Abstract
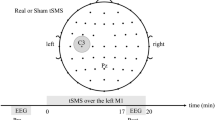
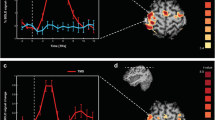
Multimodal human brain mapping has been proposed as an integrated approach capable of improving the recognition of the cortical correlates of specific neurological functions. We used simultaneous EEG-fMRI (functional magnetic resonance imaging) and EEG-TD-fNIRS (time domain functional near-infrared spectroscopy) recordings to compare different hemodynamic methods with changes in EEG in ten patients with progressive myoclonic epilepsy and 12 healthy controls. We evaluated O2Hb, HHb and Blood oxygen level-dependent (BOLD) changes and event-related desynchronization/synchronization (ERD/ERS) in the α and β bands of all of the subjects while they performed a simple motor task. The general linear model was used to obtain comparable fMRI and TD-fNIRS activation maps. We also analyzed cortical thickness in order to evaluate any structural changes. In the patients, the TD-NIRS and fMRI data significantly correlated and showed a significant lessening of the increase in O2Hb and the decrease in BOLD. The post-movement β rebound was minimal or absent in patients. Cortical thickness was moderately reduced in the motor area of the patients and correlated with the reduction in the hemodynamic signals. The fMRI and TD-NIRS results were consistent, significantly correlated and showed smaller hemodynamic changes in the patients. This finding may be partially attributable to mild cortical thickening. However, cortical hyperexcitability, which is known to generate myoclonic jerks and probably accounts for the lack of EEG β-ERS, did not reflect any increased energy requirement. We hypothesize that this is due to a loss of inhibitory neuronal components that typically fire at high frequencies.


Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- BOLD:
-
Blood oxygen level-dependent
- CT:
-
Cortical thickness
- EEG:
-
Electroencephalography
- EMG:
-
Electromyography
- EPM1:
-
Progressive myoclonic epilepsy 1A
- ERD/ERS:
-
Event-related desynchronization/synchronization
- fMRI:
-
Functional magnetic resonance imaging
- fNIRS:
-
Functional near-infrared spectroscopy
- FWE:
-
Family wise error
- FWHM:
-
Full width at half maximum
- GLM:
-
General linear model
- HHb:
-
Deoxyhemoglobin
- HRF:
-
Hemodynamic response function
- MDL:
-
Minimum description length
- MNI:
-
Montreal Neurological Institute
- MRI:
-
Magnetic resonance imaging
- NIR:
-
Near-infrared
- O2Hb:
-
Oxyhemoglobin
- ROI:
-
Region of interest
- SPM:
-
Statistical parametric mapping
- TD-fNIRS:
-
Time domain functional near-infrared spectroscopy
References
Allen PJ, Polizzi G, Krakow K, Fish DR, Lemieux L (1998) Identification of EEG events in the MR scanner: the problem of pulse artefact and a method for its subtraction. NeuroImage 8(3):229–239
Allen PJ, Josephs O, Turner R (2000) A method for removing imaging artefact from continuous EEG recorded during functional MRI. NeuroImage 12(2):230–239
Anwar AR, Muthalib M, Perrey S, Galka A, Granert O, Wolff S, Deuschl G, Raethjen J, Heute U, Muthuraman M (2013) Comparison of causality analysis on simultaneously measured fMRI and NIRS signals during motor tasks. Conf Proc IEEE Eng Med Biol Soc 2013:2628–2631
Attwell D, Laughlin SB (2001) An energy budget for signaling in the grey matter of the brain. J Cereb Blood Flow Metab 21(10):1133–1145
Buzzi A, Chikhladze M, Falcicchia C, Paradiso B, Lanza G, Soukupova M, Marti M, Morari M, Franceschetti S, Simonato M (2012) Loss of cortical GABA terminals in Unverricht–lundborg disease. Neurobiol Dis 47(2):216–224
Canafoglia L, Ciano C, Panzica F, Scaioli V, Zucca C, Agazzi P, Visani E, Avanzini G, Franceschetti S (2004) Sensorimotor cortex excitability in Unverricht–Lundborg disease and lafora body disease. Neurology 63:2309–2315
