Abstract
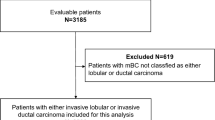
Invasive lobular carcinomas (ILC) show better clinical behaviour compared with other histological types, but significantly lower pathological complete response (pCR) rates after neoadjuvant chemotherapy (NACT). We investigated whether factors influencing pCR rate in ILC after NACT can be identified and whether clinical outcome is different. 9,020 breast cancer patients from nine German neoadjuvant trials with known histological type were pooled. 11.7 % of tumours were ILC. Endpoints were: pCR rate, surgery type and survival. ILC was associated with older age, larger tumour size, lymph node negativity, lower grade and positive hormone-receptor-status (HR). Patients with ILC achieved a significantly lower pCR rate compared with non-ILC patients (6.2 vs. 17.4 %, P < 0.001). The pCR rate was 4.2 % in ILC/HR+/G1-2, 7.0 % in ILC with either HR− or G3, and 17.8 % in ILC/HR−/G3. Mastectomy rate was higher in ILC compared with non-ILC patients irrespective of response to NACT (pCR: 27.4 vs. 16.6 %, P = 0.037 and non-pCR: 41.8 % vs. 31.5 %, P < 0.0001). Age and HR independently predicted pCR in ILC. In ILC patients, pCR did not predict distant disease free (DDFS) and loco-regional disease free survival (LRFS), but overall survival (OS). Non-pCR patients with ILC had significantly better DDFS (P = 0.018), LRFS (P < 0.0001) and OS (P = 0.044) compared with non-ILC patients. Patients with ILC had a low chance of obtaining a pCR and this is not well correlated with further outcome. The mastectomy rate was considerably high in ILC patients even after obtaining a pCR. We, therefore, suggest to offer NACT mainly to ILC patients with HR-negative tumours.


Similar content being viewed by others
References
Li CI, Anderson BO, Daling JR et al (2003) Trends in incidence rates of invasive lobular and ductal breast carcinoma. JAMA 289(11):1421–1424
Arpino G, Bardou VJ, Clark GM et al (2004) Infiltrating lobular carcinoma of the breast: tumour characteristics and clinical outcome. Breast Cancer Res 6(3):R149–R156
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19(5):403–410
Li CI, Uribe DJ, Daling JR (2005) Clinical characteristics of different histologic types of breast cancer. Br J Cancer 93(9):1046–1052
Rakha EA, Ellis IO (2010) Lobular breast carcinoma and its variants. Semin Diagn Pathol 27(1):49–61
Orvieto E, Maiorano E, Bottiglieri L et al (2008) Clinicopathologic characteristics of invasive lobular carcinoma of the breast: results of an analysis of 530 cases from a single institution. Cancer 113(7):1511–1520
Reis-Filho JS, Simpson PT, Jones C et al (2005) Pleomorphic lobular carcinoma of the breast: role of comprehensive molecular pathology in characterization of an entity. J Pathol 207(1):1–13
Lips EH, Mulder L, de Ronde JJ et al (2012) Neoadjuvant chemotherapy in ER+ HER2-breast cancer: response prediction based on immunohistochemical and molecular characteristics. Breast Cancer Res Treat 131(3):827–836
von Minckwitz G, Untch M, Blohmer J-U et al (2012) Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol 30(15):1796–1804
Cristofanilli M, Gonzalez-Angulo A, Sneige N et al (2005) Invasive lobular carcinoma classic type: response to primary chemotherapy and survival outcomes. J Clin Oncol 23(1):41–48
von Minckwitz G, Costa SD, Raab G et al (2001) Dose-dense doxorubicin, docetaxel, and granulocyte colony-stimulating factor support with or without tamoxifen as preoperative therapy in patients with operable carcinoma of the breast: a randomized, controlled, open phase IIb study. J Clin Oncol 19(15):3506–3515
Untch M, Loibl S, Bischoff J et al (2012) Lapatinib versus trastuzumab in combination with neoadjuvant anthracycline-taxane-based chemotherapy (GeparQuinto, GBG 44): a randomised phase 3 trial. Lancet Oncol 13(2):135–144
Wolff AC, Hammond ME, Schwartz JN et al (2007) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol 25(1):118–145
Untch M, Fasching PA, Konecny GE et al (2011) Pathologic complete response after neoadjuvant chemotherapy plus trastuzumab predicts favorable survival in human epidermal growth factor receptor 2-overexpressing breast cancer: results from the TECHNO trial of the AGO and GBG study groups. J Clin Oncol 29(25):3351–3357
von Minckwitz G, Rezai M, Loibl S et al (2010) Capecitabine in addition to anthracycline/taxane-based neoadjuvant treatment in patients with primary breast cancer: the phase III GeparQuattro study. J Clin Oncol 28(12):2015–2023
von Minckwitz G, Eidtmann H, Rezai M et al (2012) Neoadjuvant chemotherapy and bevacizumab for HER2-negative breast cancer. N Engl J Med 366(4):299–309
