Abstract
Estrogen synthesis suppression induced by aromatase inhibitors in breast cancer (BC) patients may be affected by single nucleotide polymorphisms (SNPs) of the gene encoding aromatase enzyme, CYP19A1. We assessed the association between plasma estrone sulfate (ES), letrozole treatment, and four SNPs of CYP19A1 gene (rs10046 C>T, rs4646 G>T, rs749292 C>T, rs727479 T>G) which seem to be related to circulating estrogen levels. Patients were enrolled into a prospective, Italian multi-center clinical trial (Gruppo Italiano Mammella, GIM-5) testing the association of CYP19A1 SNPs with the efficacy of letrozole adjuvant therapy, in postmenopausal early BC patients. SNPs were identified from peripheral blood cell DNA. Plasma ES concentrations were evaluated by Radio Immuno Assay. Blood samples were obtained immediately before letrozole therapy (N = 204), at 6-weeks (N = 178), 6 (N = 152) and 12-months (N = 136) during treatment. Medians (IQR) of ES were 160 pg/mL (85–274) at baseline, 35 pg/mL (12–64) at 6-weeks, 29 pg/mL (17–48) at 6 months and 25 pg/mL (8–46) after 12 months treatment. No statistically significant association was evident between polymorphisms and ES circulating levels during letrozole therapy. Letrozole suppression of the aromatase enzyme function is not affected by polymorphisms of CYP19A1 gene in postmenopausal BC patients.
Similar content being viewed by others
Introduction
The third-generation aromatase inhibitor letrozole is a highly potent and totally selective suppressor of aromatase activity [1] approved by the Food and Drug Administration (FDA) since 1997 for treating postmenopausal breast cancer (BC) patients. Peripheral aromatization of androgens is the main source of endogenous estrogens in postmenopausal women.
By effectively blocking estrogen synthesis, letrozole inhibits the growth or induces the regression of hormone-responsive breast tumors in vivo [2].
CYP19A1 gene encodes for aromatase (cytochrome P-450, family 19, subfamily A, polypeptide1; 15q21.1), the enzyme responsible for the final step of estrogen biosynthesis, i.e., the conversion of steroidal C-19 androgens (androstenedione and testosterone) to C-18 estrogens (estrone and estradiol). Several reports have shown that CYP19A1 genetic polymorphisms are significantly associated with different levels of circulating estrogens. Dunning et al. [3] found that in postmenopausal women, the rs10046 single nucleotide polymorphism (SNP) was predictive of different levels of estradiol, estrone, and estradiol:testosterone ratio although this polymorphism accounted only for 1.6 % of the total variance.
Analysis of 103 common CYP19A1 SNPs, carried out in five large prospective cohorts of postmenopausal women, showed that specific haplotypes, such as those composed of the two SNPs rs727479 and rs749292, were significantly associated with higher circulating levels of estradiol and estrone [4].
CYP19A1 genetic variants have also been related with tumor stage, HER2 status and efficacy of aromatase inhibitors [5–8]; recently, it has been suggested that specific CYP19A1 polymorphisms might be clinical markers predictive of the efficacy of letrozole treatment in metastatic BC patients [9]. In fact, it has been reported that in postmenopausal metastatic BC women treated with letrozole, time to progression (TTP) was significantly prolonged in those with the rare T allele of rs4646 compared with homozygotes for the wild-type variant (G/G) [5]. On the other hand, the same variants (G/T and T/T) were associated with a poorer benefit from letrozole (shorter progression-free survival), evaluated in a neoadjuvant setting [6].
In the present study, we evaluated four common CYP19A1 polymorphisms and plasma level concentrations of estrone sulfate, immediately before and up to 12 months from the beginning of aromatase inhibitor treatment, in a cohort of Italian postmenopausal BC patients. Primary aim of this study was to verify potential association between genetic polymorphisms of CYP19A1 and the letrozole activity evaluated by measuring estrone sulfate circulating levels as an index of aromatase enzyme function.
