Abstract
Clinical trials have shown the efficacy of trastuzumab-based adjuvant therapy in HER2-positive breast cancers, but routine clinical use awaits evaluation of compliance, safety, and effectiveness. Adjuvant trastuzumab-based therapy in routine clinical use was evaluated in the retrospective study GHEA, recording 1,002 patients treated according to the HERA protocol between March 2005 and December 2009 in 42 Italian oncology departments; 874 (87.23 %) patients completed 1-year trastuzumab treatment. In 128 patients (12.77 %), trastuzumab was withdrawn due to cardiac or non-cardiac toxicity (28 and 29 patients, respectively), disease progression (5 patients) or the clinician’s decision (66 patients). In addition, 156 patients experienced minor non-cardiac toxicities; 10 and 44 patients showed CHF and decreased LVEF, respectively, at the end of treatment. Compliance and safety of adjuvant trastuzumab-based therapy in Italian hospitals were high and close to those reported in the HERA trial. With a median follow-up of 32 months, 107 breast cancer relapses were recorded (overall frequency, 10.67 %), and lymph node involvement, estrogen receptor negativity, lymphoid infiltration, and vascular invasion were identified as independent prognostic factors for tumor recurrence, indicating that relapses were associated with advanced tumor stage. Analysis of site and frequency of distant metastases showed that bone metastases were significantly more frequent during or immediately after trastuzumab (<18 months from the start of treatment) compared to recurrences in bone after the end of treatment and wash-out of the drug (>18 months from the start of treatment) (35.89 vs. 14.28 %, p = 0.0240); no significant differences were observed in recurrences in the other recorded body sites, raising the possibility that the protection exerted by trastuzumab is lower in bone metastases.
Similar content being viewed by others
Introduction
The HER2 gene is amplified and/or overexpressed in 15–25 % of breast cancers and is associated with an aggressive disease course [1–4]. Trastuzumab, a humanized monoclonal antibody targeting the extracellular domain of the transmembrane tyrosine kinase receptor HER2 [5], has been shown in phase III clinical trials to reduce the risk of relapse and death in patients with HER2-positive breast cancers when administered along with chemotherapy in an adjuvant setting [6–9]. Results of the Herceptin Adjuvant (HERA) trial at 2 years of median follow-up showed that 1-year adjuvant trastuzumab treatment significantly improved rates of disease-free survival (DFS) [hazard ratio (HR) = 0.63, 95 % CI 0.53–0.75; p < 0.0001) and overall survival (HR = 0.63, 95 % CI 0.45–0.87; p = 0.0051) [10] respect to observation group, with a significant benefit still observed at 4-year [11] and 8-year [12] median follow-up. These findings confirm that adjuvant trastuzumab given sequentially to chemotherapy is associated with a persistent benefit and remains an appropriate treatment modality in patients with HER2-positive early breast cancer. However, estimates provided by clinical trials for eligible patients may not be entirely applicable to all women receiving trastuzumab-based therapy in community practice, pointing to the need for observational studies as a tool to achieve a complete picture of compliance and safety of trastuzumab-based treatment.
The observational retrospective multicenter Italian study GHEA (Group HErceptin in Adjuvant Therapy) was designed to evaluate the adherence to trastuzumab treatment guidelines and the safety of adjuvant trastuzumab in Italian patients treated in routine clinical practice according to the HERA protocol. Indeed, the protocol of the HERA trial is a key reference for trastuzumab-containing chemotherapy regimens in treating HER2-positive breast cancer mainly carried out in an adjuvant setting in Europe, including Italy. As an additional parameter to estimate trastuzumab benefits in community practice, the GHEA study also sought to determine whether patients relapsing under trastuzumab treatment differ from those relapsing after the end of the treatment with respect to prognostic factors and site/frequency of distant metastases.
