Abstract
Background
Metaplastic breast cancer (MpBC) is a rare histological subtype of breast cancer recognized as a unique pathologic entity in 2000. However, the pathogenesis, optimal therapy, and prognosis of MpBC and the potential effect of systemic treatments on different subtypes of MpBC are not well defined.
Methods
A retrospective population-based study was performed to identify breast cancer patients with MpBC and other triple-negative breast cancers (TNBC) between 2010 and 2014 using the surveillance, Epidemiology, and End Results (SEER) database. Chi-square test was used to analyze characteristics between subgroups. Kaplan–Meier analysis and Multivariate Cox regressions were used to evaluate overall survival (OS) of MpBC, TNBC, and MpBC subgroups. Competing risk analysis and multivariate regression model of competing risk were used to assess breast cancer-specific survival (BCSS) of MpBC and TNBC
Results
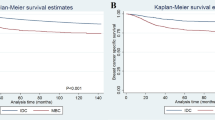
We identified a study cohort of 22,433 patients (1112 MpBC and 21,321 TNBC). MpBC correlated with older population, larger tumor size and less lymph node involvement, and TNBC phenotype. Patients with MpBC especially with triple-negative subtype (TN-MpBC) had worse survival than the overall TNBC population. However, the prognosis of MpBC without triple-negative subtype (non-TN MpBC) was not different from that of TNBC. In Kaplan–Meier analysis, chemotherapy was not associated with significant difference in OS of TN-MpBC. In non-TN MpBC group, the 3-year OS was 79.8% for patients receiving chemotherapy and 70.5% in patients without chemotherapy, and chemotherapy was associated (P = 0.033) with improved OS. Within the MpBC patients, radiotherapy was significantly (HR 1.544; 95% CI 1.148–2.078; P = 0.004) associated with improved OS and (HR 1.474; 95% CI 1.067–2.040; P = 0.019) BCSS.
Conclusions
Patients with TN-MpBC had worse prognosis than TNBC and chemotherapy was not associated with improved survival. In contrast, non-TN MpBC may derive survival benefit from chemotherapy and radiotherapy.



Similar content being viewed by others

Abbreviations
- MpBC:
-
Metaplastic breast cancer
- TNBC:
-
Triple-negative breast cancer
- SEER:
-
Surveillance, Epidemiology, and End Results
- OS:
-
Overall survival
- BCSS:
-
Breast cancer-specific survival
- TN-MpBC:
-
Triple-negative subtype of MpBC
- Non-TN MpBC:
-
MpBC without triple-negative subtype
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- IDC:
-
Invasive ductal carcinoma, no special type
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- HER2:
-
Human epidermal growth factor receptor 2
- ICD-0-3:
-
International Classification of Diseases for Oncology Version 3
- TNBC:
-
Triple-negative subtype of IDC
- CT:
-
Chemotherapy
- RT:
-
Radiotherapy
References
Oberman HA (1987) Metaplastic carcinoma of the breast. A clinicopathologic study of 29 patients. Am J Surg Pathol 11:918–929. https://doi.org/10.1097/00000478-198712000-00002
Tavassoli FA (1992) Classification of metaplastic carcinomas of the breast. Pathol Annu 27(Pt 2):89–119
Lee H, Jung SY, Ro JY, Kwon Y, Sohn JH, Park IH, Lee KS, Lee S, Kim SW, Kang HS, Ko KL, Ro J (2012) Metaplastic breast cancer: clinicopathological features and its prognosis. J Clin Pathol 65:441–446. https://doi.org/10.1136/jclinpath-2011-200586
Li CI, Anderson BO, Daling JR, Moe RE (2003) Trends in incidence rates of invasive lobular and ductal breast carcinoma. JAMA 289:1421–1424
Park HS, Park S, Kim JH, Lee JH, Choi SY, Park BW, Lee KS (2010) Clinicopathologic features and outcomes of metaplastic breast carcinoma: comparison with invasive ductal carcinoma of the breast. Yonsei medical journal 51:864–869. https://doi.org/10.3349/ymj.2010.51.6.864
Dieci MV, Orvieto E, Dominici M, Conte P, Guarneri V (2014) Rare breast cancer subtypes: histological, molecular, and clinical peculiarities. Oncologist 19:805–813. https://doi.org/10.1634/theoncologist.2014-0108
Haffty BG, Yang Q, Reiss M, Kearney T, Higgins SA, Weidhaas J, Harris L, Hait W, Toppmeyer D (2006) Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol 24:5652–5657. https://doi.org/10.1200/JCO.2006.06.5664