Patients and methods
Study design and patients
This study is a part of a multicenter, prospective, not comparative study of adjuvant hormonal therapy with letrozole after 4, 5 years to 6 years of tamoxifen (GIM5—Gruppo Italiano Mammella GIM-5 trial—EudraCT n. 2005-001213-18; EU clinical trial register; https://www.clinicaltrialsregister.eu/ctr-search/trial/2005-001213-18/IT) in postmenopausal early BC patients, which aims at evaluating the correlation between SNPs of CYP19A1 and Disease-Free Survival (DFS). For the purpose of the ancillary study reported herein, genetic analysis of CYP19A1 gene from peripheral blood cells was performed together with dosage of plasma estrone sulfate in a subgroup of patients to assess the associations between SNPs of CYP19 and aromatase inhibition calculated in terms of plasma estrone sulfate concentrations.
Patients
Postmenopausal women with early hormone receptor positive (ER+ and/or PgR+ ≥1 % by immunohistochemical evaluation) BC were eligible. Main inclusion criteria were (1) stage I–II–III histologically confirmed BC; (2) radical surgery (either mastectomy or breast conserving surgery) and axillary or sentinel node dissection or biopsy; (3) previous adjuvant hormonal therapy with Tamoxifen for at least 4, 5 years and no more than 6 years and a risk of recurrence ≥10 % (i.e., node positive (pN+) BC or node negative (pN−) BC and one of the following: pT1c and G3, or pT2 and G ≥ 2, or pT3 and any G). Tamoxifen had to be stopped no more than 6 months before study entry; and (4) postmenopausal status defined as (i) age >55 years with cessation of menses or (ii) age <55 years, but not spontaneous menses for ≥1 year, or (iii) age <55 years and spontaneous menses within the past 1 year, but currently amenorrheic (e.g., spontaneous or secondary to hysterectomy) and with postmenopausal gonadotropin levels (LH and FSH levels >40 IU/L) or postmenopausal estradiol levels (<5 ng/dL) or according to the definition of “postmenopausal range” for the laboratory involved. Patients had to have ECOG Performance Status ≤2 and adequate bone marrow, liver, and renal function.
The study was approved by the institutional review boards of the participating centers and all patients provided written informed consent.
Letrozole (Femara®, Novartis AG; Switzerland) was administered at the dose of 2.5 mg/day and the planned duration of the treatment was 5 years.
CYP19A1 genotyping
Genomic DNA was extracted from peripheral blood samples using QIAamp DNA blood Midi Kit (Qiagen S.p.A.) according to manufacturer’s instructions. Four common CYP19A1 variants were analyzed: rs749292 (c.1-23624C>T, ref seq AY957953.1), rs727479 (c.145 + 418G>T), and two polymorphisms located in the 3′ untranslated region (3′UTR), rs10046 (c* + 19C>T), and rs4646 (c* + 161G>T). Analysis of these latter snps was performed using the hexaprimer amplification refractory mutation system PCR (H-ARMS-PCR), as previously described [10].
Snps rs749292 and rs727479 were genotyped by two newly developed ARMS-PCRs. Briefly, PCR reactions were performed in a final volume of 20 μl containing ≈100 ng genomic DNA, 100 μmol/L dNTPs, specific buffer (1.5 mM MgCl2), and the appropriate concentration of each primer (Table 1). 1.25 U of AmpliTaq-Gold (Applera Europe.B.V.) plus 2.5 % DMSO (v/v) or 1.25 U HotStarTaq DNA Polymerase (QIAGEN S.p.A) plus 0.25× Q solution (v/v) were used for the amplification of rs749292 and rs727479, respectively. Detailed methods are reported in Table 1. PCR products were separated by electrophoresis on 2.5 % low melting point agarose gel containing ethidium bromide (Fig. 1).