Patients and methods
Patients
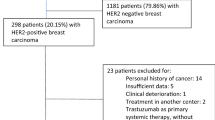
The multicenter retrospective observational Italian study GHEA included 1,002 HER2-positive breast cancer patients treated with trastuzumab in an adjuvant setting in 42 Italian oncology departments from March 2005 to December 2009. The database, closed on 16 December 2010, was examined in follow-up. Oncology departments were recruited through a public call for Italian oncologic centers treating at least 50 breast cancers/year and with HER2-positive patients treated with adjuvant trastuzumab from March 2005 to December 2009. Patients who were considered eligible for adjuvant trastuzumab by the oncologist and receiving this treatment for at least one cycle in the indicated period were included. All primary tumors were scored 3+ by immunohistochemistry or 2+/FISH-positive prior to trastuzumab treatment in each institution. As in the HERA trial, trastuzumab was administered, mainly every 3 weeks, in patients with primary breast cancer following surgery, chemotherapy (neoadjuvant and/or adjuvant), and radiotherapy (if applicable). Histopathological data, chemotherapy treatments, type of surgery, site of first relapse, and times of relapse were recorded for each patient. Non-cardiac toxicity data, including haematological, gastrointestinal, respiratory, renal, liver, dermatological, neurological, and infective adverse events, as well as trastuzumab-associated cardiotoxicity, including congestive heart failure (CHF), decrease in LVEF, and alteration of conduction or pace, were registered. Adverse events were assessed clinically and by haematological and biochemical means throughout the treatment in each participating center. Cardiac function was monitored in all patients every 4 months by electrocardiogram, and LVEF was assessed by echocardiography or multiple gate acquisition (MUGA) scan. LVEF decrease of ≥10 percentage points from baseline to <50 % at any time was considered as adverse event. Breast cancer first-relapse events were registered as local, contralateral, or distant when they occurred, respectively, in the same breast as the first tumor, in the other breast, or in another part of the body [central nervous system (CNS), bone, liver, lung, visceral, lymph nodes, and other organs]. For patients with multiple synchronous sites of recorded events, the first-relapse site was hierarchically considered as distant, local, contralateral breast cancer, and second primary malignancies. Non-breast second primary tumors were considered as “other neoplasia”. Relapses were subgrouped either as “early” when they occurred during the 1-year trastuzumab treatment and in the next 6 months or “late” when they occurred after the 18 months. DFS was defined as the time from start of trastuzumab treatment to the first event.
To ensure rapid and homogeneous data-gathering for patients enrolled in the study, a web-based system was specifically developed to record patient clinical and demographical data. Structured forms for data entry using the Microsoft SQL server and with exclusive log-in and password for Internet access to insert and update all data by each participating center were created. The database was accessible to a single administrator who supervised and monitored data accrual in each center since the beginning of the project. At the end of the data entry period, access to the system was restricted for all participating centers. The Independent Ethics Committee of each participant institution approved the observational study.
Statistical analysis
Bivariate analysis was carried out for all variables with respect to relapses, using contingency tables evaluated by Chi square or Fisher’s exact test. DFS analysis was carried out based on the life-table method [13] including any types of relapses.
Univariate analysis was carried out using the phreg SAS procedure with univariate Cox proportional hazards regression. All predictors with p < 0.05 were used in multivariate analysis with backward elimination, using the Cox regression model and evaluated by Chi square test. Assumption of proportionality was tested for all covariates by including time-dependent covariates in the model using the interaction with log(time). All analyses were conducted using SAS software (SAS Institute Inc., Cary, NC). Two-sided p < 0.05 was considered significant.
