in lumpectomy and oncoplastic breast-conserving surgery in the US, 2011–2016. Ann Surg Oncol. https://doi.org/10.1245/s10434-018-6760-7
Chauhan A, Sharma MM, Kumar K (2016) Evaluation of surgical outcomes of oncoplasty breast surgery in locally advanced breast cancer and comparison with conventional breast conservation surgery. Indian J Surg Oncol 7(4):413–419. https://doi.org/10.1007/s13193-016-0549-6
Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA (2015) Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg 150(1):9–16. https://doi.org/10.1001/jamasurg.2014.2895
Wong SM, Freedman RA, Sagara Y, Aydogan F, Barry WT, Golshan M (2017) Growing use of contralateral prophylactic mastectomy despite no improvement in long-term survival for invasive breast cancer. Ann Surg 265(3):581–589. https://doi.org/10.1097/sla.0000000000001698
Albornoz CR, Matros E, Lee CN, Hudis CA, Pusic AL, Elkin E, Bach PB, Cordeiro PG, Morrow M (2015) Bilateral mastectomy versus breast-conserving surgery for early-stage breast cancer: the role of breast reconstruction. Plast Reconstr Surg 135(6):1518–1526. https://doi.org/10.1097/prs.0000000000001276
Lautner M, Lin H, Shen Y, Parker C, Kuerer H, Shaitelman S, Babiera G, Bedrosian I (2015) Disparities in the use of breast-conserving therapy among patients with early-stage breast cancer. JAMA Surgery 150(8):778–786. https://doi.org/10.1001/jamasurg.2015.1102
Carter SA, Lyons GR, Kuerer HM, Bassett RL Jr, Oates S, Thompson A, Caudle AS, Mittendorf EA, Bedrosian I, Lucci A, DeSnyder SM, Babiera G, Yi M, Baumann DP, Clemens MW, Garvey PB, Hunt KK, Hwang RF (2016) Operative and oncologic outcomes in 9861 patients with operable breast cancer: single-institution analysis of breast conservation with oncoplastic reconstruction. Ann Surg Oncol 23(10):3190–3198. https://doi.org/10.1245/s10434-016-5407-9
Albornoz CR, Bach PB, Mehrara BJ, Disa JJ, Pusic AL, McCarthy CM, Cordeiro PG, Matros E (2013) A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg 131(1):15–23. https://doi.org/10.1097/PRS.0b013e3182729cde
Jeevan R, Mennie JC, Mohanna PN, O’Donoghue JM, Rainsbury RM, Cromwell DA (2016) National trends and regional variation in immediate breast reconstruction rates. Br J Surg 103(9):1147–1156. https://doi.org/10.1002/bjs.10161
Surgeons, ACo (2018) ACS national surgical quality improvement program. ACS. Accessed 8/1/2018
Chatterjee A, Gass J, Burke MB, Kopkash K, El-Tamer MB, Holmes DR, Clark P, Reiland J (2018) Results from the American Society of Breast Surgeons Oncoplastic Surgery Committee 2017 survey: current practice and future directions. Ann Surg Oncol. https://doi.org/10.1245/s10434-018-6586-3
Liang Y, Naber SP, Chatterjee A (2018) Anatomic and terminological description and processing of breast pathologic specimens from oncoplastic large volume displacement surgeries. Mod Pathol 31:1004–1011
Losken A, Hart AM, Broecker JS, Styblo TM, Carlson GW (2017) Oncoplastic breast reduction technique and outcomes: an evolution over 20 years. Plast Reconstr Surg 139(4):824e–833e. https://doi.org/10.1097/prs.0000000000003226
Bazzarelli A, Zhang J, Arnaout A (2016) Patient-reported satisfaction following oncoplastic breast-conserving therapy. In: The American Society of Breast Surgeons Annual Meeting, Dallas, Texas, 4/13/2016
Chand ND, Browne V, Paramanathan N, Peiris LJ, Laws SA, Rainsbury RM (2017) Patient-reported outcomes are better after oncoplastic breast conservation than after mastectomy and autologous reconstruction. Plast Reconstr Surg 5(7):e1419. https://doi.org/10.1097/gox.0000000000001419
Cil TD, Cordeiro E (2016) Complications of oncoplastic breast surgery involving soft tissue transfer versus breast-conserving surgery: an analysis of the NSQIP database. Ann Surg Oncol 23(10):3266–3271. https://doi.org/10.1245/s10434-016-5477-8
Elston JB, Prabhakaran S, Lleshi A, Castillo B, Sun W, Kumar A, Ma Z, Smith PD, Dayicioglu D (2017) Complications and recurrence in implant-sparing oncologic breast surgery. Ann Plast Surg 78(6S Suppl 5):S269–S274. https://doi.org/10.1097/SAP.0000000000001039
Chatterjee A, II ACO, Asban A, Minasian RA, Losken A, Graham R, Chen L, Czerniecki BJ, Fisher C (2018) A cost-utility analysis comparing oncoplastic breast surgery to standard lumpectomy in large breasted women. Adv Breast Cancer Res 07(02):14. https://doi.org/10.4236/abcr.2018.72011
Asban A, Homsy C, Chen L, Fisher C, Losken A, Chatterjee A (2018) A cost-utility analysis comparing large volume displacement oncoplastic surgery to mastectomy with single stage implant reconstruction in the treatment of breast cancer. Breast 41:159–164. https://doi.org/10.1016/j.breast.2018.07.012
Tan MP (2016) Is there an ideal breast conservation rate for the treatment of breast cancer? Ann Surg Oncol 23(9):2825–2831. https://doi.org/10.1245/s10434-016-5267-3
De Lorenzi F, Hubner G, Rotmensz N, Bagnardi V, Loschi P, Maisonneuve P, Venturino M, Orecchia R, Galimberti V, Veronesi P, Rietjens M (2015) Oncological results of oncoplastic breast-conserving surgery: Long term follow-up of a large series at a single institution: a matched-cohort analysis. Eur J Surg Oncol 42(1):71–77. https://doi.org/10.1016/j.ejso.2015.08.160
Acknowledgements
The ACS-NSQIP is not responsible for the statistical validity of the data analysis or the conclusions derived by the authors. The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, Award Number TL1TR002546. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors. This article does not contain any studies with human participants performed by any of the authors.
Informed consent
The study was reviewed and deemed exempt by Tufts Medical Center Institutional Review Board, given ACS NSQIP database was a de-identified data set. No individual participant consent was required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jonczyk, M.M., Jean, J., Graham, R. et al. Surgical trends in breast cancer: a rise in novel operative treatment options over a 12 year analysis. Breast Cancer Res Treat 173, 267–274 (2019). https://doi.org/10.1007/s10549-018-5018-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-5018-1