Genotyping of CYP19A1 polymorphisms. a, b Tetra-ARMS-PCR for analysis of rs749292 and rs727479 snps. Representative results for C/C (lane 1), C/T (lane 2), and T/T (lane 3) patients are shown. The 476-bp amplicon identifies the PCR non-allele-specific control; the 308- and 219-bp fragments are associated to the C and the T alleles, respectively. M Molecular size marker (50 bp ladder). b Representative results for a G/G homozygote (lane 1), a G/T heterozygote (lane 2) and T/T homozygote (lane 3) are shown. The 572-bp fragment identifies the PCR control, the 385-bp and 236-bp fragments are associated to the G and the T alleles, respectively. M Molecular size marker (100 bp ladder). c Hexaprimer Amplification Refractory Mutation System PCR (H-ARMS) for simultaneous genotyping of rs10046 and rs4646 snps. Representative results for 6 patients. Lane 1 C/C homozygote (rs10046) and G/T heterozygote (rs4646), lane 2 C/C homozygote (rs10046) and T/T homozygote (rs4646), lane 3 C/T heterozygote (rs10046) and G/G homozygote (rs4646), lane 4 C/C homozygote (rs10046) and G/G homozygote (rs4646), lane 5 T/T homozygote (rs10046) and G/G homozygote (rs4646); lane 6 C/T heterozygote (rs10046) and G/T heterozygote (rs4646). The 255 bp and the 149 bp fragments correspond to the C and the T alleles of rs10046, respectively; the 289 bp and the 112 bp fragments correspond to the T allele (*) and the G allele (*) of rs4646, respectively. The C (rs10046)–T* (rs4646) haplotype is identified by a 202 bp specific fragment; the 342 bp amplicon represents the control PCR fragment
To confirm genotype results 25 % of sample DNAs, randomly selected, were blindly analyzed in an external laboratory ARMS and H-ARMS PCR analysis (with a different thermal cycler; moreover, in both the laboratories, 5 % of DNAs were further tested by direct sequencing on both DNA strands). No discrepancy was observed.
Hormone measurements
Blood samples for estrone sulfate assessment were collected from patients enrolled in seven Italian medical oncology departments. Medical oncologists of each center were adequately instructed about sample collection and storage. Samples were periodically sent to the centralized lab into dry ice-containing boxes and transported in temperature-controlled conditions.
Blood samples for hormone measurements were collected in vials containing sodium ethylenediaminetetraacetic acid (EDTA) between 8 and 10 a.m. to avoid circadian variations. Blood samples were collected before the beginning of letrozole treatment (baseline samples) and after 6 weeks (i.e., at the time of L steady state [11]), 6 months, and 1 year. Plasma samples were separated by centrifugation and stored at −80 °C until analyzed.
Estrone sulfate levels were determined by radioimmunoassay (RIA) after a non chromatographic procedure to eliminate interference from dehydroepiandrosterone sulfate (DHEAS) [12]. Briefly, plasma samples (200 μL for baseline and 600 μL for on-treatment samples) were extracted with 3 mL of absolute ethanol (Carlo Erba, Italy) in 5 mL polypropylene tubes. After 20 min of vigorous shaking, tubes were centrifuged (3500×g for 15 min at 4 °C) to pellet the denatured proteins. The supernatant was decanted in 5-mL flat bottom polypropylene vials, dried under nitrogen at room temperature (25 °C), reconstituted in 0.5 mL of 0.02 % sodium acetate buffer, pH 4.6, and transferred into 0.5 mL safe-lock tubes (Eppendorf, Germany). Capped tubes were heated for 18 h at 100 °C in a Thermoblock heating module and then they were centrifuged (16000 g for 15 min at 4 °C). To remove unconjugated steroids, the supernatant was collected and transferred in screw-capped 5-mL polypropylene vials containing 40 μL of di kalium hydrogen phosphate buffer 1 M pH 8.0 and extracted twice with 3 mL of diethyl ether (Carlo Erba, Italy). The ether extracts were decanted once the aqueous phase was frozen in dry-ice and discarded. The aqueous residuals were then dried under nitrogen at room temperature and reconstituted in 200 μL of pure water. An aliquot of 100 μL was used to evaluate estrone sulfate concentration using a commercially available estrone-sulfate radioimmunoassay kit (DSL-5400 Diagnostic Systems Laboratories Inc, Webster, TX) according to the assay procedure reported by manufacturer. Standard curves were set with seven estrone sulfate concentration points ranging from 0 to 2500 pg/mL; external control standards were prepared following the procedure above reported. Recovery, evaluated by comparing estrone sulfate standard concentrations before and after the cleaning procedure, was higher than 93 %. Coefficient of variation (CV %), evaluated by 6 replicates of the same sample, was below 14 %. Assay sensibility was 5 pg/mL and was calculated by the instrument (γ-scintillation counter Cobra II Autogamma, Canberra Packard) from standard curve.