Results
We analyzed data from 1,002 HER2-positive breast cancer patients treated with trastuzumab in an adjuvant setting. Table 1 lists the characteristics of patients and disease. The median age was 52.9 years, 45.01 % of patients were node-negative, 44.01 % were both ER− and PgR-positive, and 17.16 % were positive for one of the two hormone receptors, and 53.69 % had T1 tumor size (54.85 % of T1 tumors were node-negative). As expected for HER2-positive carcinomas, tumors were mainly grade III (59.99 %) and of ductal histotype (85.43 %). All patients were treated with chemotherapy: 182 received neoadjuvant treatment, 862 received adjuvant treatment, and 42 both. Chemotherapy was mostly anthracycline-based (84.33 %) and 45.41 % of these patients also received taxanes. Hormone therapy was used in 54.99 % of patients, 60.44 %of whom received aromatase inhibitors. Almost all recorded patients (97.80 %) underwent trastuzumab administration every 3 weeks, with 1-year trastuzumab treatment completed in 874 (87.23 %) patients. Of 128 patients (12.77 %) who discontinued trastuzumab, 123 stopped for reasons other than relapse and 5 for relapse during therapy. Treatment withdrawal was due to cardiac and non-cardiac adverse events in 28 (20 for CHF and 8 for decreased LVEF), and 29 patients (10 for dermatological, 6 for haematological, 4 for gastrointestinal, 4 for neurological, 2 for infective, 1 for renal, 1 for liver, and 1 for respiratory adverse events), respectively, and to clinical judgment in 66 (Table 2). Toxicity was the most relevant factor leading to trastuzumab withdrawal in patients treated for <6 months, while the clinical decision was the major motivation to stop treatment in those who received trastuzumab for ≥6 but <12 months (Table 2). Of note, 80.36 % of these patients had T1 and/or N0 tumors. In addition, 156 patients experienced minor non-cardiac toxicities; of 701 patients who were monitored for cardiac toxicities past the end of treatment, 10 and 44 patients showed CHF and decreased LVEF, respectively. In the entire series, LVEF was monitored by MUGA in only 20 patients. Non-cardiac toxicities included haematological, gastrointestinal, respiratory, renal, liver, dermatological, and neurological adverse events.
With a median follow-up of 32 months, 107 (10.68 %) breast cancer events, including local (1.80 %), contralateral (0.10 %), and distant recurrences (8.78 %), were registered (Table 3; Fig. 1). In addition, 9 (0.90 %) secondary non-breast primary tumors were observed (one thyroid, one lung, one renal, two endometrial, one leukemia, and three unspecified carcinomas). Figure 2 shows the DFS of our series calculated from the start of trastuzumab treatment. When breast cancer relapse occurring after the end of the treatment was analyzed according to time of trastuzumab treatment, five (13.51 %) recurrences were observed in 37 patients treated <6 months, 6 (6.59) in 91 patients treated from ≥6 to <12 months, and 74 (8.47) in 874 patients who completed the 1-year treatment.
Analysis of the clinical and pathological characteristics listed in Table 1 revealed an association between tumor recurrence and axillary lymph node involvement (N+) (p < 0.0001), larger tumor size (p < 0.0001), absence of estrogen receptors (p < 0.0001), and of progesterone receptors (p = 0.0018), vascular invasion (p = 0.0005), lymphoid infiltration (p = 0.0023), grade III (p = 0.0026), and chemotherapy regimens (p = 0.0024) (Table 4). Univariate analysis indicated that lymph node involvement, grade III, larger tumor size, lymphoid infiltration, vascular invasion, absence of hormone receptors, and treatment with anthracyclines plus taxanes were significantly associated (p < 0.05) with DFS (Table 5). A positive significant correlation of the anthracyclines plus taxanes regimen was observed with size and node positivity (p < 0.0001), indicating that patients with more advanced tumors received this therapeutic regimen. Multivariate analysis of covariates displaying p < 0.05 identified lymph node involvement (HR = 3.633, 95 % CI 1.600–8.249, p = 0.0020), presence of estrogen receptors (HR = 0.552, 95 % CI 0.314–0.968, p = 0.0382), lymphoid infiltration (HR = 1.912, 95 % CI 1.061–3.444, p = 0.0310), and vascular invasion (HR = 1.853, 95 % CI 1.028–3.338, p = 0.0400) as independent prognostic factors (Table 5).
Comparison of “early” recurrences (44 cases, including five local relapses) arising during or immediately after trastuzumab treatment (≤18 months from start of treatment) and “late” recurrences (63 relapses, including 13 local and 1 contralateral recurrences) occurring after the end of the treatment and wash-up of the drug (>18 months from start of treatment) revealed no significant differences in clinical and pathological parameters (Table 6).
