Abstract
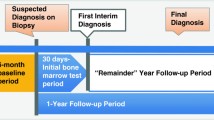
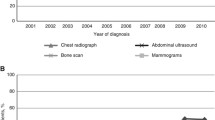
Current National Comprehensive Cancer Network guidelines for breast cancer staging include pre-treatment complete blood count (CBC) and liver function tests (LFT) to screen for occult metastatic disease. To date, the relevance of these tests in detecting metastatic disease in asymptomatic women with early-stage breast cancer (Stage I/II) has not been demonstrated. Although chest x-rays are no longer recommended in the NCCN guidelines, many centers continue to include this imaging as part of their screening process. We aim to determine the clinical and financial impact of these labs and x-rays in the evaluation of early-stage breast cancer patients. A single institution IRB-approved retrospective chart review was conducted of patients with biopsy-proven invasive breast cancer treated from January 1, 2005–December 31, 2009. We collected patient demographics, clinical and pathologic staging, chest x-ray, CBC, and LFT results at the time of referral. Patients were stratified according to radiographic stage at the time of diagnosis. We obtained Medicare reimbursement fees for cost analysis. From 2005 to 2009, 1609 patients with biopsy-proven invasive breast cancer were treated at our institution. Of the 1082 patients with radiographic stage I/II disease, 27.3 % of patients had abnormal CBCs. No additional testing was performed to evaluate these abnormalities. In the early-stage population, 24.7 % of patients had elevated LFTs, resulting in 84 additional imaging studies. No metastatic disease was detected. The cost of CBC, LFTs and chest x-rays was $110.20 per patient, totaling $106,410.99. Additional tests prompted by abnormal results cost $58,143.30 over the five-year period. We found that pre-treatment CBCs, LFTs, and chest x-rays did not improve detection of occult metastatic disease but resulted in additional financial costs. Avoiding routine ordering of these tests would save the US healthcare system $25.7 million annually.

Similar content being viewed by others
References
Howlander N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF (2014) SEER cancer statistics review, 1975–2011. Bethesda, MD: National cancer institute. Available from: http://seer.cancer.gov/csr/1975_2011/. Accessed 7 April 2015
Gradishar WJ, Anderson BO, Blair SL, Burstein HJ, Cyr A, Elias AD et al (2014) Breast cancer version 3.2014. J Natl Compr Cancer Netw 12(4):542–590
Chen EA, Carlson GA, Coughlin BF, Reed WP, Garb JL, Frank JL (2000) Routine chest roentgenography is unnecessary in the work-up of stage I and II breast cancer. J Clin Oncol 18(20):3503–3506
Ciatto S, Pacini P, Azzini V, Neri A, Jannini A, Gosso P et al (1988) Preoperative staging of primary breast cancer. A multicentric study. Cancer 61(5):1038–1040
Puglisi F, Follador A, Minisini AM, Cardellino GG, Russo S, Andreetta C et al (2005) Baseline staging tests after a new diagnosis of breast cancer: further evidence of their limited indications. Ann Oncol 16(2):263–266
Kasem AR, Desai A, Daniell S, Sinha P (2006) Bone scan and liver ultrasound scan in the preoperative staging for primary breast cancer. Breast J 12(6):544–548
Poonacha TK, Go RS (2011) Level of scientific evidence underlying recommendations arising from the national comprehensive cancer network clinical practice guidelines. J Clin Oncol 29(2):186–191
Feig BW, Ching CD, Department OOS (2012) The MD anderson surgical oncology handbook. Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia
Houry S, Georgeac C, Hay JM, Fingerhut A, Boudet MJ (1995) A prospective multicenter evaluation of preoperative hemostatic screening tests. The french associations for surgical research. Am J Surg 170(1):19–23
Chee YL, Crawford JC, Watson HG, Greaves M (2008) Guidelines on the assessment of bleeding risk prior to surgery or invasive procedures. British committee for standards in haematology. Br J Haematol 140(5):496–504
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest Statement
All authors have no support, financial relationships, or interests from any institution or company for the submitted work presented in this manuscript.
Rights and permissions
About this article
Cite this article
Louie, R.J., Tonneson, J.E., Gowarty, M. et al. Complete blood counts, liver function tests, and chest x-rays as routine screening in early-stage breast cancer: value added or just cost?. Breast Cancer Res Treat 154, 99–103 (2015). https://doi.org/10.1007/s10549-015-3593-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3593-y