Abstract
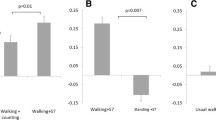
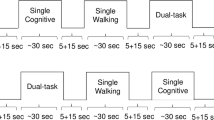
The posture first hypothesis suggests that under dual-task walking conditions older adults prioritize gait over cognitive task performance. Functional neural confirmation of this hypothesis, however, is lacking. Herein, we determined the functional neural correlates of the posture first hypothesis and hypothesized that the presence of neurological gait abnormalities (NGA) would moderate associations between brain activations, gait and cognitive performance. Using functional near-infrared spectroscopy we assessed changes in oxygenated hemoglobin levels in the pre-frontal cortex (PFC) during normal walk and walk while talk (WWT) conditions in a large cohort of non-demented older adults (n = 236; age = 75.5 ± 6.49 years; female = 51.7 %). NGA were defined as central (due to brain diseases) or peripheral (neuropathic gait) following a standardized neurological examination protocol. Double dissociations between brain activations and behavior emerged as a function of NGA. Higher oxygenation levels during WWT were related to better cognitive performance (estimate = 0.145; p < 0.001) but slower gait velocity (estimate = −6.336, p < 0.05) among normals. In contrast, higher oxygenation levels during WWT among individuals with peripheral NGA were associated with worse cognitive performance (estimate = −0.355; p < 0.001) but faster gait velocity (estimate = 14.855; p < 0.05). Increased activation in the PFC during locomotion may have a compensatory function that is designed to support gait among individuals with peripheral NGA.

Similar content being viewed by others
References
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders (text revision ed.). American Psychiatric Press, Washington, DC
Ayaz H, Izzetoglu M, Platek SM, Bunce S, Izzetoglu K, Pourrezaei K, Onaral B (2006) Registering fNIR data to brain surface image using MRI templates. Conf Proc IEEE Eng Med Biol Soc 1:2671–2674. doi:10.1109/IEMBS.2006.260835
Ayers EI, Tow AC, Holtzer R, Verghese J (2014) Walking while talking and falls in aging. Gerontology 60(2):108–113. doi:10.1159/000355119
Bloem BR, Grimbergen YA, van Dijk JG, Munneke M (2006) The “posture second” strategy: a review of wrong priorities in Parkinson’s disease. J Neurol Sci 248(1–2):196–204. doi:10.1016/j.jns.2006.05.010
Blumen HM, Holtzer R, Brown LL, Gazes Y, Verghese J (2014) Behavioral and neural correlates of imagined walking and walking-while-talking in the elderly. Hum Brain Mapp. doi:10.1002/hbm.22461
Cabeza R (2002). Hemispheric asymmetry reduction in older adults: the HAROLD model. Psychol Aging 17(1), 85–100. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11931290
Cooper RJ, Selb J, Gagnon L, Phillip D, Schytz HW, Iversen HK, Boas DA (2012) A systematic comparison of motion artifact correction techniques for functional near-infrared spectroscopy. Front Neurosci 6:147. doi:10.3389/fnins.2012.00147
Drew T, Prentice S, Schepens B (2004) Cortical and brainstem control of locomotion. Prog Brain Res 143:251–261. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=14653170
Duff K, Humphreys Clark JD, O’Bryant SE, Mold JW, Schiffer RB, Sutker PB (2008) Utility of the RBANS in detecting cognitive impairment associated with Alzheimer’s disease: sensitivity, specificity, and positive and negative predictive powers. Arch Clin Neuropsychol 23(5):603–612. doi:10.1016/j.acn.2008.06.004
England SE, Verghese J, Mahoney JR, Trantzas C, Holtzer R (2015) Three-level rating of turns while walking. Gait Posture 41(1):300–303. doi:10.1016/j.gaitpost.2014.09.010
Erdogan SB, Yucel MA, Akin A (2014) Analysis of task-evoked systemic interference in fNIRS measurements: insights from fMRI. Neuroimage 87:490–504. doi:10.1016/j.neuroimage.2013.10.024
Gerin-Lajoie M, Richards CL, McFadyen BJ (2005) The negotiation of stationary and moving obstructions during walking: anticipatory locomotor adaptations and preservation of personal space. Motor Control 9(3):242–269
Harada T, Miyai I, Suzuki M, Kubota K (2009) Gait capacity affects cortical activation patterns related to speed control in the elderly. Exp Brain Res 193(3):445–454. doi:10.1007/s00221-008-1643-y