In our series, bone (23.86 %) was the most frequent site of first distant metastasis, followed by CNS (17.05 %). Notably, comparison of the frequency of first distant metastases in the two subgroups (39 early vs. 49 late distant metastases) according to site (Table 7) indicated a significantly higher rate of bone metastases in early than in late recurrences (35.89 vs. 14.28 %, p = 0.0240) and a higher, although not statistically significant, incidence of CNS relapses (23.07 vs. 12.24 %). Metastases in the late versus early group were not significantly more frequent in liver (16.32 vs. 10.26 %), lung (18.37 vs. 10.26 %), other viscera (6.12 vs. 0.00 %), or lymph nodes (16.32 vs. 7.69 %); cases with multiple relapses at the time of diagnosis were equally distributed in the two subgroups (14.28 % in early vs. 10.26 % in late metastases).
Discussion
The observational study GHEA shows that trastuzumab treatment is feasible and well-tolerated in routine clinical practice. Indeed, the majority of the patients recorded in the study adhered to trastuzumab administration following locoregional treatment and chemotherapy as in the HERA trial, with injection every 3 weeks in 97.80 % of them and completion of the 1-year trastuzumab therapy in 874 (87.23 %) patients. The treatment discontinuation rate was higher in our series than in the HERA trial [6, 10] due to 6.587 % of patients who stopped trastuzumab not for toxicity but for clinical and/or patient decision, while the frequency of adverse events accounting for trastuzumab withdrawal was similar to that in the HERA trial.
While toxicities were the major reason for treatment withdrawal within 6 months, later withdrawal reflected the clinician’s judgment that for patients at low risk of recurrence, the risk of adverse cardiac events could be minimized by reducing the treatment length without compromising efficacy. Indeed, less than 1-year of trastuzumab is reportedly active in decreasing relapse rates [8]. Consistent with this hypothesis, of the 56 patients who stopped the treatment based on the clinician’s decision, 80.36 % had T1 and/or N0 tumors. The low aggressiveness of these carcinomas is also demonstrated by the lower frequency of relapses after withdrawal compared with patients who stopped before 6 months of treatment. The decision against completing 1-year trastuzumab treatment is still rare and, in fact, was made for only about 7 % of the patients in Italian clinical practice.
Trastuzumab was withdrawn due to cardiac events in 28 patients (2.79 %), a rate similar to that in the HERA trial [14, 15]. However, another 54 patients experienced cardiac toxicity after the end of treatment, consistent with a recent population-based observational study [16] reporting that the risk of cardiotoxicity associated with trastuzumab following anthracycline appears to increase over time. This underscores the need for long-term surveillance of cardiotoxicity. Since trastuzumab followed anthracycline-based regimens in the majority of patients, clinical practice should include cardiac monitoring past the end of treatment.
We observed that patients treated with adjuvant trastuzumab in the Italian clinical practice were at an earlier stage of disease compared with those included in the HERA trial. Overall, the 11 % of relapse events observed in the GHEA study is similar to the 13 % reported in the 2-year median follow-up of HERA [10], considering the earlier stage of disease of our patients. Recently published results [17] derived from 87 patients treated with adjuvant trastuzumab in a public hospital showed a compliance and safety similar to that of our study and of the HERA trial, further supporting the feasibility of this treatment outside clinical trials.
Our analysis of the role of pathobiological markers in increasing the risk of relapse suggests that the recurrences in trastuzumab-treated patients in clinical practice are associated with a more advanced stage of disease, consistent with the progressively decreased dependence of more advanced tumors on the HER2 signaling pathway [18]. Since maximum trastuzumab activity in clinical trials is reportedly restricted to the time of treatment and a few months thereafter [10], we hypothesize that relapses in this period are “truly” resistant, while later relapses that might have been sensitive when trastuzumab was present develop upon antibody wash-out. Thus, assuming that early relapses recorded in our study are associated with trastuzumab resistance, we speculate that the pathobiologic parameters analyzed are not involved in trastuzumab resistance since their distribution was similar in early and late relapses. This is consistent with other reports showing Forest plots unable to identify parameters predictive of resistance and useful in clinical practice; indeed, no association between response to trastuzumab and hormone receptor status, grade, node involvement, or size has been found [10, 11].