von Minckwitz G, Raab G, Caputo A et al (2005) Doxorubicin with cyclophosphamide followed by docetaxel every 21 days compared with doxorubicin and docetaxel every 14 days as preoperative treatment in operable breast cancer: the GEPARDUO study of the German Breast Group. J Clin Oncol 23(12):2676–2685
Thomssen C, Scharl A, Harbeck N (2011) AGO recommendations for diagnosis and treatment of patients with primary and metastatic breast cancer. Update 2011. Breast Care (Basel) 6(4):299–313
Purushotham A, Pinder S, Cariati M et al (2010) Neoadjuvant chemotherapy: not the best option in estrogen receptor-positive, HER2-negative, invasive classical lobular carcinoma of the breast? J Clin Oncol 28(22):3552–3554
Katz A, Saad ED, Porter P et al (2007) Primary systemic chemotherapy of invasive lobular carcinoma of the breast. Lancet Oncol 8(1):55–62
Goldhirsch A, Winer EP, Coates AS et al (2013) Personalizing the treatment of women with early breast cancer: highlight of the St. Gallen International expert consensus on the primary therapy of early breast cancer. Ann Oncol 24(9):2206–2223
Boughey JC, Wagner J, Garrett BJ et al (2009) Neoadjuvant chemotherapy in invasive lobular carcinoma may not improve rates of breast conservation. Annals Surg Oncol 16(6):1606–1611
Delpech Y, Coutant C, Hsu L et al (2013) Clinical benefit from neoadjuvant chemotherapy in oestrogen receptor-positive invasive ductal and lobular carcinomas. Br J Cancer 108(2):285–291
Morrow M, Kiney K, Scholtens D et al (2006) Selecting patients for breast conserving surgery – The Importance of Lobular Histology. Cancer 106(12):2563–2568
Voogd AC, Nielsen M, Peterse JL et al (2001) Differences in risk factors for local and distant recurrence after breast-conserving therapy or mastectomy for stage I and II breast cancer: pooled results of two large European randomized trials. J Clin Oncol 19(6):1688–1697
Diepenmaat LA, van der Sangen M, van de Poll-Franse LV et al (2009) The impact of postmastectomy radiotherapy on local control in patients with invasive lobular breast cancer. Radiother Oncol 91(1):49–53
Biglia N, Maggiorotto F, Liberale V et al (2013) Clinical-pathologic features, long term-outcome and surgical treatment in a large series of patients with invasive lobular carcinoma (ILC) and invasive ductal carcinoma (IDC). Eur J Surg Oncol 39(5):455–460
Vo T, Meric-Bernstam F, Yi Min et al (2006) Outcomes of breast-conservation therapy for invasive lobular carcinoma are equivalent to those for invasive ductal carcinoma. Am J Surg 192(4):552–555
Colleoni M, Rotmensz N, Maisonneuve P et al (2012) Outcome of special types of luminal breast cancer. Ann Oncol 23(6):1428–1436
Cortazar P, Zhang L, Untch M et al (2012) Meta-analysis results from the collaborative trials in neoadjuvant breast cancer (CTNeoBC). Cancer Res 72(24 Suppl.):S1–S11
Noske A, Loibl S, Darb-Esfahani S et al (2011) Comparison of different approaches for assessment of HER2 expression on protein and mRNA level: prediction of chemotherapy response in the neoadjuvant GeparTrio trial (NCT00544765). Breast Cancer Res Treat 126(1):109–117
Denkert C, Huober J, Loibl S et al (2013) HER2 and ESR1 mRNA expression levels and response to neoadjuvant trastuzumab plus chemotherapy in patients with primary breast cancer. Breast Cancer Res 15:R11
Metzger-Filho O, Procter M, de Azambuja E et al (2013) Magnitude of trastuzumab benefit in patients with HER2-positive, invasive lobular breast carcinoma: results from the HERA trial. J Clin Oncol 31(16):1954–1960
Longacre TA, Ennis M, Quenneville LA et al (2006) Interobserver agreement and reproducibility in classification of invasive breast carcinoma: an NCI breast cancer family registry study. Mod Pathol 19(2):195–207
Kiaer H, Andersen JA, Rank F et al (1988) Quality control of patho-anatomical diagnosis of carcinoma of the breast. Acta Oncol 27(6A):745–747
Rakha EA, El-Sayed ME, Menon S et al (2008) Histologic grading is an independent prognostic factor in invasive lobular carcinoma of the breast. Breast Cancer Res Treat 111(1):121–127
Metzger-Filho O, Michiels S, Bertucci F et al (2013) Genomic grade adds prognostic value in invasive lobular carcinoma. Ann Oncol 24(2):377–384
Rakha EA, El-Sayed ME, Powe DG et al (2008) Invasive lobular carcinoma of the breast: response to hormonal therapy and outcomes. Eur J Cancer 44:73–83
Conflict of interest
The authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sibylle Loibl and Cristina Volz, shared first authorship.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Loibl, S., Volz, C., Mau, C. et al. Response and prognosis after neoadjuvant chemotherapy in 1,051 patients with infiltrating lobular breast carcinoma. Breast Cancer Res Treat 144, 153–162 (2014). https://doi.org/10.1007/s10549-014-2861-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-2861-6