Analyses of estrone sulfate plasma levels, as well as CYP19A1 genotyping, were performed at the centralized laboratories of the National Cancer Institute of Genoa.
Statistical methods
Plasma estrogen levels were found fit a log normal (ln) distribution [13]. Therefore, ln values for plasma estrone sulfate were used in all statistical analyses. Median, interquartile range (IQR), geometric mean (GM), and 95 % confidence intervals (CI) were used as summary measures for descriptive statistics.
ANOVA Univariate and ANCOVA (adjusted for baseline hormone levels) was used to assess the statistical significance of difference between means. A value of P < .05 was considered statistically significant.
SPSS software was employed for statistical analysis.
Deviation from Hardy–Weinberg equilibrium (HWE) was analyzed by Pearson X 2 test by means of the Finetti program (http://ihg2.helmholtz-muenchen.de/cgi-bin/hw/hwa2.pl [14]).
Haplotypes and the deviation between observed and expected frequencies were evaluated by Χ 2 of 3 × 3 table (http://www.oege.org/software/cubex/ [15]).
Results
Concentration of estrone sulfate in BC postmenopausal women before and after letrozole administration
Patients were enrolled in the clinical study between August 2005 and April 2008. Baseline plasma concentrations of estrone sulfate were evaluated on 204 patients. Patients’ characteristics are reported in Table 2. Median age was 62 years (range 40–80 years); median body mass index (BMI) was 25.8 kg/m2 (range 17.7–44.3 kg/m2).
At baseline, the geometric mean of circulating estrone sulfate was 138 pg/mL (95 % CI 117–162).
Medians and IQR of estrone sulfate concentrations evaluated in 204 patients at baseline, 178 pts after 6 weeks, 151 pts after 6 months, and 135 pts after 12 months are reported in Fig. 2. As expected, letrozole administration led to a steep decrease in estrone sulfate circulating levels. In fact, medians (IQR) of circulating estrone sulfate were 160 pg/mL (85–274) at baseline, 35 pg/mL (12–64) at 6-weeks, 29 pg/mL (17–48) at 6-months, and 25 pg/mL (8–46) after 12-months treatment, indicating a high and long-term activity of the aromatase inhibitor.
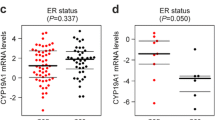
CYP19A1 polymorphisms, correlation with baseline concentrations of estrone sulfate and letrozole activity
Four CYP19A1 allelic variants were evaluated on enrolled BC patients: rs749292, located in exon1 (23624 bp from the ATG start codon), rs727479 in the IVS2 region, rs10046 and rs4646 in the 3′ untranslated region (3′UTR) of the aromatase-coding gene.
Allele and genotype frequencies observed in our patient cohort were superimposable to those reported for the European population and consistent with Hardy–Weinberg equilibrium (p > 0.05, data not shown).