Notwithstanding the observational nature of our study and the limited number of cases of relapses in our series, we noted a significantly higher frequency of bone relapses during the trastuzumab treatment as compared to recurrences at that site after the end of treatment and wash-out of the drug. While the higher frequency of CNS metastatic disease [19] is consistent with the inability of trastuzumab to pass the blood–brain barrier and affect brain metastases [20–22], the lower activity of trastuzumab in preventing bone relapses should be of interest for clinicians to better direct choice of therapies in these patients. Proof of the low activity of trastuzumab in countering bone metastases awaits analysis of bone relapses occurring during and after trastuzumab treatment with respect to the observational HERA patient population. If proven, the basis of this low efficacy of trastuzumab on bone metastases warrants analyses to estimate the drug’s penetration in this tissue, although antibodies can localize in bone [23], or to confirm in vivo the reduction of HER2 expression levels in tumor cells homing to the bone, as reported in some studies ([24] and references therein). These mechanisms might impair both cytotoxic and cytostatic effects of trastuzumab (reviewed in [4]), triggering resistance escape mechanisms through upregulation of other receptor activities or through perturbation of the bone microenvironment [25–27].
Our data pointing to low trastuzumab activity in bone relapses are consistent with its higher activity on visceral recurrences observed in the HERA trial with 1-year median follow-up [6], i.e., during or immediately after trastuzumab administration, and also at 4-year median follow-up, when the best trastuzumab-induced benefits were observed for liver recurrences [28].
Among other trials of trastuzumab in the adjuvant setting, only PACS06 reported relapses according to site in the randomized arms [29]; however, the lack of a statistically significant reduction in relapse risk by trastuzumab observed in that study precludes comparison with our results. Moreover, final overall survival analysis of the EGF104900 trial, a phase III randomized multicenter open-label study of lapatinib alone compared with lapatinib plus trastuzumab in patients with HER2-positive metastatic breast cancer, whose disease progressed during prior trastuzumab therapy, showed that patients with visceral but not those with bone disease significantly benefited from the addition of trastuzumab to lapatinib treatment [30].
In conclusion, our data revealed high compliance of adjuvant trastuzumab treatment in Italian oncology clinics, a satisfactory trastuzumab safety profile, and a treatment efficacy close to that observed in clinical trials. Our results indicating a significantly higher frequency of bone metastases in the first 18 months from the start of trastuzumab treatment merit-specific future analyses to address the possibility that trastuzumab has low efficacy in bone metastases.
References
Slamon DJ, Clark GM, Wong SG et al (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235:177–182
Slamon DJ, Godolphin W, Jones LA et al (1989) Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 244:707–712
Reese DM, Slamon DJ (1997) HER-2/neu signal transduction in human breast and ovarian cancer. Stem Cells 15:1–8
Tagliabue E, Campiglio M, Pupa SM et al (2012) Activity and resistance mechanisms of trastuzumab in different clinical settings. Cancer Treat Rev 38:212–217
Carter P, Presta L, Gorman CM et al (1992) Humanization of an anti-p185 HER2 antibody for human cancer therapy. Proc Natl Acad Sci USA 89:4285–4289
Piccart-Gebhart MJ, Procter M, Leyland-Jones B et al (2005) Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med 353:1659–1672
Romond EH, Perez EA, Bryant J et al (2005) Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353:1673–1684
Joensuu H, Bono P, Kataja V et al (2009) Fluorouracil, epirubicin, and cyclophosphamide with either docetaxel or vinorelbine, with or without trastuzumab, as adjuvant treatments of breast cancer: final results of the FinHer Trial. J Clin Oncol 27:5685–5692
Slamon D, Eiermann W, Robert N et al (2011) Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med 365:1273–1283
Smith I, Procter M, Gelber RD et al (2007) 2-Year follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer: a randomised controlled trial. Lancet 369:29–36
