Abstract
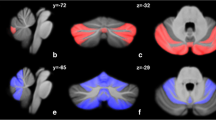
EPM1 (epilepsy, progressive myoclonic 1; Unverricht-Lundborg disease, OMIM #254800) is the most frequent form of progressive myoclonus epilepsy. Previous findings have suggested that its pathophysiology mainly involves the cerebellum, but the evaluation of cerebellar dysfunction is still unsatisfactory. The aim of this study was to assess the structural and functional involvement of the cerebellum in EPM1. We used voxel-based morphometry and spatially unbiased infra-tentorial template analyses of structural magnetic resonance imaging (MRI) scans, and functional MRI (fMRI) scans during block and event-related go/no-go motor tasks to study 13 EPM1 patients with mild to moderate myoclonus. We compared the results with those obtained in 12 age-matched healthy controls (HCs) and in 12 patients with hereditary spinocerebellar ataxia (SCA). Structural analyses revealed different patterns of atrophic changes in the EPM1 and SCA patients: in the former, they involved both cerebrum and cerebellum but, in the latter, only the cerebellum. During fMRI, block and event-related go/no-go tasks similarly activated the cerebellum and cerebrum in the EPM1 patients and HCs, whereas both tasks revealed much less cerebellar activation in the SCA patients than in the other two groups. Volumetric evaluation of the EPM1 patients showed that the cerebellum seemed to be marginally involved in a widespread atrophic process, and fMRI showed that it was not functionally impaired during motor tasks.




Similar content being viewed by others
References
Ashburner J (2007) A fast diffeomorphic image registration algorithm. Neuroimage 38:95–113
Bhatia KP, Brown P, Gregory R, Lennox GG, Manji H, Thompson PD, Ellison DW, Marsden CD (1995) Progressive myoclonic ataxia associated with coeliac disease. The myoclonus is of cortical origin, but the pathology is in the cerebellum. Brain 118:1087–1093
Buijink AW, Caan MW, Tijssen MA, Hoogduin JM, Maurits NM, van Rootselaar AF (2013) Decreased cerebellar fiber density in cortical myoclonic tremor but not in essential tremor. Cerebellum 12:199–204
Buijink AW, Broersma M, van der Stouwe AM, Sharifi S, Tijssen MA, Speelman JD, Maurits NM, van Rootselaar AF (2015) Cerebellar atrophy in cortical myoclonic tremor and not in hereditary essential tremor—a voxel-based morphometry study. Cerebellum, pp 1–9
Canafoglia L, Ciano C, Visani E, Anversa P, Panzica F, Viri M, Gennaro E, Zara F, Madia F, Franceschetti S (2010) Short and long interval cortical inhibition in patients with Unverricht-Lundborg and Lafora body disease. Epilepsy Res 89:232–237
Chew NK, Mir P, Edwards MJ, Cordivari C, Martino D, Schneider SA, Kim HT, Quinn NP, Bhatia KP (2008) The natural history of Unverricht-Lundborg disease: a report of eight genetically proven cases. Mov Disord 23:107–113
D’Agata F, Caroppo P, Boghi A, Coriasco M, Caglio M, Baudino B, Sacco K, Cauda F, Geda E, Bergui M, Geminiani G, Bradac GB, Orsi L, Mortara P (2011) Linking coordinative and executive dysfunctions to atrophy in spinocerebellar ataxia 2 patients. Brain Struct Funct 216:275–288
Diedrichsen J (2006) A spatially unbiased atlas template of the human cerebellum. Neuroimage 33:127–138
Diedrichsen J, Balsters JH, Flavell J, Cussans E, Ramnani N (2009) A probabilistic MR atlas of the human cerebellum. Neuroimage 46:39–46
Eldridge R, Iivanainen M, Stern R, Koerber T, Wilder BJ (1983) ‘‘Baltic’’ myoclonus epilepsy: hereditary disorder of childhood made worse by phenytoin. Lancet 2:838–842
Friston KJ, Holmes AP, Poline JB, Grasby PJ, Williams SC, Frackowiak RS, Turner R (1995) Analysis of fMRI time-series revisited. Neuroimage 2:45–53
Ganos C, Erro R, Edwards MJ, Rothwell J, Bhatia K (2014) The role of the cerebellum in the pathogenesis of cortical myoclonus. Mov Dis 29:438–443
Genton P (2010) Unverricht-Lundborg disease (EPM1). Epilepsia 51(suppl 1):37–39
Haltia M, Kristensson K, Sourander P (1969) Neuropathological studies in three Scandinavian cases of progressive myoclonus epilepsy. Acta Neurol Scand 45:63–77