Correlation between CYP19A1 polymorphisms and baseline estrone sulfate levels was performed. As shown in Table 3, the mean estrone sulfate concentration associated with the genotype C/C (rs749292), C/C (rs10046), G/G (rs727479), and T/T (rs4646) was lower than that observed for the other genotypes. The lowest levels were 101 and 99 pg/mL, observed in G/G (rs747279 and T/T (rs4646), respectively.
Differences in circulating estrone sulfate ranged from +35 % up to +44 % in patients with rs749292 C/T–T/T (vs C/C) and rs727479 T/G–T/T (vs G/G) variants, respectively; furthermore, estrone sulfate was ~23 and 52 % higher in T/T (rs10046) and G/G (rs4646) homozygote patients versus respective controls (C/C and T/T).
Although these results suggested that some of these genetic variants might be predictors of estrone sulfate concentrations, the differences observed did not reach statistical significance.
Out of the 204 patients, estrone sulfate plasma levels were evaluated in 178 patients after 6 weeks of letrozole treatment, in 151 patients after 6 months and in 135 patients after 12 months. Main causes of the decreased number of patients were lack of plasma sample collection during the followup visit, and treatment withdrawal for any reason. As shown in Table 3, no clear association was evident between polymorphisms and estrone sulfate circulating levels during letrozole therapy, being the hormone concentrations similar among each group. Statistical analyses, by ANOVA univariate and ANCOVA with adjustment for baseline concentration of estrone sulfate, did not show any significant difference.
Discussion
In women with hormone receptor positive BCs adjuvant endocrine treatment significantly reduces the risk of relapse and death [16, 17].
Estrogens are biosynthesized from androgens by the enzyme complex called aromatase. In postmenopausal women, intratumoral aromatase is the source of local estrogen production in BC tissues. Therefore, inhibition of aromatase is an important approach for reducing growth-stimulatory effects of estrogens in estrogen-dependent BC [18].
Letrozole is a third generation, non steroidal, well-tolerated, and effective aromatase inhibitor both in metastatic and early BC patients [19]. In postmenopausal women, adjuvant therapy with letrozole is more effective than tamoxifen, and extended adjuvant therapy with letrozole, after the completion of adjuvant tamoxifen therapy, is more effective than placebo in this patient population [20]. Although data are limited, circulating estrogen levels seem to influence disease-free survival in postmenopausal women with BC. Lønning et al. [21] reported a negative correlation between specific estrogens (estradiol and estrone sulfate) and the length of the disease free survival in postmenopausal women with breast cancer. In a case–control cohort study, Rock et al. [22] evaluated whether serum concentrations of estradiol, testosterone, and sex hormone binding protein were associated with recurrence free survival in women who were followed for more than 7 years after BC diagnosis. In their analysis, total estradiol, bioavailable estradiol, and free estradiol circulating concentrations were significantly associated with risk of recurrence. Therefore, higher circulating estrogen concentrations might accelerate the growth of micrometastasis in postmenopausal women treated in adjuvant setting for BC.
Primary aim of our study was to assess whether the letrozole activity in terms of aromatase inhibition, evaluated by plasma concentration of estrone sulfate, could be affected by the polymorphisms of the gene coding the enzyme.
The use of plasma estrogens (estradiol and estrone) to evaluate the activity of aromatase inhibitors is hampered by technical difficulties in measuring very low postmenopausal estrogen levels [23]. This is a negligible problem with estrone sulfate, being its levels reliably measurable by highly sensitive assay methods also in postmenopausal women. Plasma estrone sulfate is produced by sulfatation of circulating estrone and the levels of estradiol, estrone, and estrone sulfate are in equilibrium [24]. Thus, the inhibition of the peripheral aromatase causes a similar fall in all three plasma estrogens, and circulating estrone sulfate levels can be considered a surrogate marker for aromatase inhibitor activity [25]. Estrone sulfate was therefore chosen as indicator of estrogen suppression in this study.