Gianni L, Dafni U, Gelber RD et al (2011) Treatment with trastuzumab for 1 year after adjuvant chemotherapy in patients with HER2-positive early breast cancer: a 4-year follow-up of a randomised controlled trial. Lancet Oncol 12:236–244
Goldhirsch A, Piccart-Gebhart MJ, Procter (2013) HERA TRIAL: 2 years versus 1 year of trastuzumab after adjuvant chemotherapy in women with HER2-positive early breast cancer at 8 years of median follow up. Cancer Res 72 [24 suppl], 103 s (S5-2)
Cox DR (1972) Regression models and life tables. J R Stat Soc 34:187–220
Suter TM, Procter M, van Veldhuisen DJ et al (2007) Trastuzumab-associated cardiac adverse effects in the herceptin adjuvant trial. J Clin Oncol 25:3859–3865
Procter M, Suter TM, De AE et al (2010) Longer-term assessment of trastuzumab-related cardiac adverse events in the Herceptin Adjuvant (HERA) trial. J Clin Oncol 28:3422–3428
Bowles EJ, Wellman R, Feigelson HS et al (2012) Risk of heart failure in breast cancer patients after anthracycline and trastuzumab treatment: a retrospective cohort study. J Natl Cancer Inst 104:1293–1305
Palmieri C, Shah D, Krell J et al (2011) Management and outcome of HER2-positive early breast cancer treated with or without trastuzumab in the adjuvant trastuzumab era. Clin Breast Cancer 11:93–102
Sharma SV, Settleman J (2007) Oncogene addiction: setting the stage for molecularly targeted cancer therapy. Genes Dev 21:3214–3231
Kennecke H, Yerushalmi R, Woods R et al (2010) Metastatic behavior of breast cancer subtypes. J Clin Oncol 28:3271–3277
Hasan A, Ghebeh H, Lehe C et al (2011) Therapeutic targeting of B7-H1 in breast cancer. Expert Opin Ther Targets 15:1211–1225
Geyer CE, Martin A, Newstat B, et al. (2007) Lapatinib (L) plus capecitabine (C) in HER2+ advanced breast cancer (ABC): Genomic and updated efficacy data. J Clin Oncol. Suppl 25, 40s-Abstract 1035
Azim HA, Azim HA Jr (2012) Systemic treatment of brain metastases in HER2-positive breast cancer: current status and future directions. Future Oncol 8:135–144
Dijkers EC, Oude Munnink TH, Kosterink JG et al (2010) Biodistribution of 89Zr-trastuzumab and PET imaging of HER2-positive lesions in patients with metastatic breast cancer. Clin Pharmacol Ther 87:586–592
Niikura N, Liu J, Hayashi N et al (2012) Loss of human epidermal growth factor receptor 2 (HER2) expression in metastatic sites of HER2-overexpressing primary breast tumors. J Clin Oncol 30:593–599
Johnston SR, Head J, Pancholi S et al (2003) Integration of signal transduction inhibitors with endocrine therapy: an approach to overcoming hormone resistance in breast cancer. Clin Cancer Res 9:524S–532S
Rosales C, Brown EJ (1991) Two mechanisms for IgG Fc-receptor-mediated phagocytosis by human neutrophils. J Immunol 146:3937–3944
Jones DH, Nakashima T, Sanchez OH et al (2006) Regulation of cancer cell migration and bone metastasis by RANKL. Nature 440:692–696
Metzger-Filho O, Procter M, De Azambuja AE et al (2013) Magnitude of trastuzumab benefit in patients with HER2-positive, invasive lobular breast carcinoma: results from the HERA trial. J Clin Oncol 31:1954–1960
Spielmann M, Roche H, Delozier T et al (2009) Trastuzumab for patients with axillary-node-positive breast cancer: results of the FNCLCC-PACS 04 trial. J Clin Oncol 27(36):6129–6134
Blackwell KL, Burstein HJ, Storniolo AM et al (2012) Overall survival benefit with lapatinib in combination with trastuzumab for patients with human epidermal growth factor receptor 2-positive metastatic breast cancer: final results from the EGF104900 Study. J Clin Oncol 30(21):2585–2592
Acknowledgments
We thank Luca Gianni for helpful discussion and critical review of the manuscript. We also thank Laura Mameli for secretarial assistance. This work was supported by Associazione Italiana per la Ricerca sul Cancro (AIRC) (SM) and Roche s.p.a. The sponsor has no role in study design, collection analysis, interpretation of the data, in the writing of the manuscript, or in the decision to submit the manuscript.
Conflict of interest
GM has received fees as an invited speaker to oncology meetings from Roche, Celgene, Elsai, Novartis, Glaxo, Agendia and Alphagenetics. All remaining authors have declared no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was conducted on behalf of the GHEA group. The members of the GHEA group are listed in Appendix.