Jayakumar PN, Desai S, Pal PK, Balivada S, Ellika S, Kalladka D (2008) Functional correlates of incoordination in patients with spinocerebellar ataxia 1: a preliminary fMRI study. J Clin Neurosci 15:269–277
Kälviäinen R, Khyuppenen J, Koskenkorva P, Eriksson K, Vanninen R, Mervaala E (2008) Clinical picture of EPM1-Unverricht-Lundborg disease. Epilepsia 49:549–556
Klockgether T, Wüllner U, Spauschus A, Evert B (2000) The molecular biology of the autosomal-dominant cerebellar ataxias. Mov dis 15:604–612
Korja M, Kaasinen V, Lamusuo S, Parkkola R, Nagren K, Marttila RJ (2007) Substantial thalamostriatal dopaminergic defect in Unverricht-Lundborg disease. Epilepsia 48:1768–1773
Koskenkorva P, Khyuppenen J, Niskanen E, Könönen M, Bendel P, Mervaala E, Lehesjoki AE, Kälviäinen R, Vanninen R (2009) Motor cortex and thalamic atrophy in Unverricht-Lundborg disease: voxelbased morphometric study. Neurology 73:606–611
Koskenkorva P, Niskanen E, Hyppönen J, Könönen M, Mervaala E, Soininen H, Kälviäinen R, Vanninen R (2012) Sensorimotor, visual, and auditory cortical atrophy in Unverricht-Lundborg disease mapped with cortical thickness analysis. AJNR Am J Neuroradiol 33:878–883
Koskiniemi M, Donner M, Majuri H, Haltia M, Norio R (1974) Progressive myoclonus epilepsy. A clinical and histopathological study. Acta Neurol Scand 50:307–332
Long L, Song Y, Zhang L, Hu C, Gong J, Xu L, Long H, Zhou L, Zhang Y, Zhang Y, Xiao B (2015) A case-control proton magnetic resonance spectroscopy study confirms cerebellar dysfunction in benign adult familial myoclonic epilepsy. Neuropsychiatr Dis Treat 11:485–491
Magaudda A, Ferlazzo E, Nguyen V-H, Genton P (2006) Unverricht-Lundborg disease, a condition with self-limited progression: long-term follow-up of 20 patients. Epilepsia 47(5):860–866
Magaudda A, Gelisse P, Genton P (2004) Antimyoclonic effect of levetiracetam in 13 patients with Unverricht-Lundborg disease: clinical observations. Epilepsia 45:678–681
Manninen O, Koskenkorva P, Lehtimäki KK, Hyppönen J, Könönen M, Laitinen T, Kalimo H, Kopra O, Kälviäinen R, Gröhn O, Lehesjoki AE, Vanninen R (2013) White matter degeneration with Unverricht-Lundborg progressive myoclonus epilepsy: a translational diffusion-tensor imaging study in patients and cystatin B-deficient mice. Radiology 269:232–239
Marsden CD, Harding AE, Obeso JA, Lu CS (1990) Progressive myoclonic ataxia (the Ramsay Hunt syndrome). Arch Neurol 47:1121–1125
Mascalchi M, Michelucci R, Cosottini M, Tessa C, Lolli F, Riguzzi P, Lehesjoki AE, Tosetti M, Villari N, Tassinari CA (2002) Brainstem involvement in Unverricht-Lundborg disease (EPM1): an MRI and 1H MRS study. Neurology 58:1686–1689
Muona M, Berkovic SF, Dibbens LM, Oliver KL, Maljevic S, Bayly MA, Joensuu T, Canafoglia L, Franceschetti S, Michelucci R, Markkinen S, Heron SE, Hildebrand MS, Andermann E, Andermann F, Gambardella A, Tinuper P, Licchetta L, Scheffer IE, Criscuolo C, Filla A, Ferlazzo E, Ahmad J, Ahmad A, Baykan B, Said E, Topcu M, Riguzzi P, King MD, Ozkara C, Andrade DM, Engelsen BA, Crespel A, Lindenau M, Lohmann E, Saletti V, Massano J, Privitera M, Espay AJ, Kauffmann B, Duchowny M, Møller RS, Straussberg R, Afawi Z, Ben-Zeev B, Samocha KE, Daly MJ, Petrou S, Lerche H, Palotie A, Lehesjoki AE (2015) A recurrent de novo mutation in KCNC1 causes progressive myoclonus epilepsy. Nat Genet 47:39–46
Panzica F, Canafoglia L, Franceschetti S (2014) EEG-EMG information flow in movement-activated myoclonus in patients with Unverricht-Lundborg disease. Clin Neurophysiol 125(9):1803–1808
Pennacchio LA, Bouley DM, Higgins KM, Scott MP, Noebels JL, Myers RM (1998) Progressive ataxia, myoclonic epilepsy and cerebellar apoptosis in cystatin B-deficient mice. Nat Genet 20:251–258
Santoshkumar B, Turnbull J, Minassian BA (2008) Unverricht-Lundborg progressive myoclonus epilepsy in Oman. Pediatr Neurol 38:252–255
Schmitz-Hübsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, Giunti P, Globas C, Infante J, Kang JS, Kremer B, Mariotti C, Melegh B, Pandolfo M, Rakowicz M, Ribai P, Rola R, Schöls L, Szymanski S, van de Warrenburg BP, Dürr A, Klockgether T, Fancellu R (2006) Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology 66:1717–1720. Erratum in: Neurology;67:299
