Abstract
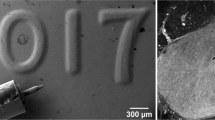
Precision medicine for inner-ear disease is hampered by the absence of a methodology to sample inner-ear fluid atraumatically. The round window membrane (RWM) is an attractive portal for accessing cochlear fluids as it heals spontaneously. In this study, we report on the development of a microneedle for perilymph sampling that minimizes the size of RWM perforation, facilitates quick aspiration, and provides precise volume control. Here, considering the mechanical anisotropy of the RWM and hydrodynamics through a microneedle, a 31G stainless steel pipe was machined into wedge-shaped design via electrical discharge machining. The sharpness of the needle was evaluated via a surface profilometer. Guinea pig RWM was penetrated in vitro, and 1 μL of perilymph was sampled and analyzed via UV–vis spectroscopy. The prototype wedge shaped needle was successfully fabricated with the tip curvature of 4.5 μm and the surface roughness of 3.66 μm in root mean square. The needle created oval perforation with minor and major diameter of 143 and 344 μm (n = 6). The sampling duration and standard deviation of aspirated volume were 3 s and 6.8 % respectively. The protein concentration was 1.74 mg/mL. The prototype needle facilitated precise perforation of RWMs and rapid aspiration of cochlear fluid with precise volume control. The needle design is promising and requires testing in human cadaveric temporal bone and further optimization to become clinically viable.








Similar content being viewed by others
References
E. Arrer, G. Oberascher, H.J. Gibitz, A map of cochlear perilymph protein based on high-resolution two-dimensional electrophoresis. Eur. Arch. Otorhinolaryngol. 247(5), 271–273 (1990)
A. Axelsson, O. Hallen, J.M. Miller, D.L. McPherson, Experimentally induced round window membrane lesions. Acta Otolaryngol. 84(1–2), 1–11 (1977)
D. Buckiová, S. Ranjan, T.A. Newman, A.H. Johnston, R. Sood, P.K.J. Kinnunen, J. Popelář, T. Chumak, J. Syka, Minimally invasive drug delivery to the cochlea through application of nanoparticles to the round window membrane. Nanomedicine 7(9), 1339–1354 (2012)
K. Gyo, Healing of experimentally produced round window membrane rupture. Acta Otolaryngol. 107(1–2), 85–89 (1989)
A. Hara, A.N. Salt, R. Thalmann, Perilymph composition in scala tympani of the cochlea: influence of cerebrospinal fluid. Hear. Res. 42(2–3), 265–271 (1989)
M. Igarashi, K. Ohashi, M. Ishii, Morphometric comparison of endolymphatic and perilymphatic spaces in human temporal bones. Acta Otolaryngol. 101(3–4), 161–164 (1986)
J. Jero, A.N. Mhatre, C.J. Tseng, R.E. Stern, D.E. Coling, J.A. Goldstein, K. Hong, Z. Wei Wen, A.T.M.S. Hoque, A.K. Lalwani, Cochlear gene delivery through an intact round window membrane in mouse. Hum. Gene Ther. 12(5), 539–548 (2001)
K. Lamm, Experimental defects of the round window membrane. HNO 40(10), 374–380 (1992)
K. Lamm, H. Lamm, C. Lamm, E. Lehnhardt, Microperforation and removal of the round window membrane. Short- and long-term study in animal experiments using electrocochleography and evoked response audiometry. HNO 36(3), 106–110 (1988)
E.O. Laurens-Thalen, H.P. Wit, J.M. Segenhout, F.W. Albers, Direct measurement flow resistance of cochlear aqueduct in guinea pigs. Acta Otolaryngol. 124(6), 670–674 (2004)
Layne, E. (1957). [73] Spectrophotometric and turbidimetric methods for measuring proteins. Methods in Enzymology, Academic Press. Volume 3: 447–454.