We analyzed the association between the CYP19A1 genetic variants and the levels of estrone sulfate before and during treatment with letrozole. Despite the lack of a statistically significant difference, our results show a trend toward higher levels of baseline estrone sulfate associated with specific SNPs according to the results reported in healthy postmenopausal women, where the T/T genotype of rs10046 was significantly associated with higher levels of estrogens compared with the wild-type variant [3] and with the results of Haiman et al. [4] who reported also an effect per copy in BC patients carrying the TT (rs749292–rs727479) haplotype.
The lack of a statistically significant difference may be due to small sample size of our study as compared with previous reports. Moreover, the difference in our results as compared to those of other investigators, may partly be explained by the different patients' population of our study which consisted in early breast cancer patients previously treated with tamoxifen.
Finally, genotype/haplotype frequencies detected in our study fit the HW equilibrium and are comparable to those reported for the European population; however, it is also possible that other polymorphic variants, in linkage disequilibrium with the SNPs tested, are relevant and/or that these SNPs have a different frequency in Italians than other Europeans, as also described for other mutations [26]. Thus, an ethnicity-specific effect, although not so likely inside Europe, might not be ruled out, being our cohort composed only of Italian patients.
In our cohort of patients, mean baseline plasma concentrations of estrone sulfate were 138 pg/mL with a large concentration range (n.d.–1422 pg/mL). These results are in agreement with those reported in literature [27, 28] and obtained according to methods employing RIA after chromatographic cleaning of the samples [29, 30]. Letrozole administration determined a marked suppression of estrogen circulating concentrations, up to 90 % of mean baseline value, and estrone sulfate levels were found below the assay sensitivity level in nearly 6 % of total samples analyzed.
A marked reduction in estrone sulfate circulating levels was observed after letrozole administration; besides this, the activity of this drug was independent from the CYP19A1 variants. These results can be of clinical interest if we consider reports of other groups suggesting specific CYP19A1 polymorphisms as potential predictive markers of letrozole activity [5, 6] in different clinical setting. Colomer et al. [5] reported that different levels of circulating hormones may be responsible for the different clinical outcome observed between metastatic BC patients carriers of the T allele (rs4646) and those with the wild-type variant (TTP 17.2 vs. 6.4 months, p = 0.02, respectively). In this regard, our results, even if not directly amenable to that patient’s cohort, do not support this hypothesis.
Noteworthy, two other, more recent, studies investigated rs4646 genotype in letrozole-treated metastatic BC patients. In both studies, there was no significant association between rs4646 and AI treatment outcome [9, 31]. Moreover, Ferraldeschi et al. genotyped 71 selected single nucleotide variants in 16 candidate genes involved in estrogen and aromatase inhibitors metabolism. Two SNPs (rs10455592 and rs4775936) were associated to the Time to Treatment Failure in univariate analysis, but no variants had independent significance in multivariate analysis. Therefore, this study does not indicate any of the specific CYP19A1 polymorphism evaluated, as predictive clinical marker for AI treatment [31].
In our study, the activity of letrozole, evaluated by circulating concentration of ES, does not seem to be influenced by genetic variants of the gene coding for aromatase. In fact, letrozole treatment led to similar concentrations of circulating estrogens independently from CYP19A1 genotypes associated with postmenopausal estrogen production. This is likely due to the profound suppression of total body aromatization that is obtained with letrozole administration. Therefore, different clinical outcomes observed in women with allelic mutations of aromatase gene [5, 6] do not seem to be related to estrogen suppression. Regarding letrozole efficacy, our data are not conclusive due to the specific group of women who received letrozole in this study. When data on association between CYP19A1 polymorphisms and AI treatment clinical outcome will be available, we will be able to give a more comprehensive answer if these polymorphisms are predictive of letrozole efficacy in the adjuvant setting for early breast cancer patients.