Canafoglia L, Ciano C, Visani E, Anversa P, Panzica F, Viri M, Gennaro E, Zara F, Madia F, Franceschetti S (2010) Short and long interval cortical inhibition in patients with Unverricht–Lundborg and lafora body disease. Epilepsy Res 89:232–237
Chen R, Tam A, Butefisch C, Corwell B, Ziemann U, Rothwell JC, Cohen LG (1998) Intracortical inhibition and facilitation in different representations of the human motor cortex. J Neurophysiol 80:2870–2881
Contini D, Torricelli A, Pifferi A, Spinelli L, Cubeddu R (2007) Novel method for depth-resolved brain functional imaging by time-domain NIRS. Proc SPIE 6629:662908
Contini D, Spinelli L, Caffini M, Cubeddu R, Torricelli A (2009) A multichannel time-domain brain oximeter for clinical studies. Proceedings of SPIE-OSA biomedical optics, P 7369 1D
Cui X, Bray S, Bryant DM, Glover GH, Reiss AL (2011) A quantitative comparison of NIRS and fMRI across multiple cognitive tasks. Neuroimage 54(4):2808–2821
Danner N, Julkunen P, Khyuppenen J, Hukkanen T, Kononen M, Saisanen L, Koskenkorva P, Vanninen R, Lehesjoki AE, Kalviainen R, Mervaala E (2009) Altered cortical inhibition in Unverricht–Lundborg type progressive myoclonus epilepsy (EPM 1). Epilepsy Res 85(1):81–88
Desikan RS, Segonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, Buckner RL, Dale AM, Maguire RP, Hyman BT, Albert MS, Killiany RJ (2006) An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage 31:968–980
Erbil N, Ungan P (2007) Changes in the alpha and beta amplitudes of the central EEG during the onset, continuation, and offset of long-duration repetitive hand movements. Brain Res 12(1169):44–56
Fischl B, van der Kouwe A, Destrieux C, Halgren E, Segonne F, Salat DH, Busa E, Seidman LJ, Goldstein J, Kennedy D, Caviness V, Makris N, Rosen B, Dale AM (2004) Automatically parcellating the human cerebral cortex. Cereb Cortex 14:11–22
Friston KJ, Holmes AP, Worsley KJ, Poline JB, Frith C, Frackowiak RSJ (1995) Statistical parametric maps in functional imaging: a general linear approach. Hum Brain Mapp 2:189–210
Gray MA, Minati L, Harrison NA, Gianaros PJ, Napadow V, Critchley HD (2009) Physiological recordings: basic concepts and implementation during functional magnetic resonance imaging. Neuroimage 47(3):1105–1115
Haeussinger FB, Heinzel S, Hahn T, Schecklmann M, Ehlis AC, Fallgatter AJ (2011) Simulation of near-infrared light absorption considering individual head and prefrontal cortex anatomy: implications for optical neuroimaging. PLoS ONE 6(10):e26377
Han X, Jovicich J, Salat D, van der Kouwe A, Quinn B, Czanner S, Busa E, Pacheco J, Albert M, Killiany R, Maguire P, Rosas D, Makris N, Dale A, Dickerson B, Fischl B (2006) Reliability of MRI-derived measurements of human cerebral cortical thickness: the effects of field strength, scanner upgrade and manufacturer. Neuroimage 32:180–194
Heinzel S, Haeussinger FB, Hahn T, Ehlis AC, Plichta MM, Fallgatter AJ (2013) Variability of (functional) hemodynamics as measured with simultaneous fNIRS and fMRI during intertemporal choice. NeuroImage 71:125–134
Jang KE, Tak S, Jung J, Jang J, Jeong Y, Ye JC (2009) Wavelet minimum description length detrending for near-infrared spectroscopy. J Biomed Opt 14:034004
Koskenkorva P, Khyuppenen J, Niskanen E, Könönen M, Bendel P, Mervaala E, Lehesjoki AE, Kälviäinen R, Vanninen R (2009) Motor cortex and thalamic atrophy in Unverricht–Lundborg disease: voxel-based morphometric study. Neurology 73(8):606–611
Koskenkorva P, Niskanen E, Hyppönen J, Könönen M, Mervaala E, Soininen H, Kälviäinen R, Vanninen R (2012) Sensorimotor, visual, and auditory cortical atrophy in Unverricht–Lundborg disease mapped with cortical thickness analysis. AJNR Am J Neuroradiol 33(5):878–883
Leff DR, Orihuela-Espina F, Elwell CE, Athanasiou T, Delpy DT, Darzi AW, Yang GZ (2011) Assessment of the cerebral cortex during motor task behaviours in adults: a systematic review of functional near infrared spectroscopy (fNIRS) studies. Neuroimage 54(4):2922–2936