Rayson D, Adjei AA, Suman VJ, Wold LE, Ingle JN (1999) Metaplastic breast cancer: prognosis and response to systemic therapy. Ann Oncol 10:413–419
Dave B, Gonzalez DD, Liu ZB, Li X, Wong H, Granados S, Ezzedine NE, Sieglaff DH, Ensor JE, Miller KD, Radovich M, KarinaEtrovic A, Gross SS, Elemento O, Mills GB, Gilcrease MZ, Chang JC (2017) Role of RPL39 in metaplastic breast cancer. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djw292
Jung SY, Kim HY, Nam BH, Min SY, Lee SJ, Park C, Kwon Y, Kim EA, Ko KL, Shin KH, Lee KS, Park IH, Lee S, Kim SW, Kang HS, Ro J (2010) Worse prognosis of metaplastic breast cancer patients than other patients with triple-negative breast cancer. Breast Cancer Res Treat 120:627–637. https://doi.org/10.1007/s10549-010-0780-8
Luini A, Aguilar M, Gatti G, Fasani R, Botteri E, Brito JA, Maisonneuve P, Vento AR, Viale G (2007) Metaplastic carcinoma of the breast, an unusual disease with worse prognosis: the experience of the European Institute of Oncology and review of the literature. Breast Cancer Res Treat 101:349–353. https://doi.org/10.1007/s10549-006-9301-1
Lai HW, Tseng LM, Chang TW, Kuo YL, Hsieh CM, Chen ST, Kuo SJ, Su CC, Chen DR (2013) The prognostic significance of metaplastic carcinoma of the breast (MCB)—a case controlled comparison study with infiltrating ductal carcinoma. Breast 22:968–973. https://doi.org/10.1016/j.breast.2013.05.010
Barquet-Munoz SA, Villarreal-Colin SP, Herrera-Montalvo LA, Soto-Reyes E, Perez-Plasencia C, Coronel-Martinez J, Perez-Montiel D, Vazquez-Romo R, Cantu de Leon D (2015) Metaplastic breast cancer: a comparison between the most common histologies with poor immunohistochemistry factors. BMC Cancer 15:75. https://doi.org/10.1186/s12885-015-1079-2
McKinnon E, Xiao P (2015) Metaplastic carcinoma of the breast. Arch Pathol Lab Med 139:819–822. https://doi.org/10.5858/arpa.2013-0358-RS
Nelson RA, Guye ML, Luu T, Lai LL (2015) Survival outcomes of metaplastic breast cancer patients: results from a US population-based analysis. Annals of surgical oncology 22:24–31. https://doi.org/10.1245/s10434-014-3890-4
Lester TR, Hunt KK, Nayeemuddin KM, Bassett RL Jr, Gonzalez-Angulo AM, Feig BW, Huo L, Rourke LL, Davis WG, Valero V, Gilcrease MZ (2012) Metaplastic sarcomatoid carcinoma of the breast appears more aggressive than other triple receptor-negative breast cancers. Breast Cancer Res Treat 131:41–48. https://doi.org/10.1007/s10549-011-1393-6
Surveillance, Epidemiology, and End Results (SEER) Program Research Data (1973–2014), National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released March 2017, based on the November 2016 submission. http://www.seer.cancer.gov (Accessed 23 Mar 2017)
Scrucca L, Santucci A, Aversa F (2007) Competing risk analysis using R: an easy guide for clinicians. Bone Marrow Transpl 40:381–387. https://doi.org/10.1038/sj.bmt.1705727
Scrucca L, Santucci A, Aversa F (2010) Regression modeling of competing risk using R: an in depth guide for clinicians. Bone Marrow Transpl 45:1388–1395. https://doi.org/10.1038/bmt.2009.359
Rakha EA, Coimbra ND, Hodi Z, Juneinah E, Ellis IO, Lee AH (2017) Immunoprofile of metaplastic carcinomas of the breast. Histopathology 70:975–985. https://doi.org/10.1111/his.13159
Pezzi CM, Patel-Parekh L, Cole K, Franko J, Klimberg VS, Bland K (2007) Characteristics and treatment of metaplastic breast cancer: analysis of 892 cases from the National Cancer Data Base. Ann Surg Oncol 14:166–173. https://doi.org/10.1245/s10434-006-9124-7
Rugo HS, Olopade OI, DeMichele A, Yau C, van ‘t Veer LJ, Buxton MB, Hogarth M, Hylton NM, Paoloni M, Perlmutter J, Symmans WF, Yee D, Chien AJ, Wallace AM, Kaplan HG, Boughey JC, Haddad TC, Albain KS, Liu MC, Isaacs C, Khan QJ, Lang JE, Viscusi RK, Pusztai L, Moulder SL, Chui SY, Kemmer KA, Elias AD, Edmiston KK, Euhus DM, Haley BB, Nanda R, Northfelt DW, Tripathy D, Wood WC, Ewing C, Schwab R, Lyandres J, Davis SE, Hirst GL, Sanil A, Berry DA, Esserman LJ, Investigators IS (2016) Adaptive randomization of veliparib-carboplatin treatment in breast cancer. N Engl J Med 375:23–34. https://doi.org/10.1056/NEJMoa1513749