Finally, no potential clinically useful difference was observed between data obtained at 6 weeks of treatment and after longer periods, indicating that the activity of letrozole is maintained even after several months of treatment.
References
Bhatnagar AS, Häusler A, Schieweck K et al (1990) Highly selective inhibition of estrogen biosynthesis by CGS 20267, a new non-steroidal aromatase inhibitor. J Steroid Biochem Mol Biol 37:1021–1027
Lønning PE (2011) The potency and efficacy of aromatase inhibitors across the breast cancer continuum. Ann Oncol 22:503–514
Dunning AM, Dowsett M, Healey CS et al (2004) Polymorphisms associated with circulating sex hormone levels in postmenopausal women. J Natl Cancer Inst 96:936–945
Haiman CA, Dossus L, Setiawan VW et al (2007) Genetic variation at the CYP19A1 locus predicts circulating estrogen levels but not breast cancer risk in postmenopausal women. Cancer Res 67:1893–1897
Colomer R, Monzo M, Tusquets I et al (2008) A single-nucleotide polymorphism in the aromatase gene is associated with the efficacy of the aromatase inhibitor letrozole in advanced breast carcinoma. Clin Cancer Res 14:811–816
Garcia-Casado Z, Guerrero-Zotano A, Llombart-Cussac A, et al (2010) A polymorphism at the 3′-UTR region of the aromatase gene defines a subgroup of postmenopausal breast cancer patients with poor response to neoadjuvant letrozole. BMC Cancer 10:36. http://www.biomedcentral.com/1471-2407/10/36. doi:10.1186/1471-2407-10-36
Ma X, Qi X, Chen C et al (2010) Association between CYP19 polymorphisms and breast cancer risk: results from 10,592 cases and 11,720 controls. Breast Cancer Res Treat 122:495–501
Fasching PA, Loehberg CR, Strissel PL et al (2008) Single nucleotide polymorphisms of the aromatase gene (CYP19A1), HER2/neu status, and prognosis in breast cancer patients. Breast Cancer Res Treat 112:89–98
Park IH, Lee YS, Lee KS et al (2011) Single nucleotide polymorphisms of CYP19A1 predict clinical outcomes and adverse events associated with letrozole in patients with metastatic breast cancer. Cancer Chemother Pharmacol 68:1263–1271
Piccioli P, Serra M, Pedemonte S et al (2008) Hexaprimer amplification refractory mutation system PCR for simultaneous single-tube genotyping of 2 close polymorphisms. Clin Chem 54:227–229
Lønning P, Pfister C, Martoni A, Zamagni C (2003) Pharmacokinetics of third-generation aromatase inhibitors. Semin Oncol 30:23–32
Brind JL, Chervinsky K, Völgelman JH, Orentreich N (1990) Radioimmunoassay of estrone sulfate in the serum of normal men after a non-chromatographic procedure that eliminates interference from dehydroepiandrosterone sulphate. Steroids 55:32–35
Lønning PE, Helle SI, Johannessen DC et al (1995) Relation between sex hormones, sex hormone binding globulin, insulin like growth factor-1 and insulin like growth factor binding protein-1 in postmenopausal breast cancer patients. Clin Endocrinol 42:23–30
Rodriguez S, Gaunt TR, Day IN (2009) Hardy–Weinberg equilibrium testing of biological ascertainment for Mendelian randomization studies. Am J Epidemiol 169:505–514
Gaunt TR, Rodriguez S, Day IN (2007) Cubic exact solutions for the estimation of pairwise haplotype frequencies: implications for linkage disequilibrium analyses and a web tool ‘CubeX’. BMC Bioinformatics 8:428. http://www.biomedcentral.com/1471-2105/8/428. doi:10.1186/1471-2105-8-428
Early Breast Cancer Trialists’ Collaborative Group (1992) Systemic treatment of early breast cancer by hormonal, cytotoxic, or immune therapy: 133 randomised trials involving 31,000 recurrences and 24,000 deaths among 75,000 women. Lancet 339:71–85