Schulz JB, Borkert J, Wolf S, Schmitz-Hübsch T, Rakowicz M, Mariotti C, Schöls L, Timmann D, van de Warrenburg B, Dürr A, Pandolfo M, Kang M, Kang JS, Mandly AG, Nägele T, Grisoli M, Boguslawska R, Bauer P, Klockgether T, Hauser TK (2010) Visualization, quantification and correlation of brain atrophy with clinical symptoms in spinocerebellar ataxia types 1, 3 and 6. Neuroimage 49:158–168. Erratum in Neuroimage. 2010;50:1712
Silén T, Forss N, Salenius S, Karjalainen T, Hari R (2002) Oscillatory cortical drive to isometrically contracting muscle in Unverricht-Lundborg type progressive myoclonus epilepsy (ULD). Clin Neurophysiol 113:1973–1979
Stoodley CJ, Schmahmann JD (2009) Functional topography in the human cerebellum: a meta-analysis of neuroimaging studies. Neuroimage 44:489–501
Striano P, Caranci F, Di Benedetto R, Tortora F, Zara F, Striano S et al (2009) 1H-MR spectroscopy indicates prominent cerebellar dysfunction in benign adult familial myoclonic epilepsy. Epilepsia 50:1491–1497
Suoranta S, Holli-Helenius K, Koskenkorva P, Niskanen E, Könönen M, Äikiä M, Eskola H, Kälviäinen R, Vanninen R (2013) 3D texture analysis reveals imperceptible MRI textural alterations in the thalamus and putamen in progressive myoclonic epilepsy type 1, EPM1. PLoS ONE 8:e69905
Tijssen MA, Thom M, Ellison DW, Wilkins P, Barnes D, Thompson PD, Brown P (2000) Cortical myoclonus and cerebellar pathology. Neurology 54:1350–1356
Ugawa Y, Day BL, Rothwell JC, Thompson PD, Merton PA, Marsden CD (1991) Modulation of motor cortical excitability by electrical stimulation over the cerebellum in man. J Physiol 441:57–72
van Egmond ME, Verschuuren-Bemelmans CC, Nibbeling EA, Elting JW, Sival DA, Brouwer OF, de Vries JJ, Kremer HP, Sinke RJ, Tijssen MA, de Koning TJ (2014) Ramsay Hunt syndrome: clinical characterization of progressive myoclonus ataxia caused by GOSR2 mutation. Mov Disord 29:139–143
van Rootselaar AF, Aronica E, Jansen Steur EN, Rozemuller- Kwakkel JM, de Vos RA, Tijssen MA (2004) Familial cortical tremor with epilepsy and cerebellar pathological findings. Mov Disord 19:213–21726
van Rootselaar AF, van der Salm SM, Bour LJ, Edwards MJ, Brown P, Aronica E, Rozemuller-Kwakkel JM, Koehler PJ, Koelman JH, Rothwell JC, Tijssen MA (2007) Decreased cortical inhibition and yet cerebellar pathology in “familial cortical myoclonic tremor with epilepsy”. Mov Disord 22:2378–2385
Visani E, Agazzi P, Canafoglia L, Panzica F, Ciano C, Scaioli V, Avanzini G (2006) Franceschetti. movement-related desynchronization-synchronization (ERD/ERS) in patients with Unverricht-Lundborg disease. Neuroimage 33:161–168
Visani E, Minati L, Canafoglia L, Gilioli I, Salvatoni L, Varotto G, Fazio P, Aquino D, Bruzzone MG, Franceschetti S, Panzica F (2010) Simultaneous EEG-fMRI in patients with Unverricht-Lundborg disease: event-related desynchronization/synchronization and hemodynamic response analysis. Comput Intell Neurosci, p 164278
Visani E, Minati L, Canafoglia L, Gilioli I, Granvillano A, Varotto G, Aquino D, Fazio P, Bruzzone MG, Franceschetti S, Panzica F (2011) Abnormal ERD/ERS but unaffected BOLD response in patients with Unverricht-Lundborg disease during index extension: a simultaneous EEG-fMRI study. Brain Topogr 24:65–77
Acknowledgements
This study was partly supported by the Italian Ministry of Health, Grant RF-2011-02347420 (to CM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of C. Besta Neurological Institute Foundation and carried out in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All of the persons gave their informed consent before being included in the study. Any details that might reveal the identity of the study subjects have been omitted.
Additional information
Anna Nigri and Elisa Visani contributed equally to the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nigri, A., Visani, E., Bertolino, N. et al. Cerebellar Involvement in Patients with Mild to Moderate Myoclonus Due to EPM1: Structural and Functional MRI Findings in Comparison with Healthy Controls and Ataxic Patients. Brain Topogr 30, 380–389 (2017). https://doi.org/10.1007/s10548-016-0534-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10548-016-0534-y