Abstract
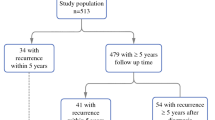
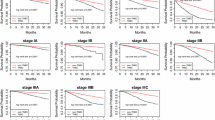
We evaluated whether the sequence or regimen of systemic chemotherapy could be a risk factor for breast cancer-related lymphedema (LE). We retrospectively analyzed 848 patients with stage II/III breast cancer who underwent curative surgery with adequate systemic therapy from 2004 to 2009. Adjuvant chemotherapy (ACT) was performed in 552 patients (65.1 %) and neoadjuvant chemotherapy (NAC) in 296 (34.9 %). We evaluated the incidence of LE based on clinicopathological factors and treatments. At a median follow-up of 5.1 years, 358 patients (42.2 %) had experienced LE and 243 (28.7 %) had retained (persistent LE) [120/552 (21.7 %) with ACT vs. 123/296 (41.6 %) with NAC; P < 0.001]. The incidence of LE in patients with taxane was greater than in those without taxane [233/704 (33.1 %) vs. 10/144 (6.9 %); P < 0.001]. Multivariate analysis showed that NAC [hazard ratio (HR), 1.63 in LE event; P < 0.001; HR, 1.39 in persistent LE; P = 0.02] and RT including supraclavicular area (SCRT) (HR 1.55; P = 0.02; HR 1.93; P = 0.006), number of dissected axillary lymph nodes (N-ALNs) >10 (HR, 1.37; P = 0.01; HR, 1.71; P = 0.001), advanced stage (HR, 1.31; P = 0.03; HR, 1.60; P = 0.002), and taxane (HR, 1.69; P = 0.03; HR, 2.07; P = 0.04) were independent risk factors for the LE occurrence. In addition to advanced stage, N-ALNs and SCRT, NAC, and taxane were shown to increase the risk of LE, which could help clinicians identify patients at risk for LE.

Similar content being viewed by others
References
Hack TF, Cohen L, Katz J (1999) Physical and psychological morbidity after axillary lymph node dissection for breast cancer. J Clin Oncol 17(1):143–149
Kwan W, Jackson J, Weir LM (2002) Chronic arm morbidity after curative breast cancer treatment: prevalence and impact on quality of life. J Clin Oncol 20(20):4242–4248
Gartner R, Jensen MB, Kronborg L (2010) Self-reported arm-lymphedema and functional impairment after breast cancer treatment–a nationwide study of prevalence and associated factors. Breast 2010 19(6):506–515
Petrek JA, Senie RT, Peters M, Rosen pp (2001) Lymphedema in a cohort of breast carcinoma survivors 20 years after diagnosis. Cancer 92(6):1368–1377
Meeske KA, Sullivan-Halley J, Smith AW et al (2009) Risk factors for arm lymphedema following breast cancer diagnosis in Black women and White women. Breast Cancer Res Treat 113(2):383–391
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515
Kim M, Kim SW, Lee SU et al (2013) A model to estimate the risk of breast cancer-related lymphedema: combinations of treatment-related factors of the number of dissected axillary nodes, adjuvant chemotherapy, and radiation therapy. Int J Radiat Oncol Biol Phys 86(3):498–503
Specht MC, Miller CL, Skolny MN et al (2013) Residual lymph node disease after neoadjuvant chemotherapy predicts an increased risk of lymphedema in node-positive breast cancer patients. Ann Surg Oncol 20(9):2835–2841
Boughey JC, Hoskin TL, Cheville AL et al (2014) Risk factors associated with breast lymphedema. Ann Surg Oncol 21(4):1202–1208
Kilbreath SL, Lee MJ, Refshauge KM et al (2013) Transient swelling versus lymphoedema in the first year following surgery for breast cancer. Support Care Cancer 21(8):2207–2215
Norman SA, Localio AR, Kallan MJ et al (2010) Risk factors for lymphedema after breast cancer treatment. Cancer Epidemiol Biomarkers Prev 19(11):2734–2746
Paskett ED, Naughton MJ, McCoy TP et al (2007) The epidemiology of arm and hand swelling in premenopausal breast cancer survivors. Cancer Epidemiol Biomarkers Prev 16(4):775–782
Shih YC, Xu Y, Cormier JN et al (2009) Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: a 2-year follow-up study. J Clin Oncol 27(12):2007–2014
Miller CL, Specht MC, Skolny MN et al (2014) Risk of lymphedema after mastectomy: potential benefit of applying ACOSOG Z0011 protocol to mastectomy patients. Breast Cancer Res Treat 144(1):71–77
Warren LE, Miller CL, Horick N et al (2014) The impact of radiation therapy on the risk of lymphedema after treatment for breast cancer: a prospective cohort study. Int J Radiat Oncol Biol Phys 88(3):565–571
Qin YY, Li H, Guo XJ et al (2011) Adjuvant chemotherapy, with or without taxanes, in early or operable breast cancer: a meta-analysis of 19 randomized trials with 30698 patients. PLoS ONE 6(11):e26946
Bronstad A, Berg A, Reed RK (2004) Effects of the taxanes paclitaxel and docetaxel on edema formation and interstitial fluid pressure. Am J Physiol Heart Circ Physiol 287(2):H963–H968
Jones SE, Savin MA, Holmes FA et al (2006) Phase III trial comparing doxorubicin plus cyclophosphamide with docetaxel plus cyclophosphamide as adjuvant therapy for operable breast cancer. J Clin Oncol 24(34):5381–5387
Andersson M, Lidbrink E, Bjerre K et al (2011) Phase III randomized study comparing docetaxel plus trastuzumab with vinorelbine plus trastuzumab as first-line therapy of metastatic or locally advanced human epidermal growth factor receptor 2-positive breast cancer: the HERNATA study. J Clin Oncol 29(3):264–271
Dominick SA, Madlensky L, Natarajan L, Pierce JP (2013) Risk factors associated with breast cancer-related lymphedema in the WHEL Study. J Cancer Surviv 7(1):115–123
Ahmed RL, Schmitz KH, Prizment AE, Folsom AR (2011) Risk factors for lymphedema in breast cancer survivors, the Iowa Women’s Health Study. Breast Cancer Res Treat 130(3):981–991
Sackey H, Magnuson A, Sandelin K et al (2014) Arm lymphoedema after axillary surgery in women with invasive breast cancer. Br J Surg 101(4):390–397
Purushotham AD, Bennett Britton TM, Klevesath MB et al (2007) Lymph node status and breast cancer-related lymphedema. Ann Surg 246(1):42–45
Coen JJ, Taghian AG, Kachnic LA et al (2003) Risk of lymphedema after regional nodal irradiation with breast conservation therapy. Int J Radiat Oncol Biol Phys 55(5):1209–1215
Acknowledgments
This research was supported by National Cancer Center Grant NCC-1210181-1 of the National Cancer Center, Republic of Korea. The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/eRGMeP.
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10549_2014_3137_MOESM1_ESM.tif
Supplementary material 1 Fig. 1 ROC curves for the number of dissected axillary lymph nodes (N-ALNs) and breast cancer-related lymphedema (LE) for a LE events and b persistent LE. (TIFF 77 kb)
Rights and permissions
About this article
Cite this article
Jung, SY., Shin, K.H., Kim, M. et al. Treatment factors affecting breast cancer-related lymphedema after systemic chemotherapy and radiotherapy in stage II/III breast cancer patients. Breast Cancer Res Treat 148, 91–98 (2014). https://doi.org/10.1007/s10549-014-3137-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-3137-x