Early Breast Cancer Trialists’ Collaborative Group (1998) Polychemotherapy for early breast cancer: an overview of the randomised trials. Lancet 352:930–942
Brueggemeier RW, Hackett JC, Diaz-Cruz ES (2005) Aromatase inhibitors in the treatment of breast cancer. Endocr Rev 26:331–345
Dellapasqua S, Colleoni M (2010) Letrozole. Expert Opin Drug Metab Toxicol 6:251–259
Keating GM (2009) Letrozole: a review of its use in the treatment of postmenopausal women with hormone-responsive early breast cancer. Drugs 69:1681–1705
Lønning PE, Helle SI, Johannessen DC et al (1996) Influence of plasma estrogen levels on the length of the disease-free interval in postmenopausal women with breast cancer. Breast Cancer Res Treat 39:335–341
Rock CL, Flatt SW, Laughlin GA et al (2008) Reproductive steroid hormones and recurrence-free survival in women with a history of breast cancer. Cancer Epidemiol Biomarkers Prev 17:614–620
Boeddinghaus IM, Dowsett M (2001) Comparative clinical pharmacology and pharmacokinetic interactions of aromatase inhibitors. J Steroid Biochem Mol Biol 79:85–91
Lønning PE, Johannessen DC, Thorsen T (1989) Alteration in the production rate and the metabolism of estrone and estrone sulphate in breast cancer patients treated with aminoglutethimide. Br J Cancer 60:107–111
Geisler J, Lønning PE (2005) Endocrine effects of aromatase inhibitors and inactivators in vivo: review of data and method limitations. J Steroid Biochem Mol Biol 95:75–81
Gismondi V, Meta M, Bonelli L et al (2004) Prevalence of the Y165C, G382D and 1395delGGA germline mutations of the MYH gene in Italian patients with adenomatous polyposis coli and colorectal adenomas. Int J Cancer 109:680–684
Eliassen AH, Missmer SA, Tworoger SS, Hankinson SE (2006) Endogenous steroid hormone concentrations and risk of breast cancer: does the association vary by a woman’s predicted breast cancer risk? J Clin Oncol 24:1823–1830
The endogenous hormones and breast cancer collaborative group (2002) Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst 94:606–616
Cauley JA, Lucas FL, Kuller LH et al (1999) Elevated serum estradiol and testosterone concentrations are associated with a high risk for breast cancer. Study of Osteoporotic Fractures Research Group. Ann Intern Med 130:270–277
Roberts KD, Rochefort JG, Bleau G, Chapdelaine A (1980) Plasma estrone sulfate levels in postmenopausal women. Steroids 35:179–187
Ferraldeschi R, Arnedos M, Hadfield KD et al (2012) Polymorphisms of CYP19A1 and response to aromatase inhibitors in metastatic breast cancer patients. Breast Cancer Res Treat 133:1191–1198
Acknowledgments
To Marco Venturini, an outstanding clinician, clinical researcher, and teacher who left all of us too early. We gratefully acknowledge the participants of the multicenter Italian clinical trial (GIM5). This work was partially supported by grants from Ministero della Salute (Italy), Compagnia di San Paolo (Torino, Italy), Oncotech consortium (Naples, Italy), Novartis Pharma SpA (unrestricted grant).
Conflict of interest
Lucia Del Mastro received honoraria for speaking activity from Novartis. All remaining authors declare no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Lunardi, G., Piccioli, P., Bruzzi, P. et al. Plasma estrone sulfate concentrations and genetic variation at the CYP19A1 locus in postmenopausal women with early breast cancer treated with letrozole. Breast Cancer Res Treat 137, 167–174 (2013). https://doi.org/10.1007/s10549-012-2306-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2306-z