Appendix
Appendix
S. Ménard (Molecular Targeting Unit, Department of Experimental Oncology and Molecular Medicine, Fondazione IRCCS Istituto Nazionale dei Tumori, Milano, Italy); G.R.R. Ricciardi (University Policlinic G. Martino, Palermo, Italy); M. Mottolese (Regina Elena National Cancer Institute, Rome, Italy); E. Taibi (Humanitas Centro Catanese di Oncologia, Catania, Italy); G. Carrillo (Azienda Ospedaliera di Rilievo Nazionale A. Cardarelli, Naples, Italy); A. Piga (Ospedale Oncologico Businco, Cagliari, Italy); D. Quitadamo (Centro Oncologico Aviano, Aviano, Italy); L. Memeo (Istituto Oncologico del Mediterraneo, Viagrande, Catania, Italy); S. Siena (Dipartimento Oncologico dell’Ospedalie Niguarda Ca’ Granda, Milano, Italy); R. Gnoni (IRCCS-Arcispedale Santa Maria Nuova, Reggio Emilia, Italy); A. Molino (Azienda Ospedaliera Universitaria Integrata di Verona, Verona, Italy); A. Jirillo (IRCCS Istituto Oncologico Veneto, Padua, Italy); G. Cavazzini (Azienda Ospedaliera Carlo Poma, Mantua); A. Lugini (Ospedale San Camillo de Lellis, Rieti, Italy); V. Sanna (Ospedale Civile SS. Annunziata, Sassari, Italy); M. Fantini (Ospedale degli Infermi Azianda USL, Rimini, Italy); D. Errante (Ospedale Civile di Vittorio Veneto ULSS7 del Veneto, Vittorio Veneto, Italy ); M. Di Seri (Policlinico Umberto I, Rome, Italy); O. Gottardi (IRCCS Multimedica, Sesto San Giovanni, Italy); A. Gambaro (Azienda Ospedaliera L. Sacco- Polo Universitario, Milano, Italy); A. Di Leo (Ospedale Misericordia e Dolce, Prato, Italy); M.P. Muttini (Ospedale Civico, Carrara, Italy); M. D’Aprile (Ospedale Santa Maria Goretti, Latina, Italy); R. Ghisini (Istituto Europeo di Oncologia, Milano, Italy); M. Mauri (Az Ospedaliera San Giovanni, Rome, Italy); M. Visini (Ospedale Manzoni, Lecco, Italy); E. Baldini (Presidio Ospedaliero Campo di Marte, Lucca, Italy); A. Rizzi (Fondazione Poliambulanza Istituto Ospedaliero, Brescia, Italy); C. Savastano (Az. Ospedaliera S. Giovanni di Dio e Ruggi d’Aragona, San Giovanni, Italy); A. Bertolini (Ospedale di Sondrio, Sondrio, Italy); M. Frisinghelli (Presidio Ospedaliera S. Chiara, Pisa, Italy); L. Amaducci (Ospedale di Faenza, Faenza, Italy); R. Visentin (Fondazione IRCCS Cà Granda Osp. Maggiore Policlinico, Milano, Italy); N. La Verde (Azienda Ospedaliera Fatebenefratelli Oftalmico, Milano, Italy); L. Pavesi (Fondazione Maugeri, Pavia, Italy); A. Pisano (Ospedale Santa Maria delle Grazie, Pozzuoli, Italy); S. Ortu (Ospedale Giovanni Paolo II, Olbia, Italy); G. Masci (Istituto Clinico Humanitas, Milano, Italy); M. Airoldi (Azienda Ospedaliera Città della Salute e della Scienza, Turin); C.A. Tondini (Ospedali Riuniti, Bergamo, Italy); F. Bassan (Ospedale Boldrini, Thiene, Italy)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Campiglio, M., Bufalino, R., Sasso, M. et al. Effect of adjuvant trastuzumab treatment in conventional clinical setting: an observational retrospective multicenter Italian study. Breast Cancer Res Treat 141, 101–110 (2013). https://doi.org/10.1007/s10549-013-2658-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2658-z