Abstract
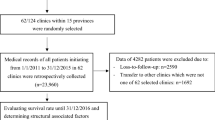
HIV care and treatment clinics (CTC) are important for management of HIV morbidity and mortality, and to reduce HIV transmission. Enrollment in HIV care and treatment clinics remains low in many developing countries. We followed up 632 newly diagnosed HIV patients aged 15 years and above from Magu District, Tanzania. Logistic regression was used to assess factors significantly associated with enrollment for CTC services. Kaplan–Meier plots and log-rank tests were used to evaluate differences in timing uptake of services. Among 632 participants, 214 (33.9%) were enrolled in CTC, and of those enrolled 120 (56.6%) took longer than 3 months to enroll. Those living in more rural villages were less likely to be enrolled than in the villages with semi-urban settings (OR 0.36; 95% CI 0.17–0.76). Moreover, those with age group 35–44 years and with age group 45 years and above were 2 times higher odds compared to those with age group 15–24 years, (OR 2.03; 95% CI 1.05–3.91) and (OR 2.69; 95% CI 1.40–5.18) respectively. Enrollment in the CTC in Tanzania is low. To increase uptake of antiretroviral therapy, it is critical to improve linkage between HIV testing and care services, and to rollout these services into the primary health facilities.


Similar content being viewed by others
References
USAID. Performance Evaluation of USAID Testing and Counseling Projects in Tanzania 2015. http://pdf.usaid.gov/pdf_docs/pa00jq5b.pdf/. Accessed 14 Nov 2017.
Tanzania HIV Impact Survey (THIS), 2017. https://phia.icap.columbia.edu/wpcontent/uploads/2017/11/Tanzania_SummarySheet_A4.English.v19.pdf/. Accessed 21 Aug 2018.
WHO. Consolidated strategic information guidelines for HIV in the health sector. 2015. http://apps.who.int/iris/bitstream/10665/164716/1/9789241508759_eng.pdf/. Accessed 27 April 2017.
UNAIDS. GLOBAL AIDS . 2016. Available from: global-AIDS-update-2016_en.pdf/. Accessed 14 Nov 2017.
UNAIDS DATA. 2017. http://www.unaids.org/sites/default/files/media_asset/20170720_Data_book_2017_en.pdf/. Accessed 25 Oct 2018.
WHO, UNICEF, UNAIDS. Global HIV/AIDS Response Progress Report 2011 [Internet]. 2011. Available from: http://www.unaids.org/sites/default/files/media_asset/20111130_UA_Report_en_1.pdf/. Accessed 14 Nov 2017.
Kishamawe C, Isingo R, Mtenga B, et al. Health & Demographic Surveillance System Profile Health & Demographic Surveillance System Profile: the Magu Health and Demographic Surveillance System (Magu HDSS). Int J Epidemiol. 2015;44:1–11.
Gerdts S, Wagenaar B, Micek M, et al. Linkage to HIV care and antiretroviral therapy by HIV testing service type in central Mozambique. J Acquir Immune Defic Syndr. 2014;66:e37–44.
Lubogo D, Ddamulira JB, Tweheyo R, Wamani H. Factors associated with access to HIV care services in eastern Uganda. BMC Fam Pract. 2015;16:1–9.
MacKellar DA, Williams D, Storer N, et al. Enrollment in HIV Care Two Years after HIV Diagnosis in the Kingdom of Swaziland: An Evaluation of a National Program of New Linkage Procedures. PLoS ONE. 2016;11(2):e0150086. https://doi.org/10.1371/journal.pone.0150086/.
Sanga ES, Lerebo W, Mushi AK, et al. Linkage into care among newly diagnosed HIV-positive individuals tested through outreach and facility- based HIV testing models in Mbeya, Tanzania. BMJ Open. 2017;7:1–10.
WHO. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. 2013. http://apps.who.int/iris/bitstream/10665/85321/1/9789241505727_eng.pdf/. Accessed 12 June 2017.
TACAIDS. National HIV and AIDS advocacy and Communication strategy (2013-2017). 2013. http://hivhealthclearinghouse.unesco.org/sites/default/files/resources/national_hiv_and_aids_advocacy_and_communication_strategy_2013_-_2017.pdf/. Accessed 21 Aug 2017.
WHO. Guideline on when to start Antiretroviral Therapy and on pre-exposure prophylaxis for HIV. 2015. http://apps.who.int/iris/bitstream/10665/186275/1/9789241509565_eng.pdf/. Accessed 14 June 2017.