Holtzer R, Verghese J, Xue X, Lipton RB (2006) Cognitive processes related to gait velocity: results from the Einstein Aging Study. Neuropsychology 20(2):215–223. doi:10.1037/0894-4105.20.2.215
Holtzer R, Verghese J, Wang C, Hall CB, Lipton RB (2008) Within-person across-neuropsychological test variability and incident dementia. JAMA 300(7):823–830. doi:10.1001/jama.300.7.823
Holtzer R, Mahoney JR, Izzetoglu M, Izzetoglu K, Onaral B, Verghese J (2011) fNIRS study of walking and walking while talking in young and old individuals. J Gerontol A Biol Sci Med Sci 66(8):879–887. doi:10.1093/gerona/glr068
Holtzer R, Wang C, Lipton R, Verghese J (2012a) The protective effects of executive functions and episodic memory on gait speed decline in aging defined in the context of cognitive reserve. J Am Geriatr Soc 60(11):2093–2098. doi:10.1111/j.1532-5415.2012.04193.x
Holtzer R, Wang C, Verghese J (2012b) The relationship between attention and gait in aging: facts and fallacies. Motor Control 16(1):64–80. http://www.ncbi.nlm.nih.gov/pubmed/22402221
Holtzer R, Epstein N, Mahoney JR, Izzetoglu M, Blumen HM (2014a) Neuroimaging of mobility in aging: a targeted review. J Gerontol A Biol Sci Med Sci 69(11):1375–1388. doi:10.1093/gerona/glu052
Holtzer R, Epstein N, Mahoney JR, Izzetoglu M, Blumen HM (2014b) Neuroimaging of mobility in aging: a targeted review. J Gerontol A Biol Sci Med Sci. doi:10.1093/gerona/glu052
Holtzer R, Mahoney J, Verghese J (2014c) Intraindividual variability in executive functions but not speed of processing or conflict resolution predicts performance differences in gait speed in older adults. J Gerontol A Biol Sci Med Sci 69(8):980–986. doi:10.1093/gerona/glt180
Holtzer R, Wang C, Verghese J (2014d) Performance variance on walking while talking tasks: theory, findings, and clinical implications. Age (Dordr) 36(1):373–381. doi:10.1007/s11357-013-9570-7
Holtzer R, Mahoney CJ, Wang C, England SE, Verghese J (2015) Online fronto-cortical control of simple and attention-demanding locomotion in humans. Neuroimage 112:152–159
Izzetoglu M, Bunce SC, Izzetoglu K, Onaral B, Pourrezaei K (2007) Functional brain imaging using near-infrared technology. IEEE Eng Med Biol Mag 26(4):38–46. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17672230
Izzetoglu M, Chitrapu P, Bunce S, Onaral B (2010) Motion artifact cancellation in NIR spectroscopy using discrete Kalman filtering. Biomed Eng Online 9:16. doi:10.1186/1475-925X-9-16
Jobsis FF (1977) Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science 198(4323):1264–1267. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=929199
Kirilina E, Jelzow A, Heine A, Niessing M, Wabnitz H, Bruhl R, Tachtsidis I (2012) The physiological origin of task-evoked systemic artefacts in functional near infrared spectroscopy. Neuroimage 61(1):70–81. doi:10.1016/j.neuroimage.2012.02.074
Li KZH, Lindenberger U, Freund AM, Baltes PB (2001) Walking while memorizing: age-related differences in compensatory behavior. Psychol Sci 12(3):230–237
Lindenberger U, Marsiske M, Baltes PB (2000) Memorizing while walking: increase in dual-task costs from young adulthood to old age. Psychol Aging 15(3):417–436
MacDonald AW 3rd, Cohen JD, Stenger VA, Carter CS (2000) Dissociating the role of the dorsolateral prefrontal and anterior cingulate cortex in cognitive control. Science 288(5472):1835–1838
Mirelman A, Maidan I, Bernad-Elazari H, Nieuwhof F, Reelick M, Giladi N, Hausdorff JM (2014) Increased frontal brain activation during walking while dual tasking: an fNIRS study in healthy young adults. J Neuroeng Rehabil 12(11):85. doi:10.1186/1743-0003-11-85
Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD (2000) The unity and diversity of executive functions and their contributions to complex “Frontal Lobe” tasks: a latent variable analysis. Cognit Psychol 41(1):49–100. doi:10.1006/cogp.1999.0734
Nutt JG, Marsden CD, Thompson PD (1993) Human walking and higher-level gait disorders, particularly in the elderly. Neurology 43(2):268–279. http://www.ncbi.nlm.nih.gov/pubmed/8437689