Montagna E, Maisonneuve P, Rotmensz N, Cancello G, Iorfida M, Balduzzi A, Galimberti V, Veronesi P, Luini A, Pruneri G, Bottiglieri L, Mastropasqua MG, Goldhirsch A, Viale G, Colleoni M (2013) Heterogeneity of triple-negative breast cancer: histologic subtyping to inform the outcome. Clin Breast Cancer 13:31–39. https://doi.org/10.1016/j.clbc.2012.09.002
Tseng WH, Martinez SR (2011) Metaplastic breast cancer: to radiate or not to radiate? Ann Surg Oncol 18:94–103. https://doi.org/10.1245/s10434-010-1198-6
Schroeder MC, Rastogi P, Geyer CE Jr, Miller LD, Thomas A (2018) Early and locally advanced metaplastic breast cancer: presentation and survival by receptor status in surveillance, epidemiology, and end results (SEER) 2010–2014. Oncologist. https://doi.org/10.1634/theoncologist.2017-0398
Hennessy BT, Gonzalez-Angulo AM, Stemke-Hale K, Gilcrease MZ, Krishnamurthy S, Lee JS, Fridlyand J, Sahin A, Agarwal R, Joy C, Liu W, Stivers D, Baggerly K, Carey M, Lluch A, Monteagudo C, He X, Weigman V, Fan C, Palazzo J, Hortobagyi GN, Nolden LK, Wang NJ, Valero V, Gray JW, Perou CM, Mills GB (2009) Characterization of a naturally occurring breast cancer subset enriched in epithelial-to-mesenchymal transition and stem cell characteristics. Cancer Res 69:4116–4124. https://doi.org/10.1158/0008-5472.CAN-08-3441
Taube JH, Herschkowitz JI, Komurov K, Zhou AY, Gupta S, Yang J, Hartwell K, Onder TT, Gupta PB, Evans KW, Hollier BG, Ram PT, Lander ES, Rosen JM, Weinberg RA, Mani SA (2010) Core epithelial-to-mesenchymal transition interactome gene-expression signature is associated with claudin-low and metaplastic breast cancer subtypes. Proc Natl Acad Sci USA 107:15449–15454. https://doi.org/10.1073/pnas.1004900107
Yang C, Lu W, Lin T, You P, Ye M, Huang Y, Jiang X, Wang C, Wang F, Lee MH, Yeung SC, Johnson RL, Wei C, Tsai RY, Frazier ML, McKeehan WL, Luo Y (2013) Activation of Liver FGF21 in hepatocarcinogenesis and during hepatic stress. BMC Gastroenterol 13:67. https://doi.org/10.1186/1471-230X-13-67
Prat A, Parker JS, Karginova O, Fan C, Livasy C, Herschkowitz JI, He X, Perou CM (2010) Phenotypic and molecular characterization of the claudin-low intrinsic subtype of breast cancer. Breast Cancer Res 12:R68. https://doi.org/10.1186/bcr2635
Sabatier R, Finetti P, Guille A, Adelaide J, Chaffanet M, Viens P, Birnbaum D, Bertucci F (2014) Claudin-low breast cancers: clinical, pathological, molecular and prognostic characterization. Mol Cancer 13:228. https://doi.org/10.1186/1476-4598-13-228
Theriault RL, Carlson RW, Allred C, Anderson BO, Burstein HJ, Edge SB, Farrar WB, Forero A, Giordano SH, Goldstein LJ, Gradishar WJ, Hayes DF, Hudis CA, Isakoff SJ, Ljung BM, Mankoff DA, Marcom PK, Mayer IA, McCormick B, Pierce LJ, Reed EC, Schwartzberg LS, Smith ML, Soliman H, Somlo G, Ward JH, Wolff AC, Zellars R, Shead DA, Kumar R, National Comprehensive Cancer N (2013) Breast cancer, version 3.2013: featured updates to the NCCN guidelines. J Natl Compr Cancer Netw 11:753–760; quiz 761
Acknowledgements
Dr. F. Esteva is partially supported by Breast Cancer Research Foundation. Dr. S. Yeung is partially supported by DepoMed, Inc. and Bristol-Myers Squibb. The University of Texas MD Anderson Cancer Center is supported in part by the National Institutes of Health through Cancer Center Support Grant P30 CA016672.
Funding
No funding is specific for this project.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Dr. Yeung is the principal investigator of an investigator-initiated clinical trial supported by DepoMed and a retrospective clinical study supported by Bristol-Myer Squibb through ARISTA-USA (BMS/Pfizer American Thrombosis Investigator Initiated Research Program). The support granted by commercial companies was not used in support of the current study. All other authors declare no competing financial or non-financial interests.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, X., Ji, J., Dong, R. et al. Prognosis in different subtypes of metaplastic breast cancer: a population-based analysis. Breast Cancer Res Treat 173, 329–341 (2019). https://doi.org/10.1007/s10549-018-5005-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-5005-6