Levira F, Agnarson AM, Masanja H, Zaba B, Ekström AM, Thorson A. Antiretroviral treatment coverage in a rural district in Tanzania—a modeling study using empirical data. BMC Public Health. 2015;15:1–12.
Nuwaha F, Kabatesi D, Whalen C. Factors influencing acceptability of Voluntary Counselling and Testing for HIV in Bushenyi district. Natl Inst Health. 2010;79(12):626–32.
Kidder DP, Bachanas P, Medley A, et al. HIV prevention in care and treatment settings: baseline risk behaviors among HIV patients in Kenya, Namibia, and Tanzania. PLoS ONE. 2013;8(2):1–9.
Naik R, Doherty T, Jackson D, et al. Linkage to care following a home-based HIV counselling and testing intervention in rural South Africa. Int AIDS Soc. 2015;18:1–9.
Chau C, Kirwan P, Brown A, Gill N, Delpech V. HIV diagnoses, late diagnoses and numbers accessing treatment and care. Public Health Engl. 2016;1–9.
Alvarez-uria G. Factors associated with delayed entry into HIV medical care after HIV diagnosis in a resource-limited setting: data from a cohort study in India. Dep Infect Dis. 2013;1:1–10.
Johnston SS, Juday T, Seekins ÞD, et al. Patterns and Correlates of Linkage to Appropriate HIV Care After HIV Diagnosis in the US Medicaid Population. Am Sex Transm Dis Assoc. 2013;40(1):18–25.
Nacher M, Adriouch L, Adenis A, et al. Short Report: risk Factors for Delayed Access to Specialized Care in French Guiana. Trop Med Hyg. 2011;84(5):806–7.
Idindili B, Jullu B, Mugusi F, Tanner M. A case-control study of factors associated with non-adherent to antiretroviral therapy among HIV infected people in Pwani Region, eastern Tanzania. Tanzan J Health Res. 2012;14(3):1–12. https://doi.org/10.4314/thrb.v14i3.6.
Rentsch CT, Kabudula CW, Catlett J, et al. Point-of-contact Interactive Record Linkage (PIRL): a software tool to prospectively link demographic surveillance and health facility data [version 2; referees: 2 approved]. Gates Open Res. 2018;1:8. https://doi.org/10.12688/gatesopenres.12751.2.
Acknowledgments
The analysis and work contributing to this paper was conducted as part of the MSc studies of SU in Kilimanjaro Christian Medical University College (KCMUCo). The Kisesa HDSS is a member of the INDEPTH Network and has received funding from the Global Fund [TNZ-405-GO4-H, TNZ-911-G14-S]. The work was supported by the Bill & Melinda Gates Foundation grants through the MeSH Consortium [OPP1120138], and the Search project [OPP1084472]. The clinical services in Kisesa are provided by the Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) through the Magu District Health Office. We acknowledge the help from staff and students of the Epidemiology and Biostatistics department at KCMUCo, and especially that of Dr Mwaka Kakolwa. We also acknowledge the work of data collection by personnel at in the National Institute for Medical Research (NIMR), Mwanza Centre and the assistance of personnel from London School of Hygiene and Tropical Medicine (LSHTM). We appreciate the contribution to this research by the study participants in Kisesa, who attended the serological survey in 2015.
Disclaimer
This study has been presented as an oral presentation at International Biometric Society (IBS)- Sub Sahara African Network (SUSAN) conference August 2017 and poster presented at Royal Society of Tropical Medicine and Hygiene (RSTM&H) East African Research September 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
Ethical approval to conduct this study was obtained from Kilimanjaro Christian Medical University College (KCMUCo) through certificate number is 990. Permission to use the data was granted by the TAZAMA project which had approval from the National Ethical Review Committee (NatREC) through certificate number NIMR/HQ/R.8c/Vol.1/307. Privacy and confidentiality were observed in the course of implementation and analysis through use of unique identifier rather than participants’ names.
Rights and permissions
About this article
Cite this article
Uvila, S.R., Mtuy, T.B., Urassa, M. et al. Enrollment in HIV Care and Treatment Clinic and Associated Factors Among HIV Diagnosed Patients in Magu District, Tanzania. AIDS Behav 23, 1032–1038 (2019). https://doi.org/10.1007/s10461-018-2338-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2338-4