Oh-Park M, Xue X, Holtzer R, Verghese J (2011) Transient versus persistent fear of falling in community-dwelling older adults: incidence and risk factors. J Am Geriatr Soc 59(7):1225–1231. doi:10.1111/j.1532-5415.2011.03475.x
Reuter-Lorenz PA, Jonides J, Smith EE, Hartley A, Miller A, Marshuetz C, Koeppe RA (2000) Age differences in the frontal lateralization of verbal and spatial working memory revealed by PET. J Cogn Neurosci 12(1):174–187. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=10769314
Rosso AL, Studenski SA, Chen WG, Aizenstein HJ, Alexander NB, Bennett DA, Rosano C (2013) Aging, the central nervous system, and mobility. J Gerontol A Biol Sci Med Sci 68(11):1379–1386. doi:10.1093/gerona/glt089
Schaefer S, Schellenbach M, Lindenberger U, Woollacott M (2015) Walking in high-risk settings: do older adults still prioritize gait when distracted by a cognitive task? Exp Brain Res 233(1):79–88. doi:10.1007/s00221-014-4093-8
Schwenk M, Zieschang T, Oster P, Hauer K (2010) Dual-task performances can be improved in patients with dementia: a randomized controlled trial. Neurology 74(24):1961–1968. doi:10.1212/WNL.0b013e3181e39696
Stern Y (2009) Cognitive reserve. Neuropsychologia 47(10):2015–2028. doi:10.1016/j.neuropsychologia.2009.03.004
Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Guralnik J (2011) Gait speed and survival in older adults. JAMA 305(1):50–58. doi:10.1001/jama.2010.1923
Verghese J, Lipton RB, Hall CB, Kuslansky G, Katz MJ, Buschke H (2002) Abnormality of gait as a predictor of non-Alzheimer’s dementia. N Engl J Med 347(22):1761–1768. doi:10.1056/NEJMoa020441
Verghese J, LeValley A, Hall CB, Katz MJ, Ambrose AF, Lipton RB (2006) Epidemiology of gait disorders in community-residing older adults. J Am Geriatr Soc 54(2):255–261. doi:10.1111/j.1532-5415.2005.00580.x
Verghese J, Derby C, Katz MJ, Lipton RB (2007) High risk neurological gait syndrome and vascular dementia. J Neural Transm 114(10):1249–1252. doi:10.1007/s00702-007-0762-0
Verghese J, Robbins M, Holtzer R, Zimmerman M, Wang C, Xue X, Lipton RB (2008) Gait dysfunction in mild cognitive impairment syndromes. J Am Geriatr Soc 56(7):1244–1251. doi:10.1111/j.1532-5415.2008.01758.x
Verghese J, Ambrose AF, Lipton RB, Wang C (2010a) Neurological gait abnormalities and risk of falls in older adults. J Neurol 257(3):392–398. doi:10.1007/s00415-009-5332-y
Verghese J, Mahoney J, Ambrose AF, Wang C, Holtzer R (2010b) Effect of cognitive remediation on gait in sedentary seniors. J Gerontol A Biol Sci Med Sci 65(12):1338–1343. doi:10.1093/gerona/glq127
Verghese J, Holtzer R, Lipton RB, Wang C (2012) Mobility stress test approach to predicting frailty, disability, and mortality in high-functioning older adults. J Am Geriatr Soc 60(10):1901–1905. doi:10.1111/j.1532-5415.2012.04145.x
Yogev-Seligmann G, Hausdorff JM, Giladi N (2008) The role of executive function and attention in gait. Mov Disord 23(3):329–342. doi:10.1002/mds.21720
Yogev-Seligmann G, Giladi N, Brozgol M, Hausdorff JM (2012) A training program to improve gait while dual tasking in patients with Parkinson’s disease: a pilot study. Arch Phys Med Rehabil 93(1):176–181. doi:10.1016/j.apmr.2011.06.005
Yuan J, Blumen HM, Verghese J, Holtzer R (2014) Functional connectivity associated with gait velocity during walking and walking-while-talking in aging: a resting-state fMRI study. Hum Brain Mapp. doi:10.1002/hbm.22717
Acknowledgments
This research was supported by the National Institutes on Aging R01AG036921 (PI: R. Holtzer) and R01AG044007 (PI: J. Verghese).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Dr. Izzetoglu has a very minor share in the company that manufactures the fNIRS device used in this study. All other authors have no conflicts of interest to report in relation to the current article.
Rights and permissions
About this article
Cite this article
Holtzer, R., Verghese, J., Allali, G. et al. Neurological Gait Abnormalities Moderate the Functional Brain Signature of the Posture First Hypothesis. Brain Topogr 29, 334–343 (2016). https://doi.org/10.1007/s10548-015-0465-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10548-015-0465-z