Logothetis NK, Pauls J, Augath M, Trinath T, Oeltermann A (2001) Neurophysiological investigation of the basis of the fMRI signal. Nature 412(6843):150–157
Magaudda A, Gelisse P, Genton P (2004) Antimyoclonic effect of levetiracetam in 13 patients with Unverricht–Lundborg disease: clinical observation. Epilepsia 45(6):678–681
Manganotti P, Tamburin S, Zanette G, Fiaschi A (2001) Hyperexcitable cortical responses in progressive myoclonic epilepsies: a TMS study. Neurology 57:1793–1799
Panzica F, Canafoglia L, Franceschetti S, Binelli S, Ciano C, Visani E, Avanzini G (2003) Movement-activated myoclonus in genetically defined progressive myoclonic epilepsies: EEG–EMG relationship estimated using autoregressive models. Clin Neurophysiol 114(6):1041–1052
Panzica F, Canafoglia L, Franceschetti S (2014) EEG–EMG information flow in movement-activated myoclonus in patients with Unverricht–Lundborg disease. Clin Neurophysiol 125(9):1803–1808
Perrin F, Pernier J, Bertrand O, Echallier JF (1989) Spherical splines for scalp potential and current density mapping. Electroencephalogr Clin Neurophysiol 72:184–187
Pfurtscheller G, Lopes da Silva FH (1999) EEG/EMG synchronization and desynchronization: basic principles. Clin Neurophysiol 110:1842–1857
Segonne F, Pacheco J, Fischl B (2007) Geometrically accurate topology-correction of cortical surfaces using nonseparating loops. IEEE Trans Med Imaging 26:518–529
Shahwan A, Farrell M, Delanty N (2005) Progressive myoclonic epilepsies: a review of genetic and therapeutic aspects. Lancet Neurol 4:239–248
Shibasaki H, Hallet M (2005) Electrophysiological studies of myoclonus. Muscle Nerve 31:157–174
Steinbrink J, Villringer A, Kempf F, Haux D, Boden S, Obrig H (2006) Illuminating the BOLD signal: combined fMRI–fNIRS studies. Magn Reson Imaging 24(4):495–505
Strangman G, Culver JP, Thompson JH, Boas DA (2002) A quantitative comparison of simultaneous BOLD fMRI and NIRS recordings during functional brain activation. NeuroImage 17:719–731
Torricelli A, Contini D, Pifferi A, Caffini M, Re R, Zucchelli L, Spinelli L (2014) Time domain functional NIRS imaging for human brain mapping. NeuroImage 85:28–50
Virtaneva K, D’Amato E, Miao J, Koskiniemi M, Norio R, Avanzini G, Franceschetti S, Michelucci R, Tassinari CA, Omer S, Pennacchio LA, Myers RM, Dieguez-Lucena JL, Krahe R, de la Chapelle A, Lehesjoki AE (1997) Unstable minisatellite expansion causing recessively inherited myoclonus epilepsy, EPM1. Nat Genet 15(4):393–396
Visani E, Agazzi P, Canafoglia L, Panzica F, Ciano C, Scaioli V, Avanzini G, Franceschetti S (2006) Movement-related desynchronization–synchronization (ERD/ERS) in patients with Unverricht–Lundborg disease. Neuroimage 33(1):161–168
Visani E, Minati L, Canafoglia L, Gilioli I, Granvillano A, Varotto G, Aquino D, Fazio P, Bruzzone MG, Franceschetti S, Panzica F (2011) Abnormal ERD/ERS but unaffected BOLD response in patients with Unverricht–Lundborg disease during index extension: a simultaneous EEG–fMRI study. Brain Topogr 24(1):65–77
Ye JC, Tak S, Jang KE, Jung J, Jang J (2009) NIRS–SPM: statistical parametric mapping for near-infrared spectroscopy. Neuroimage 44(2):428–447 Epub 2008 Sep 12
Acknowledgments
This study received funding from the European Community’s Seventh Framework Programme (FP7/2007-2013) under Grant agreement HEALTH-F5-2008-201076 (nEUROPt). The authors are grateful to Elena Schiaffi and Alice Granvillano for their outstanding technical assistance during EEG-TD-fNIRS and EEG-fMRI data acquisition.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Visani, E., Canafoglia, L., Gilioli, I. et al. Hemodynamic and EEG Time-Courses During Unilateral Hand Movement in Patients with Cortical Myoclonus. An EEG-fMRI and EEG-TD-fNIRS Study. Brain Topogr 28, 915–925 (2015). https://doi.org/10.1007/s10548-014-0402-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10548-014-0402-6