A.C. Lysaght, S.-Y. Kao, J.A. Paulo, S.N. Merchant, H. Steen, K.M. Stankovic, Proteome of human perilymph. J. Proteome Res. 10(9), 3845–3851 (2011)
K. Mizutari, M. Fujioka, M. Hosoya, N. Bramhall, H. Okano, H. Okano, A. Edge, Notch inhibition induces cochlear hair cell regeneration and recovery of hearing after acoustic trauma. Neuron 78(2), 403 (2013)
D.R. Paugh, S.A. Telian, M.J. Disher, Identification of perilymph proteins by two-dimensional gel electrophoresis. Otolaryngol. Head Neck Surg. 104(4), 517–525 (1991)
A.N. Salt, S.A. Hale, S.K. Plonkte, Perilymph sampling from the cochlear apex: a reliable method to obtain higher purity perilymph samples from scala tympani. J. Neurosci. Methods 153(1), 121–129 (2006)
F. Scheibe, H. Haupt, U. Hache, H.J. Gerhardt, H. Lauterbach, Protein concentration in the guinea-pig perilymph. Acta Otolaryngol. 79(1–2), 51–57 (1975)
H. Silverstein, A rapid protein test for acoustic neurinoma. Arch. Otolaryngol. 95(3), 202–204 (1972)
H. Silverstein, Labyrinthine tap as a diagnostic test for acoustic neurinoma. Otolaryngol Clin North Am 6(1), 229–244 (1973)
M. Sone, Pathological features of healing of a ruptured human round window membrane. ORL J. Otorhinolaryngol. Relat. Spec. 60(1), 55–57 (1998)
Stoscheck, C. M. (1990). [6] Quantitation of protein. Methods in Enzymology. P. D. Murray, Academic Press. Volume 182: 50–68.
E.V. Surovtseva, A.H. Johnston, W. Zhang, Y. Zhang, A. Kim, M. Murakoshi, H. Wada, T.A. Newman, J. Zou, I. Pyykkö, Prestin binding peptides as ligands for targeted polymersome mediated drug delivery to outer hair cells in the inner ear. Int. J. Pharm. 424(1–2), 121–127 (2012)
E.E. Swan, M. Peppi, Z. Chen, K.M. Green, J.E. Evans, M.J. McKenna, M.J. Mescher, S.G. Kujawa, W.F. Sewell, Proteomics analysis of perilymph and cerebrospinal fluid in mouse. Laryngoscope 119(5), 953–958 (2009)
I. Thalmann, T.H. Comegys, S.Z. Liu, Z. Ito, R. Thalmann, Protein profiles of perilymph and endolymph of the guinea pig. Hear. Res. 63(1–2), 37–42 (1992)
I. Thalmann, R.I. Kohut, J. Ryu, T.H. Comegys, M. Senarita, R. Thalmann, Protein profile of human perilymph: in search of markers for the diagnosis of perilymph fistula and other inner ear disease. Otolaryngol. Head Neck Surg. 111(3 Pt 1), 273–280 (1994)
W.L. Valk, H.P. Wit, F.W. Albers, Effect of acute inner ear pressure changes on low-level distortion product otoacoustic emissions in the guinea pig. Acta Otolaryngol. 124(8), 929–936 (2004)
H. Watanabe, J.W. Kysar, A.K. Lalwani, Microanatomic analysis of the round window membrane by white light interferometry and microcomputed tomography for mechanical amplification. Otol Neurotol 35(4), 672–678 (2014a)
H. Watanabe, J. Velmurugan, M.V. Mirkin, M.A. Svirsky, A.K. Lalwani, R.R. Llinas, Scanning electrochemical microscopy as a novel proximity sensor for atraumatic cochlear implant insertion. IEEE Trans. Biomed. Eng. 61(6), 1822–1832 (2014b)
Wazen, J. M., J. P. Stevens, H. Watanabe, J. W. Kysar and A. K. Lalwani (2015). Silver/silver chloride microneedles can detect penetration through the round window membrane. J Biomed Mater Res B Appl Biomater.
Acknowledgments
This research was funded by Coulter Translational Research Partnerships and American Otological Society. Professor Elizabeth S. Olson Ph.D. has been kindly providing her lab space as well as her knowledge. This research was supported by NIH National Institute on Deafness and Other Communication Disorders of the National Institutes of Health under award number R01DC014547.
Author information
Authors and Affiliations
Corresponding author
Additional information
Anil K. Lalwani and Jeffrey W. Kysar are senior authors.
Rights and permissions
About this article
Cite this article
Watanabe, H., Cardoso, L., Lalwani, A.K. et al. A dual wedge microneedle for sampling of perilymph solution via round window membrane. Biomed Microdevices 18, 24 (2016). https://doi.org/10.1007/s10544-016-0046-2
Published:
DOI: https://doi.org/10.1007/s10544-016-0046-2